Health Care Professionals' Awareness of Language Delay in Sohag, Upper Egypt
Received: 10-Mar-2017 / Accepted Date: 18-Apr-2017 / Published Date: 24-Apr-2017 DOI: 10.4172/2472-5005.1000125
Abstract
Aims: To investigate the health care professionals' awareness of Delayed Language Development (DLD) in children in Sohag, Upper Egypt.
Methods: A cross sectional survey of medical doctors, dentists, pharmacists, and paramedical staff employed in three public health care facilities were asked to fill in a questionnaire. The questionnaire addresses knowledge and attitudes towards DLD.
Results: The main source of knowledge was relatives and acquaintances. Most of the participants advised a parent of a two-year-old child with DLD not to wait and seek medical advice. They thought that the best management of DLD is language training.
Conclusion: This survey may provide insights that can raise awareness among health care professionals and help in the treatment of children with DLD with greater competence. It also emphasizes the need for increasing education of future health care professionals through putting a course of speech pathology field in the curricula of medical schools which could prove to be particularly effective.
Keywords: Delayed language development; Awareness; Attitude; Questionnaire; Upper Egypt
Introduction
Children with language disorders have difficulty using spoken and/or written language at their expected developmental level [1]. Children with normal language development tend to acquire language skills in the general education classroom with no special instruction. However, students with language impairments may require additional assistance to maintain their functioning level in the general education classroom. Failure to acquire language in the early years could result in delay or disruption in the development of cognitive skills that interweave with linguistic ability. Such Children are documented to have trouble with verbal memory organization [2], mastery of Numeracy and literacy [3], and higher-order cognitive processing such as executive function and theory of mind [4-6].
Phoniatrics as a profession was introduced to the medical field in Cairo, Egypt dating back to 1973 [7] and in Sohag, Upper Egypt dating back to 1995. Lack of agreement among professionals and even the public at large, that the needs of people with communication disorders should be prioritized for funding, is one of the most important barriers that faced the profession [8]. In Egypt, Speech-language pathology is practiced exclusively by Phoniatricians and logopedists/speech-language pathologists. Phoniatricians are doctors who are holding a bachelor degree of medicine, followed by a master degree in Phoniatrics, and then possibly, an academic Doctoral Degree. They make the diagnosis, draw the plan of intervention, perform parts of the intervention program, educate and train personnel in the field, and conduct research. Logopedists are non-medical speech-language pathologists. They require an undergraduate degree in language, psychology and sociology, followed by a postgraduate 2 years training in Logopedics (Speech-Pathology) to earn a certified diploma. Logopedists share in the diagnostic procedures and formal testing, develop and perform the behavior re-adjustment therapeutic methods and collaborate in the research program [9].
In 2010, there were approximately 125 phoniatricians and 250 logopedists in Egypt. To reach the goal of one phoniatrician for every 100,000 inhabitants, 750 additional professionals are needed. To reach the goal of one logopedist for 20,000 inhabitants, 7,500 additional professionals are needed [8]. In 2015, there were 285 phoniatrians who officially registered in Egyptian Doctors Syndicate while there is no official census of the number of the logopedists. Phoniatricians and logopedics work in 12 university clinics all over the country, as well as hospitals of the ministry of health, hospitals of the national health insurance, and hospitals of the ministry of defense and police. The phoniatrician/logopedist team cooperates, in turn, with other related disciplines to form a wider team that serves the rehabilitation needs of people with communication disorders.
The phoniatric unit at Sohag university hospital receives a considerable number of belated cases of children with DLD as our caseloads contain high percentages of children aged 6-15 years. Their parents report that they were not aware of the specialty Moreover, the physicians such as pediatricians or otolaryngologists didn't refer them to the right specialist.
Practitioners play a vital role in promoting children’s communication development in early years, particularly for children from disadvantaged backgrounds [10]. It is widely agreed that the practice of clinicians is based on their education, knowledge and awareness. If there is "know-do" gap, it will lead to an ineffective use of resources and suboptimal provision of services, especially Egypt which faces greater limitation of resources.
New attitudes are learned in essentially the same way all new information is learned. While it is not possible to change beliefs with information alone, it is possible to shape attitudes with information that is convincingly presented and which creates cognitive dissonance. It is most effective to use relatively small amounts of information at strategic times to encourage the formation of desirable attitudes [11]. Hence, if awareness is raised, the attitude may change. Elman et al. [12] warned of limited public awareness of one of language disorders such as aphasia and said that "Without public awareness, a vicious cycle sets into play, there will be less funding for research, less money for services and, perhaps, most serious of all, less empathy and understanding for people with aphasia.”
Statistical levels of awareness and knowledge of speech-language pathology and of communication disorders such as DLD are currently unknown among health care professionals in Egypt, including Sohag. The aim of this study is to conduct a survey, the first of this type in the region, to explore and analyze the attitudes and knowledge among health professionals in Sohag. No Egyptian surveys were found collecting information about the health care professionals' awareness and knowledge of Delayed language Development and speech-language pathology services. Hence, this study investigates wide population of health professionals including medical doctors, pharmacists, paramedical staff (nurses and technicians).
This survey was conducted in Sohag city, Upper Egypt. Upper Egypt is a narrow strip of land on both sides of the Nile that extends from modern-day Aswan to the area south of modern-day Cairo. Sohag (so'hæ:g) lies on the western bank of the Nile on a fertile agricultural plain. It lies midway between Aswan and Cairo. There were a number of differences between Upper and Lower Egyptians in the ancient world. They spoke different dialects, and had different customs, needs and interests. Many differences and the tensions they create still exist in modern times [13].
Methods
A questionnaire was designed according to the recent methodological literature [14,15]. The questionnaire contained 2 sections. First section contained demographic data of participants. Different information was collected from the investigated group. Health care professionals were asked their age, sex, profession, specialty and degree while they were not asked their names or the name of affiliated institution.
The second section of questionnaire was composed of 8 closed-ended questions and one open-ended question addressing attitudes and knowledge of health care professionals. The questionnaire survey with closed-ended questions is one of the most common used tools for user information elicitation [16].
A pilot study was conducted using small group of health care professional (n=20) to study the responses, obtain feedback for further changes, and to ensure that the time to complete the survey is adequate. The wording, the order of the questions, or the range of answers on multiple-choice questions and the number of open-ended questions were modified and adjusted. The open-ended questions were decreased because of larger item non-response. It seems that respondents restricted themselves with apparent ease to the alternatives offered on the close-ended forms knowing that closed-ended questions had the disadvantage of the bias that may result from suggesting responses to individuals.
The questionnaire had undergone internal validation (face validity and content validity) by three professors in Phoniatric Unit at Sohag University Hospital (SUH). Fine adjustments to the questions were done to ensure the clarity, accuracy and to exclude ambivalence. Data were collected by face-to-face interview of 5-7 minutes duration. A copy of the survey used in this study is located in Appendix A.
A cross section survey of both male and female medical doctors, dentists, pharmacists, and paramedical staff (nurses and technicians) employed in three public health care facilities were asked to fill in a questionnaire. The ethical considerations were addressed. The study was approved by the Ethical Committee of faculty of medicine Sohag University, Egypt. All participants were given both written and oral information about the study. A written consent for participation was obtained from each participant. Statistical analysis was conducted using SPSS program (version 16). Descriptive statistics were done for continuous variables by mean, standard deviation (± SD). Pearson’s correlation used to assess the association between the different parametric data. For all tests a probability (P) value less than 0.05 was considered significant.
Results
Two hundred and fifty questionnaires were distributed (201 have returned; 80.4% response). Descriptive statistics were computed for individual survey items pertaining to the characteristics of the participants (Table 1).
| Characteristics | Summary statistics No. (%) |
|---|---|
| Age | |
| Mean (SD) | 29.25 (6.78) |
| Median (range) | 28 (18-59) |
| Age | |
| <25 | 36 (17.91) |
| 25-35 | 141 (70.15) |
| >35 | 24 (11.94) |
| Occupation | |
| Paramedical | 99 (49.25) |
| Physician | 89 (44.28) |
| Pharmacist | 13 (6.47) |
| Degree Physicians | |
| General Practitioner | 12 (13.04) |
| Resident | 26 (28.26) |
| Master | 35 (38.04) |
| Ph.D. | 19 (20.65) |
| Paramedical | |
| Bachelor degree | 99 (100) |
| Pharmacist | |
| Bachelor degree | 13 (100) |
Table 1: Characteristics of the participants.
Respondents were asked to indicate their source of knowledge about delayed language development. The main source of knowledge was from relatives and acquaintances (n=65; 39.63%) while the internet and media show the lowest percentage (n=15; 9.15%) (Table 2).
| Q2: If yes, what is the source of your knowledge about Delayed Language Development disease in children | |
|---|---|
| No (%) | |
| A) Education | 30 (18.20) |
| B) The internet | 15 (9.15) |
| C) Media | 12 (7.32) |
| D) Relatives and acquaintances | 65 (39.63) |
| E) Others | 10 (6.10) |
| F) Combined | 32 (19.51) |
Table 2: Responses to Q2.
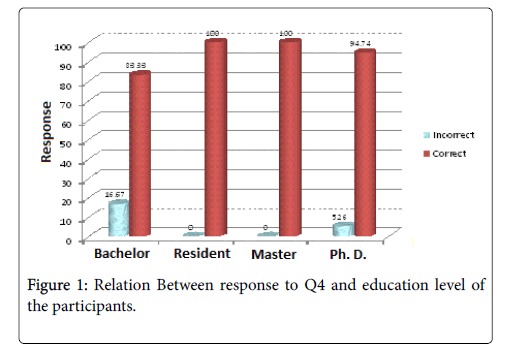
Respondents were asked to advise a parent of a 2 years old child with language delay. Most of the respondents (87.56%) advised them to seek medical advice. Almost all the respondents (n=174, 98.86%) advised to consult a specialist. Age didn't affect the knowledge of health care professionals in Q4. On the other hand, Occupation and Education level did differ significantly (p value=0.008, 0.03 respectively) (Tables 3 and 4 and Figure 1).
| Question 4 (Q4): The specialist for language delay is | |
|---|---|
| N (%) | |
| A)Pediatricians | 0(0) |
| B)Neurologist | 0 (0) |
| C)Otolaryngologist | 2 (1) |
| D)Phoniatrician | 196 (97.5) |
| E)combined | 3 (1.49) |
Table 3: Responses to Q4.
| Factors | Response to Q4 | P value | |
|---|---|---|---|
| Incorrect N (%) | Correct N (%) | ||
| Age | |||
| <35 | 1 (2.78) | 35 (97.22) | 0.83 |
| 35-50 | 3 (2.13) | 138 (97.97) | |
| >50 | 1 (4.17) | 23 (95.83) | |
| Occupation | |||
| Paramedical | 2 (2.02) | 97 (97.98) | 0.008 |
| Physician | 1 (1.12) | 88 (98.88) | |
| Pharmacist | 2 (15.38) | 11 (84.62) | |
| Degree | |||
| Bachelor | 2 (16.67) | 10 (83.33) | 0.03 |
| Resident | 0 (0) | 26 (100) | |
| Master | 0 (0) | 35 (100) | |
| Ph.D. | 1 (5.26) | 18 (94.74) | |
Table 4: Relation between responses to Q4 and participants’ characteristics. Q4: who is the specialist for language delay?
Asking the respondents about the best treatment of language delay in children, a large percentage of them (n=176, 87.56%) reported language therapy while some of the respondents thought that kindergartens where children need to interact with other children of the same age are the proper treatment for DLD (n=9; 4.48%) (Table 5). Results indicated no significant differences in terms of age (p value=0.34), occupation (p value=0.84) or education level (p value=0.62).
| Question (Q5): In your point of view, what is the best treatment for Delayed Language Development disease in children? | |
|---|---|
| N (%) | |
| A) Medication | 2 (1) |
| B)Surgery | 0 (0) |
| C)speech and language therapy | 176 (87.56) |
| D)others | 9 (4.48) |
| E)Combined | 7 (3.48) |
| F)Don’t know | 7 (3.48) |
Table 5: Responses to Q5.
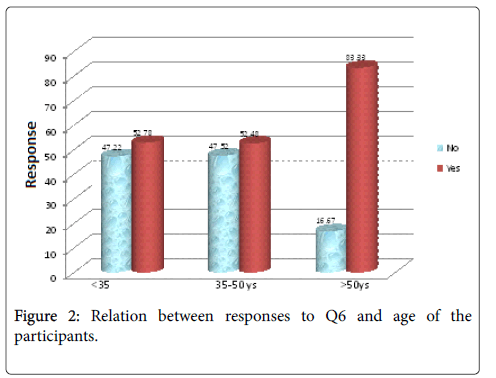
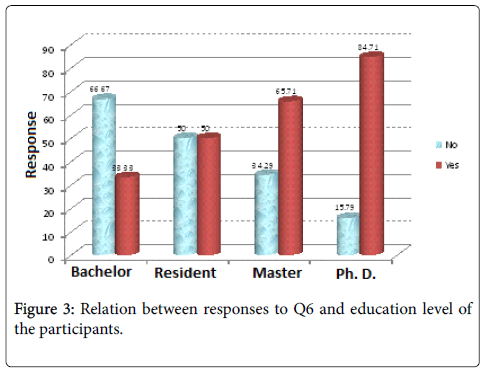
Respondents were asked if they know the difference between a phoniatrican and a logopedist, more than half of them (n=113, 56.22%) acknowledged the difference. Age and scientific degree showed significant difference (p value=0.02, 0.02 respectively) (Figures 2 and 3). On the other hand, results indicated no significant differences in terms of Occupation (p value=0.46).
Relationship between participants’ knowledge of language delay in Q1 was investigated in relation to their knowledge about the difference between phoniatricians and logopedics in Q6 and found significant difference between both variables (p value=0.004) (Table 6).
| Factors | Response to Q6 | P value | ||
|---|---|---|---|---|
| No N (%) | Yes N (%) | |||
| Age | ||||
| <35 | 17 (47.22) | 19 (52.78) | 0.02 | |
| 35-50 | 67 (47.52) | 74 (52.48) | ||
| >50 | 4 (16.67) | 20 (83.33) | ||
| Occupation | ||||
| Paramedical | 46 (46.46) | 53 (53.54) | 0.46 | |
| Physician | 35 (39.33) | 54 (60.67) | ||
| Pharmacist | 7 (53.85) | 6 (46.15) | ||
| Degree | ||||
| Bachelor | 8 (66.67) | 4 (33.33) | 0.02 | |
| Resident | 13 (50.00) | 13 (50.00) | ||
| Master | 12 (34.29) | 23 (65.71) | ||
| Ph.D. | 3 (15.79) | 16 (84.71) | ||
| Q1 | ||||
| No | 24 (64.86) | 13 (35.14) | 0.004 | |
| Yes | 64 (39.02) | 100 (60.98) | ||
Table 6: Relation between responses to Q6 and participants' characteristics. Q1: Are you aware of Delayed Language Development (DLD) disorder in children? Q6: Do you know the difference between a Phoniatrician and Logopedist?
A large percentage of them (n=159, 79.10%) knew where phoniatricans work in their city (Table 7). Also they were asked if the society is aware of speech and language disorders, about half of the respondents (n=102, 50.75%) thought that the society is not aware. Age and occupation didn't show significant difference (p value=0.22, 0.34 respectively). Yet, the Education level showed significant difference (p value=0.02) as physicians carrying master degree (65.71%) thought that the society is aware of speech and language disorders. Relationship between participants’ knowledge of language delay in Q1 was investigated in relation to their opinion of the society awareness of language delay in children and found significant difference between both variables (p value=0.02) (Table 8).
| Factors | Response to Q7 | P value | |
|---|---|---|---|
| No N (%) | Yes N (%) | ||
| Age | |||
| 13 (36.11)23 (63.89)0.003 | |||
| 35-50 yrs | 29 (20.57) | 112 (79.43) | |
| >50 yrs | 0 (0) | 24 (100) | |
| Occupation | |||
| Paramedical | 28 (28.28) | 71 (71.72) | 0.03 |
| Physician | 13 (14.61) | 76 (85.39) | |
| Pharmacist | 1 (7.79) | 12 (92.31) | |
| Degree | |||
| Bachelor | 4 (33.33) | 8 (66.67) | 0.1 |
| Resident | 5 (19.23) | 21 (80.77) | |
| Master | 3 (8.57) | 32 (91.43) | |
| Ph.D. | 1 (5.26) | 18 (94.74) | |
Table 7: Relation between responses to Q7 and participants' characteristics. Q7: Do you know where do phoniatricians work in your city town?
| Factors | Response to Q8 | P value | |
|---|---|---|---|
| No N (%) | Yes N (%) | ||
| Age | |||
| <35 | 23 (63.89) | 13 (36.11) | 0.22 |
| 35-50 | 68 (48.23) | 73 (51.77) | |
| >50 | 11 (45.83) | 13 (54.17) | |
| Occupation | |||
| Paramedical | 55 (66.5) | 44 (44.44) | 0.34 |
| Physician | 42 (47.19) | 47 (52.81) | |
| Pharmacist | 5 (38.47) | 8 (61.54) | |
| Degree | |||
| Bachelor | 10 (83.33) | 2 (16.67) | 0.02 |
| Resident | 14 (53.85) | 12 (46.15) | |
| Master | 12 (34.29) | 23 (65.71) | |
| Ph.D. | 7 (36.84) | 12 (63.16) | |
| Q1 | |||
| No | 25 (67.57) | 12 (32.43) | 0.02 |
| Yes | 77 (46.95) | 87 (53.05) | |
Table 8: Relation between responses to Q8 and participants' characteristics. Q1: Are you aware of Delayed Language Development (DLD) disorder in children? Q8: Do you think the society is aware of speech and language disorders?
Discussion
This study revealed good knowledge among health care professionals when they were asked who the specialist for language delay is. The highest level of awareness was among Physicians. Moreover, education level and scientific degree played an important role in the level of knowledge and awareness as all residents and physicians with master degree has higher knowledge than physicians with bachelor degree. This study is opposite to a survey which was done 35 years ago by Lass et al. [17]. The survey explored the knowledge and opinions of three groups of potential referrers concerning Speech-Language Pathology (SLP). The responses of 51 physicians, 74 dentists and 77 teachers revealed shortcomings in the professionals’ knowledge and use of SLP services. The difference between the two studies can be reasoned to the onslaught of information technology and the use of different and varied communication means in 21th century which make individuals more knowledgeable. Yet, Sullivan and Cleave 18 conducted a survey in 2003 and concluded that there are some critical gaps in the knowledge of the field among vital members of an interdisciplinary medical team as they were unaware of the services a SLP can provide patients.
Surprisingly, the main source of knowledge (38.63%) was relatives and acquaintances. These sources can be under informed about crucial issues, such as matters of brain plasticity connected to the risk of linguistic deprivation, and delay or disruption in the development of cognitive skills interwoven with linguistic ability. Although education is expected to be the foundation of acquisition of formal knowledge, small percentage of health care professionals gained their knowledge from education. Only very few universities in Egypt teach speech pathology in the curricula of medical schools. In Sohag, speech pathology is not taught for the future health care professionals. Sullivan and Cleave [18] as well found that the medical profession has given their students very little exposure to the field of SLP. We should turn our attention and care to what is taught about speech pathology in general and language disorders in specific to the medical and paramedical students in their study years.
The internet and media show the lowest percentage of sources of knowledge. This reflects low media presentation of speech-language pathology services as also noted by Hughes [19]. Therefore, raising awareness about DLD and speech pathology services through the internet and the media should be encouraged taking into consideration that the acceptance of new attitude depends on who is presenting the knowledge, how it is presented, how the person is perceived, the credibility of the communicator, and the conditions by which the knowledge was received.
Most of the participants believe that the earlier the consultation and seeking medical advice (age of two) the better. Early intervention is essential for children who have impairments that would limit the normal development of the physical, cognitive, emotional, and social and communication aspects in a child’s life. The goal of early intervention is to preclude or limit the physical, cognitive, emotional, and other restrictions of young children with biological or environmental risk factors [20]. The American Academy of Pediatrics (AAP) recommends that developmental surveillance, which is the process of recognizing children who might be at risk for developmental delays, be incorporated at every well-child preventive care visit. This surveillance should include asking about parents' concerns, obtaining a developmental history, making observations of the child, identifying risk and protective factors, and documenting the findings. Any concerns should be addressed promptly with developmental screening tests, i.e., standardized tools to identify and refine any risk or concern that has been noticed. In addition, all children should be screened using a standardized test during well-child visits at 9, 18, and 24 or 30 months [21]. If a potential developmental problem is noted on the screening test, further developmental and medical evaluation needs to follow. The more detailed evaluation will show whether the child has a developmental disorder or delay and needs treatment, including early developmental intervention services. Accurately identifying a developmental disorder and understanding its underlying causes are important for treatment planning, from medical treatment and intervention services for the child to genetic counseling for the child’s parents. Screening tools do not provide conclusive evidence of developmental delays and do not result in diagnoses. A positive screening result should be followed by a thorough assessment. Early identification of developmental disorders is critical to the well-being of children and their families. They are designed to help identify children who might have developmental delays. They can be specific to a disorder (for example, autism), an area (for example, cognitive development, language, or gross motor skills), or they can be general, encompassing multiple areas of concern. They can help parents and health care professionals talk about the child’s development in a systematic way. Systematic communication can help reveal parents’ concerns, help parent and health care professional observe the child’s development, and help parents become more aware of how children develop. Such tools can also be time-saving and cost-efficient in clinical practice settings [22-24]. Total cost of routine family psychosocial screening for children up to age 3 was estimated at about $2.00 per visit [25]. There are few screening tests for developmental disorders in Egypt but unfortunately DLD is not included. Hence, we can depend on health care professionals in promoting children’s developmental health while developing screening tests for DLD.
Some health care professionals thought that kindergartens where children need to interact with other children of the same age are the proper treatment for DLD. This indicates low awareness level of health care professionals. The best referral of children with language delay when most of health care professionals are aware of this problem as they are able to direct parents appropriately. Hines, Hugerford and Tomera [26] noted that the level of consistency between attitudes and behavior is affected by a person’s knowledge and awareness.
Not all health care professionals (56.22%) knew the difference between a Phoniatrician (medical speech-language pathologist) and a logopedist (nonmedical speech-language pathologist). The highest level of knowledge in this point was among older health care professionals and with the higher education level. The phoniatrician/ logopedist team cooperates, in turn, with other related disciplines to form a wider team that serves the rehabilitation needs of persons with communicative disorders. Phoniatricians in our community should pursue their efforts to increase the awareness and education of health care professionals of the qualifications of specialists who work in the field of speech-language pathology. It is also important for them to know that sometimes teachers, special education specialists and people who have only attended brief courses or workshops in speech therapy practice speech therapy services with no legal consequences in our community. Understanding that some services provided from unprofessional not certified trainers help to clarify the notion that they harm children, giving parents false hope of treatment and progress and decreasing children opportunities as they get older. It is imperative for health care professionals especially doctors to update their knowledge base and practice to reflect current standards of care.
Half of health care professionals thought that the society is not aware of speech and language disorders and suggested the need to raise awareness through educational websites, movies, television programs, flyers in hospitals and public institutes and education of parents about language and speech disorders through parent meetings in schools and kindergartens or in health care units at time of their child's vaccination. Also, medical convoys were noted to reach out to people in both rural and urban communities. Yet, there may be obstacles that impact previously mentioned public awareness – raising strategies such as a clear vision of the desired goals and objectives and poor funding of the government and organizations.
Moreover, measures should be initiated to improve awareness and education of health care professional and ensure accurate knowledge and clinical practice. Active involvement of the teaching faculty has an important role in teaching and inculcating appropriate practices through periodic educational courses. This can help to generate a well-rounded health care professional who is willing to learn new information. We also need to frequently assess their knowledge and attitude towards language delay and other speech-language disorders and services.
Conclusion
This survey may provide insights that can raise awareness among health care professionals and help in the treatment of children with DLD with greater competence. It also emphasizes the need for increasing education of future health care professionals through putting a course of speech pathology field in the curricula of medical schools which could prove to be particularly effective.
Conflict of Interests
The author declared no conflict of interest.
References
- Overby M, Carrell T, Bernthal J (2007) Teachers’ perceptions of students with speech sound disorders: A quantitative and qualitative analysis.Lang Speech Hear Serv Sch 38: 327-341.
- Rönnberg J (2003) Working memory, neuroscience, and language. In Marschark& Spencer, eds. Evidence from deaf and hard-of-hearing individuals. Oxford: Oxford UniPress 1: 478-489.
- MacSweeney M (1998) Cognition and deafness. In: Gregory S, et al. (eds) Issues in deaf education. David Fulton, London.
- Courtin C (2000) The impact of sign language on the cognitive development of deaf children: The case of theories of mind. J Deaf Stud Deaf Educ 5: 266-276.
- Courtin C (2010) A critical period for the acquisition of the theory of mind? Clues from home signers. In: Mathur G, Napoli DJ (eds) Deaf around the world: The impact of language. Oxford: Oxford University Press.
- Figueras B, Edwards L, Langdon D (2008) Executive function and language in deaf children. J Deaf Stud Deaf Educ 13: 362-377.
- Kotby MN (1973) Phoniatrics: A specialty in clinical medical practice. Ain Shams Med J 24: 347-354.
- Kotby MN, El-Sady S, Hegazi M (2010) Thirty Five Years of Care of Child Language in Egypt. Top Lang Disorders, 30: 84-91.
- (2010) Revised IALP Education Guidelines (September 1, 2009) IALP Guidelines for initial Education in Speech- Language Pathology. Folia Phoniatr Logop 62: 210-216.
- Sylva K, Melhuish E, Sammons P, Siraj-Blatchford I, Taggart B (2004) The Effective Provision of Pre-school Education (EPPE) Project: Findings from pre-school to end of key stage 1. Institute of Education: Department for Education and Skills.
- Johnston JH (2011) Shaping Beliefs and Attitude: A Handbook, Model and Plan. Tampa FL.
- Elman R, Ogar J, Elman S (2000) Aphasia: Awareness, advocacy, and activism. Aphasiology 14: 455 -459.
- Richardson D (2003) The Rough Guide to Egypt. London. Rough guides. ISBN 1-84353-050-3.
- Boynton PM, Greenhalgh T (2004) Selecting, designing, and developing your questionnaire. BMJ 328:1312-1315.
- Richardson J (2005) Design and conduct a survey. ComplTher Med, 13:47-53.
- Sakai T (2004) Questionnaire design, Marketing Research and Statistical Analysis. DrSmart Press, Taipei.
- Lass NJ, Pilson GS, Wilson KG, Cipoletti MK (1982) A survey of professionals' knowledge and awareness of speech-language pathology and audiology. Communique24-36.
- Sullivan A, Cleave P (2003) Knowledge of the roles of speech language pathologists by students in other health care programs. J Speech Lang PatholAudiol 27: 98-107.
- Hughes L (2007). Speech and language therapy and its presentation in the media: The views of journalists and students. (MSc dissertation). Retrieved from ProQuest Dissertations and Theses. (Accession UMI Number: U594165).
- Blackman JA (2002) Early intervention: A global perspective. Inf Young Children 15: 11-19.
- American Academy of Pediatrics (2006) Identifying Infants and Young Children with Developmental Disorders in the Medical Home: An Algorithm for Developmental Surveillance and Screening. Pediatrics 118:405-420.
- Regalado M, Halfon N (2001) Primary care services promoting optimal child development from birth to age 3 years. Arch PediatrAdolesc Med, 155:1311-1322.
- Skellern C, Rogers Y, O’Calaghan M (2001) A parent-completed developmental questionnaire: follow up of ex-premature infants. J Paediatr Child Health 37:125-129.
- Glascoe FP (2003) Parents’ evaluation of developmental status: how well do parents’ concerns identify children with behavioral and emotional problems? ClinPediatr (Phila) 42:133-138.
- Glascoe FP, Robertshaw NS, Woods SK (2010) Professionals' Manual, 3rd Edition: Developmental Milestones a Tool for Surveillance and Screening.PEDStest.com, LLC, Nashville, Tennessee.
- Hines J, Hugerford H, Tomera A (1986) Analysis and synthesis ofresearch on responsible environmental behavior. Journal Appl Soc Psycho, 22: 657-676.
Citation: Mostafa E (2017) Health Care Professionals' Awareness of Language Delay in Sohag, Upper Egypt. J Speech Pathol Ther 2:125. DOI: 10.4172/2472-5005.1000125
Copyright: © 2017 Mostafa E. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5150
- [From(publication date): 0-2017 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 4269
- PDF downloads: 881