hCG Testing to Determine Outcome after Medical Abortion: A Review
Received: 27-Jan-2019 / Accepted Date: 10-Apr-2019 / Published Date: 17-Apr-2019
Abstract
Introduction: The challenge in medical abortion is to reliably determine success of treatment within a short time interval, with the aim of improving evaluation of medical abortion outcomes. This can be done clinically using ultrasound (US) and/or hCG testing (urine human chorionic gonadotropin). The systematic use of US may lead to unnecessary surgical intervention and may be a barrier to the use of medical abortion when US is not accessible. Furthermore, US cannot be used in case of very early medical abortion with no confirmed intrauterine pregnancy at initiation of treatment. Serum hCG is highly reliable to judge on-going pregnancy and levels detected in urine correlate with serum levels. Self-assessment of the urine hCG test has proven to be effective and highly acceptable to women. The aim of this review is to describe the use of hCG testing for medical abortion outcomes.
Methods: An extensive literature search was performed using MedLine, with keywords “hCG” AND “abortion” and “abortion” AND “follow-up”, to identify publications in English from 2003 to 2016. A total of 910 references were found, out of which 35 including information on hCG testing were considered.
Results: This review confirms that low-sensitivity urine hCG tests are highly reliable for determining medical abortion outcomes up to 63 days gestation. Their high sensitivity and specificity allow for shortening the time interval to accurately determine success of treatment.
Conclusion: Self-assessment using a low-sensitivity urine hCG test is effective in identifying on-going pregnancy while increasing women’s autonomy by reducing in-clinic visits.
Keywords: hCG; Medical abortion follow-up; Low-sensitivity urine hCG test
Introduction
Medical abortion using mifepristone in combination with misoprostol is known to be effective and safe [1]. But routine followup is necessary to assess treatment outcomes and to exclude on-going pregnancy [2]. Moreover, a follow-up visit is legally mandatory in many countries.
To facilitate follow-up, remote techniques using urinary Human Chorionic Gonadotropin (hCG) testing have been developed in recent years.
The use of Ultrasonography (US) at follow-up to assess medical abortion outcome is rapid and reliable if done by a qualified provider and provided the pregnancy has been visualised on ultrasound prior to treatment. For women, the disadvantage of US is an additional clinic visit, leading to reduced acceptability of medical abortion. This approach may also add costs for the woman or the health care provider. In addition, ultrasound findings alone, such as diameter of the uterine cavity, do not indicate a need for surgical intervention and interpretation depends on provider experience [3-5]. Therefore, other ways to reliably diagnose success or failure of medical abortion were searched and are currently under investigation.
The follow-up visit is often the time for contraception counselling. However, this should take place before initiating medical abortion, because women can ovulate 8-14 days after treatment. If they want to prevent subsequent unwanted pregnancy, they should start reliable contraception immediately after medical abortion, before the followup visit [6,7]. Postponing contraception provision increases the risk of subsequent unplanned pregnancy. All methods of contraception, including Intra-Uterine Devices (IUDs) and hormonal , can be initiated immediately after medical abortion [1]. To prevent unnecessary visits to the clinic, implants should be placed at the time of mifepristone treatment to allow a quick start for this reversible contraceptive method [8].
In addition, treatment of potential medical abortion complications should not be delayed until a scheduled follow-up. Some women with an on-going pregnancy after medical abortion may not feel any pregnancy-related symptoms and therefore would miss an on-going pregnancy without using US or hCG [9]. This means that determining the outcome of medical abortion based on self-perception or by history-taking is inadequate [9]. A diagnostic tool like hCG is needed to reliably diagnose medical abortion outcomes, especially when women do not attend follow-up visits.
Using serum hCG testing to diagnose outcome is highly reliable but adds an invasive blood test and requires an extra visit. Urinary hCG testing has therefore been proposed as a more practical alternative, especially with newly developed low-sensitivity tests that give a positive result above a threshold of 500-1000 U/L. No comprehensive information on that subject, including the more recent techniques, is available.
This systematic review examined the evidence regarding serum and urine hCG testing for determining medical abortion outcome and how these tests can be part of follow-up management of medical abortion up to 63 days of gestation.
Method and Materials
An extensive literature search was performed using MedLine, with key words “hCG” AND “abortion” and “abortion” AND “follow-up”, to identify publications in English from 2003 to 2016 that provided information on serum and urinary hCG testing up to 63 days medical abortion and during follow-up. All articles with an English abstract were reviewed. Titles and abstracts were used to identify studies related to gestations up to 63 days and information regarding gestations above 9 weeks was excluded. In addition to medical abortion studies, studies describing hCG changes during pregnancy and after the end of pregnancy, including causes other than medical abortion, were included. A total of 910 references were found, of which 35 clearly fit the topic and were included. These papers provided information regarding hCG course during pregnancy and/or hCG testing for medical abortion follow-up (Table 1).
| Reference | Study | Objective | Country | Date | Medical Abortion | n | Test | Pre-Abortion Test | Post-Abortion Test | Assessment | Results |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Barnhart et al. [12] | Extraction of clinical database data | To estimate a standard curve of serum hCG decline characterizing spontaneous abortion | USA | 1990-1999 | Pregnant women | 710 | - | - | - | - | Rate of decline ranged=21% to 35% at 2 days and 60% to 84% at 7 days, depending on initial hCG value. |
| Behnamfar et al. [18] | Prospective | To compare usefulness of serum beta-hCG and US | Iran | 2010 | <12WA Missed abortion or blighted ovum | 144 | Ultrasound (Medison 8000, vaginal probe 7.5 MHz) | X | X (2 weeks and 4 weeks after expulsion) | Complete abortion: US: No remained material or endometrial thickness <15 mm | Beta hCG as effective as US in confirming successful medically induced abortion (kappa agreement coefficient = 0.37, p<0.5) |
| Serum βhCG (Test ELISA, kit Immunotech, Beckman Counter Co, Czech Republic) | X | X (2 weeks and 4 weeks after expulsion) | Complete abortion: Negative or decline >80% | ||||||||
| Blum et al. [10] | Prospective, non-comparative | Assessment of a semi-quantitative home pregnancy test as a possible replacement for in-person follow-up | USA | March 2010-March 2011 | ≤ 63 DA | 490 | dBest® semi-quantitative urine hCG test, cutoffs of 25, 100, 500, 2000 and 10,000 mIU/mL | X | X Morning of follow-up visit, 1 week after MIF |
Ongoing pregnancy = follow-up hCG reading was the same or higher than the baseline result | 1 on-going pregnancy detected Sensitivity = 100% Specificity = 97% |
| Blum et al. [26] | Prospective, comparative, randomized | Accuracy, feasibility, and acceptability of 2 urine pregnancy test for determining early medical abortion outcomes at 3, 7, and 14 days after MIF | Vietnam | June 2013-Feb 2014 | ≤ 63 DA | MLPT: 300 HSPT: 300 |
MLPT (Multilevel Urine Pregnancy Test) = Semi quantitative test (dBest®) Vs High Sensitivity Pregnancy Test (HSPT) |
X | X 3, 7 and 14 days after MIF |
Clinic visit if decrease or increase of MLPT, if Unchanged wait and repeat test. HSPT= yes response= hcG > 25mIU/mL | 13 on-going pregnancies (7 MLPT, 6 HSPT), all detected Sensitivity=100% for both tests Specificity for MLPT=increases with time from 64 to 97% |
| Bracken et al. [34] | Prospective randomized | Effectiveness and feasibility of remote communication technologies to increase follow-up after early medical abortion | UK | Apr 2011-Feb 2012 | ≤ 63 DA | 999 | Clinic follow-up: Ultrasonography at 1 week + high-sensitivity urine pregnancy test (Clearview One Step, 25 mIU/mL) at 3 weeks Or Remote follow-up with low-sensitivity urine pregnancy test (LSUP) (NADEL hCG-2000, 2000 mIU/mL) + phone call or SMS or online questionnaire (standardized questionnaire) at 2 weeks |
US | X | - | FU completed: Clinic, 73% (HSUP + phone: 83%, came for US: 17%) vs. remote 69% Complete abortion at FUP: Clinic-based: 96.1% vs remote: 97.6% At FU, 1 ongoing pregnancy for remote FU group and 2 for clinic-based group |
| Cameron et al. [36 ] | Prospective | To evaluate telephone follow-up with a self-performed LSUP as an alternative to routine US | Scotland | May 2010-Feb 2011 | ≤ 63 DA | 476 with telephone FU/619 | LSU hCG assay (Baby check Duo, Quadratech Diagnostics, UK) and telephone follow-up | X | X | Positive test: >1000 IU | Telephone follow-up method failed to detect one on-going pregnancy Negative predictive value: 99.7%, positive predictive value: 5% |
| Cameron et al. [39] | Retrospective | Outcome of early medical abortion in women who choose self-assessment: LSUP test + signs/symptoms that mandate contacting the TOP service | UK | Apr 2012-Oct 2013 | ≤ 63 DA | 1726 | LSUP (Baby Duo, Quadratech diagnostics, UK, detection limit 1000 IU Human Chorionic Gonadotrophin) 2 weeks after treatment + telephone-initiated by women (positive test or clinical signs) | US | X (2 weeks after treatment) | Self-assessment by reading of LSUP and clinical signs | 96% chose self-assessment 2% unscheduled visits to service 11% telephoned 8 on-going pregnancies |
| Chen et al. [35] | Retrospective | Compare proportion lost to follow-up, successful abortion, and staff effort in women who choose office or telephone-based follow-up | USA | Aug 2012-Aug 2015 | ≤ 63 DA | 176 | US (n=105) 1 to 2 weeks after MIF Or Telephone at 1 week and 4 weeks+urine pregnancy test before 4 weeks (n=71) |
US | X X |
No difference in rate of loss to follow-up (4.8% for clinic vs 5.6% for phone) Medical abortion efficacy is 94.0% (office FU) and 92.5% (telephone follow-up) Two (1.2%) on-going pregnancies in office group |
|
| Clark et al. [15] | Retrospective record review | To demonstrate safety and efficacy of providing medication abortion in a primary care site without routine use of pre- and post-procedure transvaginal sonography | USA | Jan 2002-Feb 2004 | ≤ 9 weeks | 172 | hCG measurement, using Roche’s Elecsys 2010 system | US Serum hCG |
Serum hCG US only in specific cases |
Non pregnant: 0-10 mIU/mL, inconclusive: 10.1-24.9 mIU/mL, pregnant: >25 mIU/mL | Post-treatment/pre-treatment hCG ratio >0.2 in only 4/91 women with pre- and post-hCG, and with successful abortions 99% (95/96) of those receiving initial sonography had a successful and uneventful medication abortion treatment, while 98.2% (54/55) of those not receiving an initial sonography did so |
| Clark et al. [28] | Prospective | To evaluate women’s ability to assess abortion outcome without routine use of US | USA | June 2005-Feb 2007 | ≤ 63 DA | 4484 3054 with medical abortion |
Low-sensitivity urine pregnancy test (Immuno Pregnacol, Immunostics, Ocean, NJ) | X | X (7-14 days after MIF intake) | - | Patient-reported outcomes + urine test + non-sonographic clinical evaluation performed as well as sonography to identify all women with ongoing pregnancies at follow-up 20 ongoing pregnancies |
| Ultrasonography | X | X (7-14d after MIF intake) | - | ||||||||
| Data collected by the woman (expulsion, heavy bleeding, pregnancy symptoms) | X (between MIF intake and D7-14) | - | |||||||||
| Constant et al. [40] | Prospective | To establish whether women having a medical abortion could self-assess whether their abortion was complete using an automated, interactive questionnaire on their mobile phones | South Africa | Oct 2011-May 2012 | ≤ 63 DA | 469 | Standard of care (SOC): Visit 14 to 21 days after MIF, paper self-assessment + US ± HSUP SOC + m (mobile): SOC + mobile self-assessment on D10 |
US | 176/226 women with mobile phone assessment completed (78%) Good prediction of complete procedure (71% accurate for mobile assessment, 91% for paper assessment) Neither mobile nor paper self-assessments predicted all cases needing additional treatment at follow-up. 70 (SOC) vs 73% (SOC+mobile) of complete abortion assessed. One on-going pregnancy in each group |
||
| Dabash et al. [38] | Prospective open label | To assess the efficacy and acceptability of using a Multi-Level Pregnancy Test (MLPT) combined with telephone follow-up for medical abortion in Tunisia | Tunisia | March 2013-March 2014 | ≤ 70 DA | 404 | MLPT (dBest® (Ameritek, Seattle, Washington) semiquantitative pregnancy test) + clinic visit | - | - | MLPT: 5 hCG ranges: 25-99, 100-499, 500-1,999, 2000-9,999 and ≥ 10,000 mIU/mL. | Sensitivity of follow-up MLPT=100% among women ≤ 63 DA and 50.0% among women 64-70 DA Negative predictive value: 100% up to 63 DA, 96.9% for 64-70 DA 348/404 (86%) completed telephone follow-up, 343 completed MLPT at home before telephone follow-up 97.1 % of complete abortion 1.2% ongoing pregnancy |
| Dayananda et al. [19] | Prospective controlled randomized | To estimate whether follow-up with serum hCG results in fewer unplanned visits and interventions than follow-up with US | USA | May 2009-Apr 2010 | ≤ 63 DA | 376 | Serum hCG assay | X | X (in serum hCG arm 1-2 weeks after MIF) | 80% drop in pre-abortion to post-abortion serum hCG values US: Expulsion of the gestational sac endometrial thickness |
Similar number of unplanned interventions and visits in the both arms at the 2 and 4 week FUP. W2: Unplanned interventions and visits in 8.2% hCG arm vs 6.6% US arm (NS) W4: Surgical evacuation in 4.4% of US participants vs 1.4% hCG participants (NS) |
| US Tests 1-2 weeks after MIF Additional follow-up at 2 and 4 weeks |
X | X (in ultrasound arm 1-2 weeks after MIF) | |||||||||
| Dunn et al. [21] | Prospective, comparative, non-randomized | Adherence to follow-up and clinical outcomes between standard in-clinic and remote follow-up | Canada | Jul 2011-June 2013 | ≤ 49 DA | 129 | Clinic: US | X | X Day 15 (for standard in clinic FUP) | (80% drop in β-hCG from baseline) | No difference in non-adherence rates for follow-up visit: Remote (28%) and clinic (23%) Hospital visits: 3% (remote), 9% (clinic) Complete loss to follow-up: 6% (remote), 14% (clinic) 4% surgical aspiration rate in the two groups |
| Fiala et al. [3] | Prospective observational study | To compare the usefulness of hCG measurement and ultrasound examination before and after medical abortion in determining the outcome of treatment | Austria | Apr to Nov 1999 | ≤ 49 DA | 217 | Vaginal US Serum hCG |
US and serum hCG | US and serum hCG on D6 to D18 | hCG levels at follow-up were given as the percentage of the value before the treatment | In cases of successful abortion, hCG level dropped to a mean of 3% of the initial value before treatment [range: 1-44%] 2 ongoing pregnancies: Elevated hCG levels: 159% on D10, 7900% on D8 If 20% used as cut-off, positive predictive value for successful expulsion = 0.995 Rate of surgery: 1.8% |
| Godfrey et al. [24] | Prospective diagnostic test evaluative study | To assess Low-Sensitivity (LS) and High-Sensitivity (HS) urine pregnancy tests | USA | Apr 2002-June 2003 | ≤ 63 DA | 1080 | Low-sensitivity (LS) (dBest 2000 mIU/mL hCG Urine) and high-sensitivity (HS) urine tests (Sure-Vue 25mIU/mL) | - | D+7 and D+14 after MIF: 2 urine tests+US | - | 1st week post-abortion: Correct prediction of medical abortion outcome for 122 (14.8%) LS tests and 65 (7.9%) HS tests False negative, 0 for LS tests and 2 (0.2%) for HS tests False negative: 85.2% of LS tests and 91.8% of HS 2nd week post-abortion Correct prediction of medical abortion outcome for 238 (39.1%) LS tests and 205 (33.8%) HS tests. False negative: 1 (0.2%) LS tests and 2 (0.3%) HS tests False positive: 60.8% of LS tests and 65.8% of HS tests Best test to determine expulsion of the gestational sac = LS test 1 week after medical abortion |
| Grossman et al. [22] | Prospective, observational study | To compare diagnostic accuracy of a semi-quantitative urine test to serum β-hCG measurement for detecting ongoing pregnancy after medication abortion | Mexico | March to May 2005 | Normal pregnancy <8 weeks or follow-up of abortion (up to 3 weeks after) | 97 | Semi-quantitative urine pregnancy test (Orchid Biomedical Systems) | - | - | Urine test: Negative, hCG<1 000IU/L, hCG>1 000IU/L, indeterminate Serum test: Performed after urine test |
Sensitivity of the urine test to identify individuals with a serum β-hCG level >1000 IU/L was 88.6% (95% CI 74.6– 95.7%), and its specificity was 71.7% (95% CI 57.4–82.8%) |
| Grossman and Grindlay [9] | Meta-analysis of studies related to alternative follow-up modalities (search in Nov 2009) | Accuracy of alternative modalities in detecting ongoing pregnancy or retained gestational sac | - | - | - | 8 publications | Self-assessment (only clinical signs), 2 studies Clinical assessment, 3 studies Serum hCG Urinary pregnancy test (UPT), 3 studies |
- | - | - | Most promising follow-up modalities (sensitivities ≥90% and negative predictive values ≥99%, proportion of “screen-positives” ≤33%)= serum hCG, LSUPT + standardized assessment of women's symptoms, and standardized telephone consultation |
| Hassoun et al. [23] | Prospective, non-comparative | To assess the benefit of a self-performed urine semi-quantitative test in follow-up of medical abortion (concordance between qualitative LSUP test and quantitative blood hCG test) | France | May to Nov 2013 | ≤ 63 DA | 322 | LSUP hCG Duo 5-1000’’ + Serum hCG on the same day, 2-3 weeks after MIF | - | X | LSUP two detection thresholds: 5 and 1000 IU/L Comparison between LSUP and serum HCG test done the same day |
Concordance between urine and blood hCG levels: 94.5% CI95% [90.2%, 97.4%] |
| Horning et al. [20] | Retrospective | To compare lost to follow-up rates in women who chose follow-up by in-office US or serum β-hCG testing | USA | Sep 2007-Sep 2010 | ≤ 63 DA | 865 | Serum hCG assay | X | X (1 week after MIF) and repeated 1 week later at the clinic or at the lab | - | Lost to follow-up rates: ultrasound (22.9%) and β-hCG testing (33.7%) (NS) |
| US | X (from 1 week after MIF) | ||||||||||
| Iyengar et al. [31] | Prospective randomized controlled non-inferiority | To compare the effectiveness of standard clinic follow-up versus home assessment of outcome of medical abortion in a low-resource setting Primary outcome: Complete abortion |
India | Apr 2013-May 2014 | ≤ 63 DA | 731 | Routine clinic follow-up: Bimanual pelvic examination + LSUP 10-14 days after MIF Or: Self-assessment at home: LSUP (Vedalab, Alençon, France, Ultrasound), 10 to 14 days after MIF + home visit or phone call |
- | X | LSUP with a serum hCG cutoff of 1000 IU/mL) | Complete abortion: 313/336 (93%) in the clinic group vs 347/364 (95%) in the home group 233 women (81%) performed LSUP before being contacted by the research assistant, 54 (19%) did it after being reminded Adherence to scheduled follow-up: 78% in clinic vs 92% in home group |
| Kallner et al. [25] | Prospective observational |
To assess factors affecting acceptability and experience of home use of misoprostol for medical abortion up to 63 days | Sweden | Jan 2004-Apr 2007 | ≤ 63 DA | 395 | Low-sensitivity urine hCG assay (urine hCG, ANL Produkter, Alvsjo, Sweden) At the clinic | - | X (2 weeks after misoprostol) | In case of positive urine hCG test, US 500 U/mL cut-off | 66 (16.7%) women with positive urine test: 9 vacuum aspiration (4 ongoing pregnancies, 5 incomplete abortion or prolonged bleeding) |
| Lokeland et al. [17] | Prospective study | Evaluate decrease in beta-hCG after abortion | Norway | Oct 2005-Apr 2007 | 63-90 DA | 254 | Plasma beta-hCG | X | X D9 to D19 after MIF |
Measure of decrease | Decline > 97.5% Post-abortion test > 1 000IU/L in 10 women, but all abortions complete No info regarding test in 2 ongoing pregnancies |
| Lynd et al. [27] | Prospective, non-comparative | To investigate the feasibility of Vietnamese women doing a semi-quantitative pregnancy test at home to determine their abortion status | Vietnam | Sep 2009- Apr 2010 | ≤ 63 DA | 300 | Semiquantitative urine pregnancy test (SQPT) A 5-immunochromatographic assay panel (dBest hCG Panel Test, Ameritek, Seattle, WA, USA). The test operates as both a high- and low-sensitivity test | X | X (2 weeks after MIF) | SQPT high-sensitivity (5 ranges: 25-mIU/mL, 100-mIU/mL, 500 mIU/mL, 2000-mIU/mL and at least 10 000- mIU/mL | Medical abortion successful for 275/ 293 women All 11 ongoing pregnancies identified by the test 100% sensitivity, 89.7% specificity |
| Michie and Cameron [37] | Retrospective analysis of database | Assess simplified follow-up= telephone call + self-performed LSUP 2 weeks after procedure | Scotland | March 2011-Feb 2012 | ≤ 63 DA | 1084 | LSUP (Low Sensitivity Urine Pregnancy) test (Baby check Duo) | - | X 2 weeks after medical abortion |
Colour change at urine hCG level = 1000IU | On-going pregnancies in 2 women with positive LSUP and one who forgot to do test Sensitivity of telephone follow-up with LSUP= 100% Specificity = 88% |
| Oppegaard et al. [33] | Multicentre, comparative, randomized, non-inferiority, trial | To assess whether a commercially available semi-quantitative urine hCG test for self-assessment of abortion outcome would be as effective and manageable as outpatient follow-up | Europe (Austria, Finland, Norway, and Sweden) | Aug 2011-Jan 2013 | ≤ 63 DA | 924 | Routine clinical follow-up (LSUP or serum nCG or US, depending on sites) (n=466) Or Self-assessment at home (semi-quantitative urine test: two-step urine hCG DUO test (Vedal Lab, Alençon, France) + telephone) (n=458) 1-3 weeks after abortion |
US | X | SQPT: Two detection thresholds of 5 and 1000 IU/L | Complete abortion in 432/455 (95%) women in the routine follow-up group and 419/446 (94%) in the self-assessment group, 3 undetected continuing pregnancies (0·7%) in the self-assessment |
| Parashar et al. [16] | Prospective observational study | To evaluate endometrial thickness (US) and serum hCG as markers of successful treatment | Norway | Jan to Dec 2002 | ≤ 62 DA | 255 | Serum beta hCG (Immulite 2000 hCG). Detection limit = 3IU/L | Serum beta hCG | Serum beta hCG 15 to 71 days later | Visual inspection US |
Decrease of 99% in serum hCG in 99% women 0 on-going pregnancies Surgery: 14 (6%) |
| Paul et al. [32] | Same study as Iyengar | To investigate women’s acceptability of home-assessment of abortion and whether acceptability of medical abortion differs by in-clinic or home-assessment of abortion outcome in a low-resource setting in India | India | Apr 2013-May 2014 | - | - | - | - | - | - | 41% of women with a positive or unsure LSPT (n = 27) preferred clinic or doctor’s advice for follow-up in the event of a future abortion, compared with 14% of women with a negative LSPT result (n = 245) |
| Perriera et al. [29] | Prospective, non-comparative | To assess feasibility of using telephone calls combined with high-sensitivity urine pregnancy test as a primary method of follow-up | USA | March-Oct 2008 | ≤ 63 DA | 139 | First phone call (standardized questionnaire) 7 days after MIF If possibly not expelled US, otherwise, HSUPT (Sure-Vue™ high-sensitivity) 30 days after and phone call 3 days after |
- | - | High-sensitivity test (sensitivity 25 mIU/mL) | 100% of subjects eligible for first telephone follow-up were contacted 8/133 (6.1%) were asked to return for evaluation 8/125 (6.4%) eligible for 30-day phone call presented for interim visit prior to the call 2. After 30 days, 116/117 (99.1%) eligible subjects were contacted. 27/116 (23.3%) subjects had a positive pregnancy test, 2/116 had inconclusive pregnancy test, Complete follow-up achieved in 135 of the 139 subjects (97.1%, 95% CI 94.3–99.9%). |
| Platais et al. [30] | Prospective, comparative, randomized | To evaluate the feasibility and acceptability of phone follow-up with a home semi-quantitative urine pregnancy test and standardized checklist, and compare it to alternative method of follow-up at clinic | Moldava Uzbekistan |
July 2010-Nov 2012 | ≤ 63 DA | 2400 | Clinic visit: Clinical examination + symptoms ± US, 2 weeks after MIF Semi-quantitative urine pregnancy test (dBest hCG Panel Test, Ameritek, Seattle, WA, USA) + symptoms checklist to be completed before phone call 2 weeks after medical abortion (phone group) |
- | ± X X (for baseline value for phone FUP group) |
Five ranges of hCG assigned with this test: 25-99 mIU/mL, 100-499 mIU/mL, 500-1999 mIU/mL 2000-9999 mIU/mL, and greater than 10,000 mIU/mL |
Successful contact in 97.6% phone group, vs 100% clinic visits in clinic group Ongoing pregnancy rate similar in both groups (0.4-0.6%) as well as complete abortion rate (97,6) Semi-quantitative pregnancy test identified all ongoing pregnancies in phone follow-up group |
| Pocius et al. [14] | Prospective physiologic | To describe the decline in serum hCG in the first 5 days following medical abortion | USA | NA | ≤ 63 DA | 66 | Measure of serum hCG on D1, D3, D5, D7-14 | - | - | Percent hCG decline from Day 1 to each measure | Complete medical abortion: 97% 2 pregnancies (1 not detected by decline hCG) 95% of women with a complete abortion have a decline of ≥ 90.1% in hCG by Day 5 |
Abbrevations: CI: Confidence Interval; DA: Days of Amenorrhea; FU: Follow Up; HSPT: High-Sensitivity Pregnancy Test; HSUP: High-Sensitivity Urine Pregnancy Test; LSUP: Low-Sensitivity Urine Pregnancy Test; MLPT: Multilevel Urine Pregnancy Test; NA: Not Available; NS: Not Significant; SOC: Standard of Care; SQPT: Semi-Quantitative Pregnancy Test; UPT: Urinary Pregnancy Test; US: Ultrasound; WA: Weeks of Amenorrhea
Table 1: Description of publications included in this review.
Results
The course of hCG during pregnancy and after medical abortion
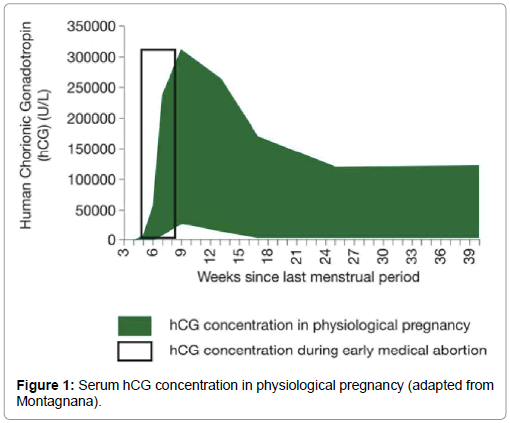
During pregnancy, hCG values differ significantly. Levels are zero in non-pregnant women, show pronounced changes over time like doubling every 48-72 h in early pregnancy, peak at 8-11 weeks of gestation at levels around 200.000 U/L and then decline for the rest of the pregnancy [10]. In early pregnancy, urinary hCG levels increase daily by approximately 50% [11]. But huge individual variations make it impossible to date gestational age based on hCG levels. Similarly, it is not possible to diagnose successful abortion with a single test at follow-up within two weeks after treatment. This explains why two tests are needed to give a rapid result of the abortion, one at baseline and one at follow-up to determine the outcome (Figure 1).
The decline in serum hCG following pregnancy termination is steep initially, but low levels can remain up to 4-6 weeks. An hCG decrease in the days following medical abortion is described in different studies [12- 14]. There is no consensus regarding the threshold of hCG at follow-up in terms of percent of the initial value that would indicate a successful abortion. Different opinions also exist on the speed of decrease of hCG following medical abortion. The rate was thought by some authors to depend on the initial hCG level, with a more rapid decline associated with a higher baseline concentration before treatment [12]. Following medical abortion using mifepristone and misoprostol, hCG declined by 70.5 ± 8.8% in the 24 h following misoprostol, with no correlation between the percentage decline within 24 h and the peak hCG level measured prior to misoprostol administration [6]. Further, the reported rate of decline ranged widely from 21% to 35% at 2 days and 60% to 84% at 7 days, depending on initial hCG value or with at least a 90% decline in 95% of women at 5 days [12,14].
Serum hCG testing to determine outcome of medical abortion
In a prospective observational study, Fiala et al. compared the usefulness of hCG measurement and ultrasound examination before and after medical abortion to determine treatment outcome [3]. The study included 217 women who underwent medical termination of pregnancy up to 49 days of amenorrhea using mifepristone and misoprostol. Ultrasound examination and a serum hCG test were performed before treatment and at follow-up (D6-D18). The hCG levels at follow-up dropped to a mean of 3% (± 3) of the value before treatment, ranging from 1 to 44% of the initial value in cases of successful abortion. When 20% of the initial hCG value was used as a cut-off, a positive predictive value for successful expulsion of 0.995 was obtained. If the reduction of the hCG level was less than 80%, the negative predictive value was 0.5 and further evaluation was needed to confirm the outcome of treatment.
Further studies confirmed these results. In a retrospective study of 172 women who underwent medical abortion for pregnancy up to 63 days, the rate of decrease in hCG from baseline to 7 days was above 20% in only 4/91 women with successful abortions [15]. A prospective study described a decrease of 99% in serum hCG at 15-71 days in 99% of 255 women who underwent abortion up to 63 days [16].
Another prospective observational study of 254 women who underwent medical abortion from 63 to 90 days showed a decline in hCG above 97.5% in women with successful termination [17].
In a prospective comparative study of 144 women with treatment for missed abortion or blighted ovum and a gestational age below 12 weeks, serum hCG testing was considered as effective as ultrasound in confirming medically-induced abortion 2 and 4 weeks after expulsion, with a kappa correlation coefficient of 0.327 [18].
A prospective, controlled and randomized study of 376 women who underwent medical abortion up to 63 days showed no significant difference in the low-level rate of unplanned interventions and visits between arms -8.2% in the hCG arm vs 6.6% in the ultrasound arm at 2 weeks [19].
The use of serum hCG testing did not significantly decrease adherence to follow-up visits. In a retrospective chart review of 885 women who underwent medical abortion, the rates of loss to followup were 23% in women choosing follow-up via in-office ultrasound assessment and 34% in women choosing hCG testing [20]. However, the women who chose hCG testing were inherently less likely to follow up. There was no difference between groups in the rate of loss to follow- up in another prospective study comparing the adherence to follow-up between standard in-clinic and remote follow-up in 129 women who underwent medical abortion up to 49 days of gestation (rate of loss to follow-up: 28% for remote vs 23% for standard follow-up) [21].
Urine pregnancy test (urine hCG test) and medical abortion
The concordance between urine and serum beta-hCG measurement was demonstrated in multiple studies.
Urine beta-hCG testing (Orchid Biomedical System) followed by serum testing in 97 women up to 3 weeks after medical abortion (or during normal pregnancies) demonstrated good sensitivity (89%) and specificity (72%) of the urine test for identifying individuals with a serum beta-hCG >1000 U/L [22]. In another prospective study of 322 women who underwent medical abortion up to 63 days, the concordance between urine (low sensitivity urine pregnancy test hCG Duo 5-1000) and serum beta-hCG levels was 94.5% [23].
Urine pregnancy tests have good sensitivity and good specificity to detect outcome of medical abortion up to 63 days [1,24-27]. Therefore, low-sensitivity hCG tests were developed. In a prospective observational study of 3054 women who underwent medical abortion up to 63 days, a low-sensitivity urine pregnancy test combined with women’s self-assessment and a non-sonographic clinical evaluation was as effective as US in identifying all women with on-going pregnancies at follow-up 7 to 14 days after treatment [28].
Self-assessment using urine pregnancy test combined with other measures
Different self-assessment protocols that women can do at home were evaluated using various urine tests. The objective was to decrease the high loss to follow-up to 18 to 30% when women are asked to return for a follow-up visit and to determine medical abortion outcomes while individualising follow-up according to women’s preference [22]. Low-sensitivity urinary pregnancy tests have various thresholds of hCG ranging from 500 to 2000 mIU/ml, while high-sensitivity urinary pregnancy tests can detect hCG levels as low as 5 mIU/ml.
The feasibility of protocols combining a urine pregnancy test and telephone follow-up was confirmed in multiple studies. A protocol required a phone call 7 days after mifepristone administration, followed by US if the woman or clinician thought the pregnancy was not expelled. Otherwise, cases were followed by a high-sensitivity urine pregnancy test 30 days after mifepristone and a phone call 3 days after the urinary test. It led to 97% complete follow-up in 139 women undergoing medical abortion up to 63 days [29]. In a study in 2400 women, the use of a home semi-quantitative urine pregnancy test in combination with a standardized checklist over the phone led to a 98% rate of follow-up. This compared to a 100% follow-up rate in women attending clinical examination in combination with optional US 2 weeks after mifepristone for medical abortion up to 63 days [30]. The adherence to scheduled follow-up was 92% in women who took a low-sensitivity urine pregnancy test at home in combination with a home visit or phone. This compared to a 78% follow-up rate for women coming to a clinic 10 to 14 days after medical abortion for a bimanual pelvic examination and low-sensitivity urine pregnancy test in a randomized study of 731 women undergoing medical abortion up to 63 days [31,32]. A prospective, comparative, randomized study compared clinical assessment with self-assessment of abortion outcome in 924 women who underwent medical abortion up to 63 days. Follow-up was performed 1 to 3 weeks after abortion. No women in the routine follow-up group had undetected continuing pregnancies in the second trimester, versus 3 (0.7%) in the self-assessment group. However, selfassessment was non-inferior to routine follow-up [33].
The usefulness of a remote/at home follow-up was also assessed in a prospective study comparing the rate of follow-up in 999 women undergoing medical abortion up to 63 days [34]. Women were randomized either to: 1) a “clinic-based” group with US 1 week after mifepristone administration or a high-sensitivity urine pregnancy test performed at 3 weeks and a telephone call with clinic staff if the woman could not attend the 1-week follow-up visit or 2) to a “remote follow-up” group using a low-sensitivity pregnancy test and a standardized questionnaire administered by a non-clinical call centre operator by phone, text message or internet 2 weeks after treatment. The rate of follow-up was 69% for remote follow-up and 73% for clinic-based follow-up, but in the latter group, most failed to return for their scheduled US and were followed by phone (83%). This high level of follow-up was also confirmed in a retrospective analysis of 176 women who underwent medical abortion up to 63 days with a rate of lost to follow-up of 5.6% for phone follow-up in combination with urine pregnancy test within 4 weeks after medical abortion [35].
The sensitivity and specificity of a remote protocol using a lowsensitivity urine pregnancy test in combination with telephone followup, were high, respectively 75% to 100% and 85 to 88% at 2 weeks after medical abortion up to 63 days [31,36-38].
During clinical studies, 81 to 85% of women did a home urine pregnancy test without waiting for the planned telephone follow-up [28,35]. Based on this finding, a study was conducted where women could do a urine pregnancy test at home in combination with selfassessment. Women were asked to contact the abortion service in case of a positive or invalid test and in case of predefined signs and symptoms. Results were assessed in 1726 women undergoing medical abortion up to 63 days [39]. A total of 96% of women chose self-assessment and 6% of those phoned the service. Eight on-going pregnancies occurred (0.5%, 95% confidence interval 0.2-0.9%), with 4 detected within 4 weeks of treatment and the remainder not detected until one or more missed menses after the procedure. In another prospective study, the self-assessment was provided either as a paper document or as an automated interactive questionnaire on women’s mobile phones [40]. There was a good prediction of complete procedure in 71% of women who used the mobile phone assessment and 91% of those who sent a paper assessment.
A 2011 Cochrane meta-analysis of 8 studies looked at alternative follow-up modalities after first-trimester medication abortion to diagnose on-going pregnancy or retained gestational sac [9]. The sensitivity, specificity, positive predictive value and negative predictive value were calculated and compared with ultrasound or clinician examination. The most promising follow-up modalities included serum hCG measurements, low sensitivity urine pregnancy test combined with a standardized assessment of women's symptoms and standardized telephone consultation (perhaps followed by high sensitivity urine pregnancy test). These follow-up modalities had sensitivities of ≥ 90% and negative predictive values of ≥ 99% and resulted in a proportion of “screen-positives” of ≤ 33%.
Discussion
The aim of this review was to describe the use of hCG testing for medical abortion outcomes. More specifically, it explored urinary hCG testing using low-sensitivity tests that could facilitate self-assessment follow-up, improve access to medical abortion in areas where there is no US access, decrease the rate of unnecessary surgery in case of misinterpretation of US, reduce the time interval until outcome can be determined and increase women’s autonomy in the abortion process.
Thirty-five studies were identified, of which 20 were related to urinary hCG testing, either alone or in combination with selfassessment. These studies illustrated the course of historic development of current tests, including the initial use of serum hCG testing, followed by the use of high-sensitivity urinary pregnancy tests and finally, lowsensitivity urinary hCG testing. This may explain the differences found in the results of these studies.
This review confirmed that serum hCG testing allows for determination of medical abortion outcomes. The good sensitivity and good specificity of urine hCG tests to detect outcomes up to 63 days was also demonstrated. However, the high sensitivity to detect hCG and slow reduction of hCG in the human body after a successful termination of pregnancy implies that a very long interval is necessary before a normal hCG test would become negative, i.e. 4-6 weeks. This could lead to a delay in the diagnosis of on-going pregnancy as well as stress for the woman. New, low-sensitivity urine hCG tests have therefore been developed to allow for earlier assessment.
To increase acceptability and reduce unnecessary surgical and medical interventions after medical abortion, the current follow-up protocols after medical termination of pregnancy should be revised. Current follow-up protocols, sometimes even legally mandatory, require the woman to come back to the clinic for an additional visit and/ or for US. The high loss to follow-up rate may be due to the woman’s conviction that the pregnancy has ended combined with a good health feeling. Consequently, many women see no need to spend time and energy to see a doctor. Moreover, in countries where transportation is difficult, interest in self-assessment using urinary hCG testing was demonstrated [31].
Of the recently proposed follow-up protocols, most do not recommend a clinic visit. Follow-up may consist of remote assessment, which may include clinical symptom assessment as well as hCG testing using low sensitivity urine pregnancy test. Some use urine pregnancy testing combined with telephone follow-up. The latter could be replaced with written information given to patients as there is nothing that could be asked exclusively during a telephone by another person instead of written information handed over to the patient. A recent study from Scotland found that when given the option, most women who plan to go home to expel a pregnancy following an early medical abortion choose not to receive a phone call from the abortion service [41].
Relying solely on hCG testing at early follow-up in medical abortion is challenging because of huge individual hCG variations during the first trimester. A reliable diagnosis based on a single test becomes even more difficult because of the variation of hCG decline after successful medical abortion. Therefore, a baseline hCG test at the beginning of treatment is necessary to allow comparison with the follow-up result. However, the new low-sensitivity tests allow use of a single test if an intrauterine pregnancy has been diagnosed at the beginning of treatment. Another benefit of these new tests is their ease of use for all women regardless of education or literacy level.
One of the limitations of this review is the absence of information regarding surgical management of medical abortion outcomes in the presence or absence of hCG testing. This does not allow for any comparison between various follow-up techniques. In addition, concomitant parameters including the quality of medical care, the psychological and relational dimensions of the woman’s request and the woman’s feelings during abortion should also be taken into account when comparing various follow-up techniques.
Conclusions
The different protocols described in this review, including serum hCG testing, urinary hCG testing, paper questionnaire for selfassessment and mobile phone questionnaire, allow practitioners to individualise and personalise medical abortion follow-up without impairing safety, as long as contraceptive counselling is undertaken before initiation of medical abortion. The use of low-sensitivity urine hCG testing improves follow up, as it saves women from unnecessary clinic visits and shortens the time interval to obtain accurate results.
Declarations
Funding: This work was supported by a grant from Exelgyn.
Acknowledgments: The authors wish to thank Laurence Saya, MD, Altius Pharma CS, for help in bibliographic analysis and medical writing and Joyce Arthur, Executive Director of the Abortion Rights Coalition of Canada, for her contribution in the revision of this work.
Declaration of interest: The authors are members of the external scientific advisory board of Exelgyn. Christian Fiala has served on an ad hoc basis as an invited lecturer for Exelgyn. Teresa Bombas is a Member of a global advisory board at Merck and HRA, speaker of conferences/symposium organized by Bayer, MERCK, HRA, Gedeon and Exelgyn. Mirella Parachini has an occasional consultancy relationship with Exelgyn and Nordic. Aubert Agostini is a member of the board at Nordic Pharma and MSD. He is an investigator in Nordic Pharma studies. Roberto Lertxundi has a financial relationship (member of advisory boards, lecturer and/or consultant) with Exelgyn, Nordic-Pharma, Exeltis, Bayer-Pharma and Teva. Marek Lubusky has an occasional consultancy relationship with Exelgyn and Nordic. Kristina Gemzell-Danielsson serves or has served on an ad hoc basis as an invited lecturer for Exelgyn, Line Pharma, Gynuity and as an investigator in clinical trials conducted by Concept Foundation/ SunPharma.
References
- WHO (2012) Safe abortion: Technical and policy guidance for health systems.
- Fiala C, Gemzel-Danielsson K (2006) Review of medical abortion using mifepristone in combination with a prostaglandin analogue. Contraception 74: 66-86.
- Fiala C, Safar P, Bygdeman M, Gemzell-Danielsson (2003) Verifying the effectiveness of medical abortion: Ultrasound versus hCG testing. Eur J Obstet Gynecol Reprod Biol 109: 190-195.
- Reeves MF, Fox MC, Lohr PA, Creinin MD (2009) Endometrial thickness following medical abortion is not predictive of subsequent surgical intervention. Ultrasound Obstet Gynecol 34: 104-109.
- Peyron R, Aubeny E, Targosz V, Silvestre L, Renault M, et al. (1998) Early termination of pregnancy with mifepristone (RU 486) and the orally active prostaglandin misoprostol. N Engl J Med 21: 1509-1513.
- Lähteenmäki P, Luukkainen T (1978) Return of ovarian function after abortion. Clin Endocrinol 8: 123-132.
- Schreiber CA, Sober S, Ratcliffe S, Creinin MD (2011) Ovulation resumption after medical abortion with mifepristone and misoprostol. Contraception 84:230-233.
- Hognert H, Kallner HK, Cameron S, Nyrelli C, Jawad I, et al. (2016) Immediate versus delayed insertion of an etonogestrel releasing implant at medical abortion-a randomized controlled equivalence trial. Hum Reprod 31: 2484-2490.
- Grossman D, Grindlay K (2011) Alternatives to ultrasound for follow-up after medication abortion: A systematic review. Contraception 83: 504-510.
- Blum J, Shochet T, Lynd K, Lichtenberg ES, Fischer D, et al. (2012) Can at-home semi-quantitative pregnancy tests serve as a replacement for clinical follow-up of medical abortion? A US study. Contraception 86: 757-762.
- Gnoth C, Johnson S (2014) Strips of hope: Accuracy of home pregnancy tests and new developments. Geburtsh Frauenheilk 74: 661-669.
- Barnhart K, Sammel MD, Chung K, Zhou L, Hummel AC, et al. (2004) Decline of serum human chorionic gonadotropin and spontaneous complete abortion: Defining the normal curve. Obstet Gynecol 104: 975-981.
- Honkanen H, Ranta S, Ylikorkala O, Heikinheimo O (2002) The kinetics of serum hCG and progesterone in response to oral and vaginal administration of misoprostol during medical termination of early pregnancy. Hum Reprod 2: 2315-2319.
- Pocius KD, Bartz D, Maurer R, Stenquist A, Fortin J, et al. (2016) Serum human chorionic gonadotropin (hCG) trend within the first few days after medical abortion: A prospective study. Contraception 95: 263-268.
- Clark W, Panton T, Hann L, Gold M (2007) Medication abortion employing routine sequential measurements of serum hCG and sonography only when indicated. Contraception 75: 131-135.
- Parashar P, Iversen OE, Midboe G, Myking O, Bjorge L (2007) Medical abortion in the first trimester: The use of serum hCG and endometrial thickness as markers of completeness. Eur J Contracept Reprod Health Care 12: 366-371.
- Lokeland M, Iversen OE, Dahle GS, Nappen MH, Ertzeid L, et al. (2010) Medical abortion at 63 to 90 days of gestation. Obstet Gynecol 115: 962-968.
- Behnamfar F, Mahdian M, Rahimi F, Samimi M (2013) Misoprostol abortion: Ultrasonography versus beta-hCG testing for verification of effectiveness. Pak J Med Sci 29: 1367-1370.
- Dayananda I, Maurer R, Fortin J, Goldberg AB (2013) Medical abortion follow-up with serum human chorionic gonadotropin compared with ultrasonography: A randomized controlled trial. Obstet Gynecol 121: 607-613.
- Horning EL, Chen BA, Meyn LA, Creinin MD (2012) Comparison of medical abortion follow-up with serum human chorionic gonadotropin testing and in-office assessment. Contraception 85: 402-407.
- Dunn S, Panjwani D, Gupta M, Meaney C, Morgan R, et al. (2015) Comparison of remote and in-clinic follow-up after methotrexate/misoprostol abortion. Contraception 92: 220-226.
- Grossman D, Berdichevsky K, Larrea F, Beltran J (2007) Accuracy of a semi-quantitative urine pregnancy test compared to serum beta-hCG measurement: A possible screening tool for ongoing pregnancy after medication abortion. Contraception 76: 101-104.
- Hassoun D, Périn I, Hiên H, Demars HH (2016) Feasibility of self-performed urine pregnancy testing for follow-up after medical abortion. Eur J Obstet Gynecol Reprod Biol 197: 174-178.
- Godfrey EM, Anderson A, Fielding SL, Meyn L, Creinin MD (2007) Clinical utility of urine pregnancy assays to determine medical abortion outcome is limited. Contraception 75: 378-382.
- Kallner HK, Fiala C, Gemzell-Danielsson K (2012) Assessment of significant factors affecting acceptability of home administration of misoprostol for medical abortion. Contraception 85: 394-397.
- Blum J, Sheldon WR, Ngoc NT, Winikoff B, Nga NT, et al. (2016) Randomized trial assessing home use of two pregnancy tests for determining early medical abortion outcomes at 3, 7 and 14 days after mifepristone. Contraception 94: 115-121.
- Lynd K, Blum J, Ngoc NT, Shochet T, Blumental PD, et al. (2013) Simplified medical abortion using a semi-quantitative pregnancy test for home-based follow-up. Int J Gynaecol Obstet 121: 144-148.
- Clark W, Bracken H, Tanenhaus J, Schweikert S, Lichtenberg ES, et al. (2010) Alternatives to a routine follow-up visit for early medical abortion. Obstet Gynecol 115: 264-272.
- Perriera LK, Reeves MF, Chen BA, Hohmann HL, Hayes J, et al. (2010) Feasibility of telephone follow-up after medical abortion. Contraception 81: 143-149.
- Platais I, Tsereteli T, Comendant R, Kurbanbekova D, Winikoff B (2015) Acceptability and feasibility of phone follow-up with a semiquantitative urine pregnancy test after medical abortion in Moldova and Uzbekistan. Contraception 91: 178-183.
- Iyengar K, Paul M, Iyengar SD, Klingberg-Alvin M, Essen B, et al. (2015) Self-assessment of the outcome of early medical abortion versus clinic follow-up in India: A randomised, controlled, non-inferiority trial. Lancet Glob Health 3: e537-545.
- Paul M, Iyengar K, Essén B, Gemzell-Danielsson K, Iyengar SD, et al. (2015) Acceptability of home-assessment post medical abortion and medical abortion in a low-resource setting in Rajasthan, India. Secondary outcome analysis of a non-inferiority randomized controlled trial. PLoS One 10: e0133354.
- Oppegaard KS, Qvigstad E, Fiala C, Heikinheimo O, Benson L, et al. (2015) Clinical follow-up compared with self-assessment of outcome after medical abortion: A multicentre, non-inferiority, randomised, controlled trial. Lancet 385: 698-704.
- Bracken H, Lohr PA, Taylor J, Morroni C, Winikoff B (2014) RU OK? The acceptability and feasibility of remote technologies for follow-up after early medical abortion. Contraception 90: 29-35.
- Chen MJ, Rounds KM, Creinin MD, Cansino C, Hou MY (2016) Comparing office and telephone follow-up after medical abortion. Contraception 94: 122-126.
- Cameron ST, Glasier A, Dewart H, Johnstone A, Burnside A (2012) Telephone follow-up and self-performed urine pregnancy testing after early medical abortion: A service evaluation. Contraception 86: 67-73.
- Michie L, Cameron ST (2014) Simplified follow-up after early medical abortion: 12-month experience of a telephone call and self-performed low-sensitivity urine pregnancy test. Contraception 89: 440-445.
- Dabash R, Shochet T, Hajri S, CHelli H, Hassairi AE, et al. (2016) Self-administered multi-level pregnancy tests in simplified follow-up of medical abortion in Tunisia. BMC Womens Health 16: 49.
- Cameron ST, Glasier A, Johnstone A, Dewart H, Campbell A (2015) Can women determine the success of early medical termination of pregnancy themselves? Contraception 91: 6-11.
- Constant D, De-Tolly K, Harries J, Myer L (2015) Assessment of completion of early medical abortion using a text questionnaire on mobile phones compared to a self-administered paper questionnaire among women attending four clinics, Cape Town, South Africa. Reprod Health Matters 22: 83-93.
- Montagnana M, Trenti T, Aloe R, Cervellin G, Lippi G (2011) Human chorionic gonadotropin in pregnancy diagnostics. Clin Chim Acta 412: 1515-1520.
Citation: Fiala C, Bombas T, Parachini M, Agostini A, Lertxundi R, et al. (2019) hCG Testing to Determine Outcome after Medical Abortion: A Review. J Preg Child Health 6:409
Copyright: © 2019 Fiala C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 34122
- [From(publication date): 0-2019 - Apr 06, 2025]
- Breakdown by view type
- HTML page views: 33111
- PDF downloads: 1011