Research Article Open Access
Harvesting Free Palatal Masticatory Mucosal Graft Using 3a Mucotome
Amit Arvind Agrawal* and Amit Sope
Department of Periodontics and Implantology, MGV’s KBH Dental College and Hospital, India
- *Corresponding Author:
- Amit Arvind Agrawal
MDS, M Phil, MGV’s KBH Dental College and Hospital
Nashik, Maharashtra, India
E-mail: agrodent@rediffmail.com
Received Date: April 06, 2016; Accepted Date: May 10, 2016; Published Date: May 18, 2016
Citation: Agrawal A A, Sope A (2016) Harvesting Free Palatal Masticatory Mucosal Graft Using 3a Mucotome. J Interdiscipl Med Dent Sci 4:197. doi: 10.4172/2376-032X.1000197
Copyright: © 2016 Agrawal A A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Introduction: Free masticatory mucosal grafts are frequently being used in various indications during periodontal plastic surgeries. It can be procured from donor site, usually the palate, using scalpels, gingivectomy knife or palatal shaving knife. However, drawbacks of previous methods for procuring free masticatory mucosal graft motivated the idea to utilize a new device to obtain a more uniform graft with lesser time and efforts.
Aims and objective: This article intend to discuss the technical details and clinical application of the proposed ‘3A mucotome’ in two cases having gingival recession with associated mucogingival deformity.
Case series: Post-operative follow-up of two cases, at 1.5 and 1 year respectively, showed satisfactory increase in width of attached gingiva and root coverage.
Conclusion: The wider range of blade adaptation to the palate was the main thrust of this device modification. In addition to this, the precise cutting of the instrument and satisfactory control over its movement produced grafts of uniform thickness and without macrolacerations.
Keywords
Mucotome; Free gingival graft; Pacquette knife; Ivory matrix retainer; Free masticatory mucosal grafts
Introduction
The technique of free autogenous gingival grafting (FGG) has undergone little modification since its introduction by Bjorn in Scandinavia in 1963 [1] and by King and Pennel in the United States in 1964 [2]. The technique is widely used to treat a variety of mucogingival problems such as insufficient or lack of attached gingiva, the presence of high frenum attachments, shallow fornix and denuded roots following gingival recession [3-5]. FGG can be procured from donor site using scalpels, gingivectomy knife or palatal shaving knife (Paquette knife). The donor site is frequently the palate, although the use of edentulous ridge areas, tuberosity and attached gingiva has also been described. Scalpel is most commonly used and conventional method for procuring gingival auto grafts. Gingivectomy knife, although not commonly used, also works on similar principle.
Since the scalpel blade is straight and stiff and the palate is curved, repeated incisions to release the graft from underlying connective tissue results in ragged surface both on undersurface of grafts and raw surface of donor site, which then takes longer time to heal. Most of these problems were solved when ‘Paquette knife’ was introduced. Snyder [6] first reported use of a ‘palatal shaving knife’ devised by Uohara and Federbusch for obtaining the graft specimen. It was also referred to as the ‘blade-loop knife’ by Antonelli et al. [7]
However following limitations could be observed while using Pacquette knife,
a. The curvature of the blade has limited range of adjustment, which is by finger pressure or by use of plier only.
b. For attachment of razor blade strip on rod, the insertion points for both ends of the blade are very close to each other. This creates a sharp curve (bend) and hence it becomes difficult to adjust the blade against comparatively shallow curvature of the palate, even after finger/ plier modification.
c. Because of the sharp curve and limited range of movement of the razor blade strip on the Paquette knife, the graft obtained are narrower and considerably thicker in the middle part as compared to their edges.
d. Accurate technique for use of this instrument is lacking in the literature; hence there are multiple unanswered questions such as position of finger rest, angulation of blade and handle and method of mounting the blade on the handle, etc.
In view of the above limitations, the search for a device which would offer significant advantages over the conventional methods of procuring FGG was much felt. The present article describes technical modification of ivory matrix retainer no. 8 to hold a razor blade and its clinical application as a mucotome (provisional patent number 1753/ mum/2011) for procuring FGG / free masticatory mucosal autograft (FMMG) from palate.
Material and Methods
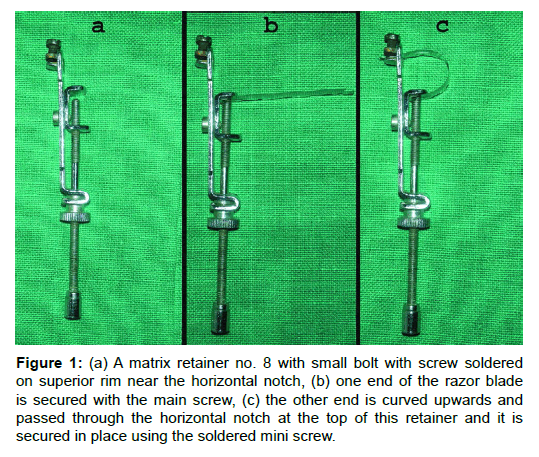
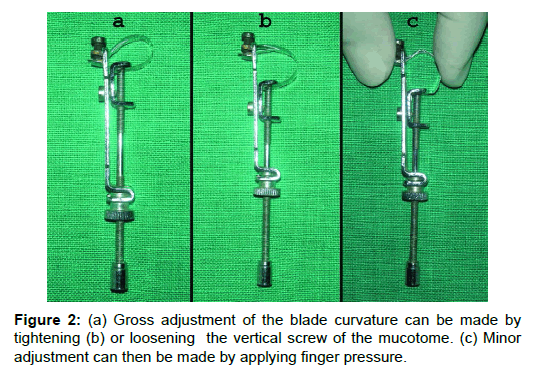
Ivory matrix retainer no.8 is originally used in ‘conservative dentistry’ to support silver amalgam restoration during condensation in class-I compound and class-II MOD (mesial occlusal distal) cavities. A small bolt is soldered on superior rim of the horizontal notch such that a small screw when passed through it will help to secure the superior end of the cutting blade (Figure 1a). A commercially available stainless steel razor blade is broken into half lengthwise and is engaged on this device so that it functions like a mucotome One end of the razor blade is secured with the main screw (Figure 1b), the other end is curved upwards and passed through the horizontal notch at the top of this retainer and it is secured in place using the soldered mini screw (Figure 1c). At times the superior end of blade, passing through the notch, may need slight trimming with scissors for proper fit. The direction of cutting edge of the razor blade should be adjusted according to the selection of donor site and direction of movement of the device. Since the attachment of the two ends of blade are sufficiently far enough the blade has a comparatively shallow curvature (as compared to the Paquette knife). The curved part of the blade is placed against the palate; adjustment can be made in curvature of the blade to best match the curvature of the donor site, to obtain a graft of approximately uniform thickness. Gross adjustment of the blade curvature can be made by tightening (Figure 2a) or loosening the vertical screw of the mucotome (Figure 2b). Minor adjustment can then be made by applying finger pressure to the curved part of the blade or manipulating with a plier (Figure 2c). Thus a greater range of adjustment can be done to best adapt the curvature of the blade to the varying anatomy of palate in different patients.
Figure 1: (a) A matrix retainer no. 8 with small bolt with screw soldered on superior rim near the horizontal notch, (b) one end of the razor blade is secured with the main screw, (c) the other end is curved upwards and passed through the horizontal notch at the top of this retainer and it is secured in place using the soldered mini screw.
Clinical Cases
Case-1
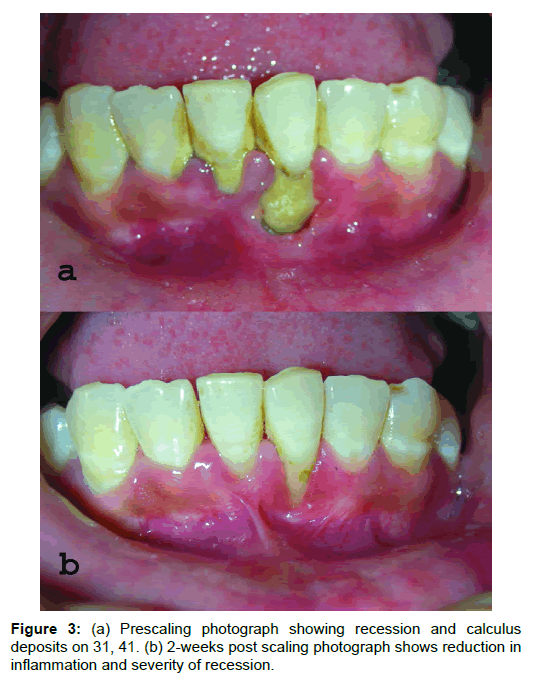
A 35-year-old female patient reported with a complaint of receding gums in mandibular anterior region. On examination, patient had 7 mm of labial recession with 31 and 3mm with 41. Probing depth was around 2mm, inadequate width of attached gingiva (positive tension test) with 31 and ++ calculus score [8] with 31and 41 (Figure 3a). Thorough scaling and root planning was performed and patient was advised to continue chlorhexidine mouthwash for two weeks. Post-scaling results after 2-weeks showed significant reduction in inflammation, reduction of recession by 1mm each on 31 and 41 and reduction in more than 50% of width of recession defect with 31 (Figure 3b). However, the high frenal attachment can be more clearly appreciated and the width of attached gingiva is still inadequate. For correction of high frenum and to increase the width of attached gingiva together with root coverage, a FMMG seemed to be the most appropriate choice of surgery.
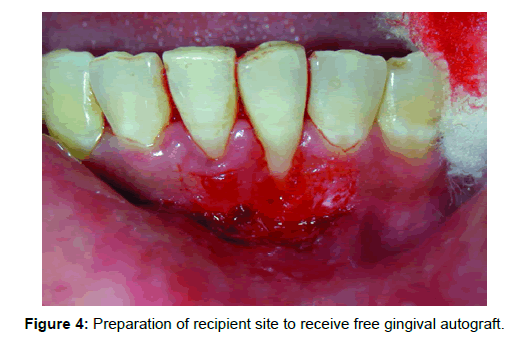
Recipient site: Surgical procedure began with the preparation of the recipient site utilizing sharp dissection to remove surface epithelium, lamina propria and submucosal layers, leaving a thin layer of connective tissue and periosteum covering the osseous surfaces (Figure 4). It was advocated that the remaining tissue should be smooth to prevent dead spaces from occurring between the graft and its recipient bed. One of the few modifications in the preparation of the recipient site is the use of a fenestration at the base of the graft where the new mucogingival junction is to be established.
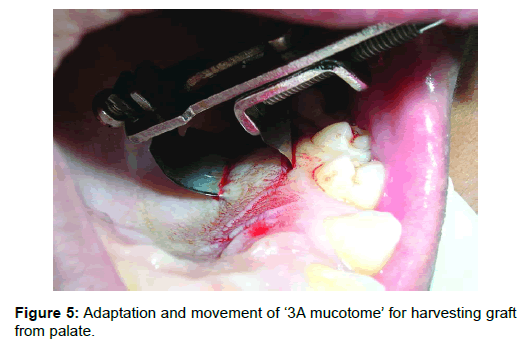
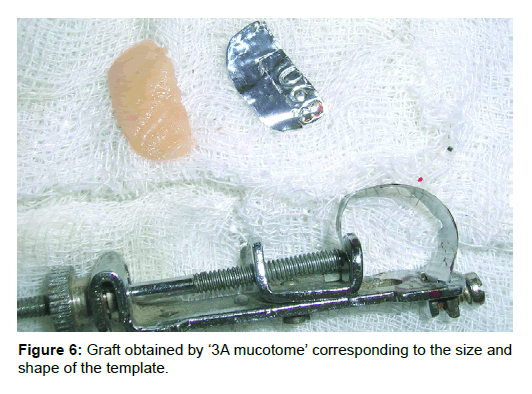
Donor site: Palatal masticatory mucosa between palatal root of 1st molar and canine was anesthetized; the required size of graft was marked on the palate with the help of a template. The curved blade of mucotome was kept at the distal end of the mark with the cutting edge of blade facing mesially. The contoured blade was engaged into the mucosa and moved anteriorly till the marking towards the palatal root of cuspid (Figure 5). Finger rest can be easily taken on occlusal surface of molars, which will provide stability while moving the blade anteriorly. The desired thickness of the graft can be varied according to the angulation of the blade with respect to the surface of palatal mucosa while moving through the tissues. Another way to judge the thickness is by the faint grayish color of the blade observed beneath the tissue. Smooth pass of the razor blade through tissue produces graft of uniform thickness with smooth cut undersurface. At times a slight jiggling/seesaw movement may be required for smooth movement of the blade. Borders of graft have long internal bevel due to curvature of blade. The better the blade curvature adapted to the curvature of the palate, the shallower will be the beveled margin. The edges can be left beveled or if desired can be trimmed with a scissor to obtain a butt joint. In case a butt joint is desired, the size of the graft should be slightly larger than the template size. Trimming the margins of graft would provide a butt joint without compromising the required graft size (Figure 6).
Grafts obtained with thick areas, uneven surfaces or with fatty or glandular tissues attached can be corrected easily using the same instrument to trim the undersurface of the graft. For this, one end of the graft is held tightly with a tissue forceps and cutting edge of blade of mucotome is placed on raw surface and moved away from tissue forceps to other end aiming to remove the excess unwanted tissues. Failure to remove this fat and glandular tissue will result in the graft that is totally movable when probed. The fat and glandular tissues inhibit the graft take by reducing plasmatic diffusion.
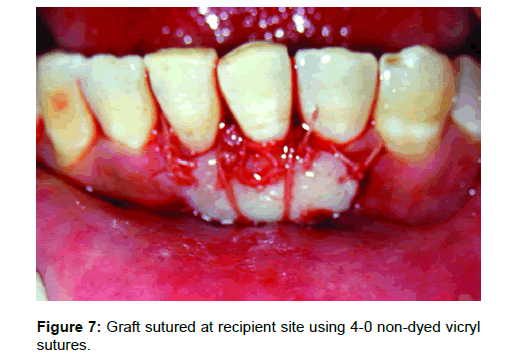
Citric acid root conditioning prior to FGG coverage of denuded roots may increase the likelihood of reattachment, but controlled studies to determine the value of the procedure done on human subjects have not found any justifiable reason to do so [9]. The graft is sutured in place with resorbable suture so that the external bevel of the recipient site corresponds with the internal bevel of the graft. This type of "lap joint" seems to virtually eliminate the thick bulgy appearance that often occurs at the graft-bed junction if a "butt joint" is used. After adaptation with moist gauze, the graft was stabilized in place using 4-0 vicryl sutures, coronally and laterally. Horizontal stretching suture should be used to overcome the effects of primary contraction. This stretching suture allows the blood vessels within the graft to open, and permit diffusion of fluid. Additional sutures were given across the graft vertically for better adaptation over recipient bed; thereby avoid dead space adjacent to root prominence (Figure 7).
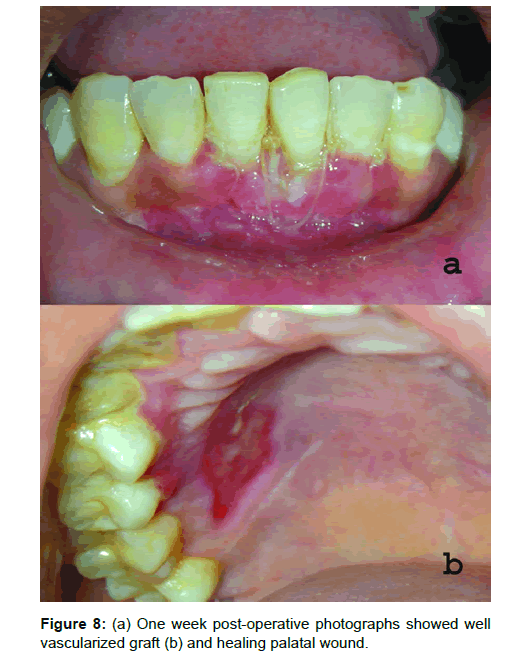
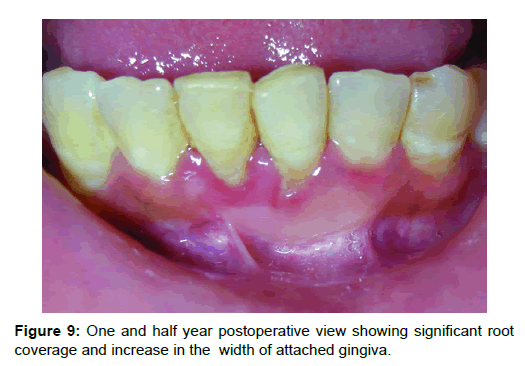
Results: One week post-operative photographs showed well vascularized graft (Figure 8a) and healing palatal wound (Figure 8b). One and half year postoperative photograph (Figure 9) showed significant root coverage, 85% with 31 and 100% with 41. The tension test was negative and there was significant increase in the width of attached gingiva. Note that the margins of healed graft are nicely blended with the adjacent tissue. Oral prophylaxis was done and oral hygiene instructions reinforced at this stage again and patient is kept under follow-up.
Case-2
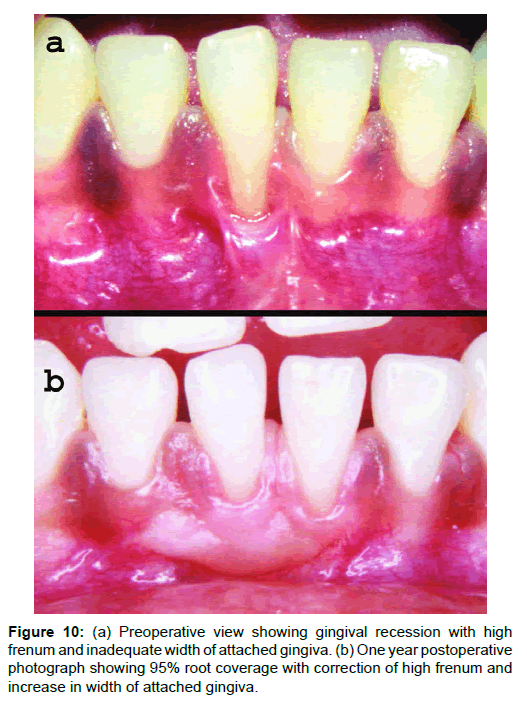
A 23-year-old male patient reported with a complaint of progressive recession with mandibular incisors. On examination tooth 41 was associated with gingival recession of 6mm on labial surface, high frenum and inadequate width of attached gingiva (Figure 10a). Surgical technique for FGG/FMMG was same as described for previous case. One year postoperative photograph (Figure 10b) showed 95% root coverage along with correction of high frenum attachment at the same time increasing the width of attached gingiva.
Discussion
Drawbacks of previous methods for procuring free masticatory mucosal graft, motivated the idea to slightly modify the ivory matrix retainer no. 8 to hold a razor blade and use it as a ‘3A mucotome’. Following advantages were discovered after the clinical application of such a technical modification.
a. Less time consuming: graft can be procured within seconds.
b. Simplicity: Easy to master.
c. Allows greater range of adjustment for the curvature of blade, i.e. initially with the main screw and later with the fingertip or plier.
d. Procured grafts are of relatively uniform thickness and without increase macrolacerations.
e. The graft margins have shallow bevels which can be used as it is or trimmed to obtained butt margins..
A modification of the technique using this mucotome can be applied for procuring connective tissue graft by a ‘double’ trap door technique, similar to that described by Edel [10]. Herein the mucotome is initially moved from mesial to distal direction (cutting edge of blade directed distally). This reflects the partial thickness flap with base of flap distally. Now the cutting edge of blade is directed mesially and blade is engaged in connective tissue and moved from distal to mesial. This gives a connective tissue flap with its base mesially. Incising it at mesial end can then separate the CTG out. The mucosal partial thickness flap is repositioned and sutured. However, the parallel incision and single incision technique for procuring CTG should be preferred as they are not only predictable but also the post operative healing is less traumatic for the patient.
An instrument similar to Paquette knife but with a mechanically oscillating blade for obtaining grafts from a palatal donor site was designed by Mormann et al. [11]. He obtained free gingival graft from a sample of 27 patients and measured the thickness of the graft using Mitotoya thickness measuring gauge. He found that thickness of graft obtained using mucotome ranged from 0.37 to 0.75 mm while that by manual scalpel averaged 0.96 mm. He concluded that graft of intermediate thickness (0.55 mm) showed excellent clinical healing of the donor and recipient site. However, Borghetti and Gardella [12] used thick gingival grafts (1.8 mm) to treat gingival recession. They obtained 85.2% root coverage. Thick grafts yield a higher percentage of root coverage than thin grafts. Even, Holbrook and Ochsenbein [13] modified Miller’s technique. They did not use citric acid and held the thickness of their grafts to about 1.5 mm and got good results. A general belief is that thin, or intermediate-thickness graft (.5-.75 mm) are ideal for increasing the zone of keratinized attached gingiva and undergo minimal primary contraction because of the amount of elastic fibers. For the case of root coverage and ridge augmentation, the ideal thickness of the graft is 1.25 to 2 mm. This is to have minimal secondary contraction but possess greater primary contraction when compared to the thinner graft. The beauty of the mucotome used in the cases described here is that the thickness of the graft can be controlled and one may be able to harvest graft ranging from 0.3 mm to 2.0 mm or more.
Our criterion of success, in addition to root coverage, was the clinical increase in the zone of attached gingiva by the survival of our graft. Postoperatively graft survival could be detected in almost all instances by the lighter color, peculiar to the palatal tissue; differences in the tissue character compared to adjacent areas and the presence of rugae where they existed in the initial donor tissue. Although creeping has been a well known fact, Matter and Cimasoni [14] found that factors such as width of the recession, position of the graft, bone resorption, position of the tooth and hygiene of the patient are certain factors that seem to have a definite influence upon the phenomenon of creeping attachment.
Future studies focused on comparing effectiveness between ‘3A mucotome’, Pacquette knife or any other method could consider variables such as immediate bleeding from donor site, percentage area and speed of epithelization at donor site, graft shrinkage at recipient site and patient related factors such as postoperative pain, bleeding, discomfort, etc.
Conclusion
The free gingival graft is a simple, predictable technique for increasing the zone of attached gingiva. Clinicians interested in performing minor surgical procedures should include the free gingival graft in their armamentarium. The wider range of blade adaptation to the palate was the main thrust of this device. In addition to this, the precise cutting of the instrument and satisfactory control over its movement produced grafts of uniform thickness and without macrolacerations.
Perhaps the use of free gingival graft today is limited, however, it can still be employed in the case of (1) combination of frenulotomy and deepen of vestibule in the pre-prosthetic cases, (2) where other surgical techniques cannot predictably be used to attain an adequate zone of attached gingiva. (3) Inadequate donor connective tissue for subepithelial connective tissue graft, and (4) insufficient width and thickness of keratinized tissue to allow a pedicle procedure to be performed. Most importantly, the wound healing model of the free gingival graft and that of the connective tissue graft are very similar since they are both soft tissue healing. Nevertheless, the free gingival graft procedure is an important adjunct to the periodontal therapy. Optimal success is dependent upon the proper case selection and adherence to the basic principal of grafting. Each case should be individualized and
carefully plan out the technique to achieve optimal result.
Acknowledgement
I would like to thank my guide and mentor Dr. Ramreddy K. Yeltiwar for encouraging me and permitting me to use this device on patients under his supervision.
References
- Bjorn H (1963) Free transplantation of gingiva propria. Odontologisk Revy 14: 321-323.
- Pennel BM, Tabor JC, King KO, Towner JD, Fritz BD,et al. (1969) Masticatory mucosal graft. J Periodontol40: 162-166.
- Nabers JM (1966) Free gingival grafts. Periodontics 4: 243-245.
- Nabers JM (1966) Extension of vestibular fornix utilizing a gingival graft. Periodontics4:77-79.
- Sullivans HC, Atkins JH (1968) Freeautogenous gingival grafts. Principles of successful grafting. Periodontics6:121-129.
- Soehren SE, Allen AL, Cutright D, Seibert JS (1973) Clinical and histologic studies of donor tissues utilized for free grafts of masticatory mucosa. J Periodontol44: 727-741.
- Antonelli JR, Panno FV, Witko A (1998) Inflammatory papillary hyperplasia: supraperiosteal excision by the blade-loop technique. Gen Dent46:390-397.
- Agarwal AA (2011) randomized clinical study to assess the reliability and reproducibility of Sign Grading System. Indian J Dent Res 22:285-290.
- Ibbott CG, Oles RD, Laverty WH (1985) Effects of citric acid treatment on autogenous free graft coverage of localized recession. J Periodontol 56:662-665.
- Edel A (1974) Clinical evaluation of free connective tissue grafts used to increase the width of keratinized gingiva. J ClinPeriodontol1:185-196.
- Mormann W (1978) Free mucosal grafts: a technique for obtaining grafts with a newly developed mucotome (Article in German). DtschZahnarztl Z 33:88-92.
- Borghetti A, Gardella JP (1990) Thick gingival autograft for the coverage of gingival recession: a clinical evaluation. IntJ Periodontics Restorative Dent10:216- 229.
- Holbrook T, Ochsenbein C (1983)Complete coverage of the denuded root surface with a one-stage gingival graft. IntJ Periodontics Restorative Dent 3:8-27.
- Matter J, Cimasoni G (1976) Creeping attachment after free gingival grafts. J Periodontol 47:574-579.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 17578
- [From(publication date):
June-2016 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 16504
- PDF downloads : 1074