Hair Loss and Hirsutism Management
Received: 12-Jul-2018 / Accepted Date: 08-Sep-2017 / Published Date: 29-Sep-2017
Abstract
Hair loss known as alopecia is a major reason for the distress of patients. Patients may present with focal patches of hair loss or more diffuse hair loss, which may include predominant hair thinning or increased hair shedding. On the counterpart, hirsutism is a disorder of excess growth of terminal hairs in androgen-dependent areas in women. Hirsutism, derived from the Latin word “hisutus” means shaggy, rough and bristly, is a common disorder, affecting women. In this review article we discuss about the causes, treatment and prevention of hair loss and hirsutism.
Keywords: Alopecia; Hirsutism; Androgenisation; Trichotillomania; Hyperprolactinaemia
37780Introduction
Alopecia refers to hair loss. It can affect the scalp or other parts of the body, and can be localized or widespread. It may be due to hair shedding, poor quality hair, or hair thinning and can be scarring or non-scarring in nature. Hair grows on most parts of the skin surface, except palms, soles, lips and eyelids. Hair thickness and length varies according to site. Vellus hair is fine, light in color, and short in length. Terminal or androgenic hair is thicker, darker and longer. A hair shaft grows within a follicle at a rate of about 1 cm per month. It is due to cell division at the base of the follicle (hair bulb) [1-5].
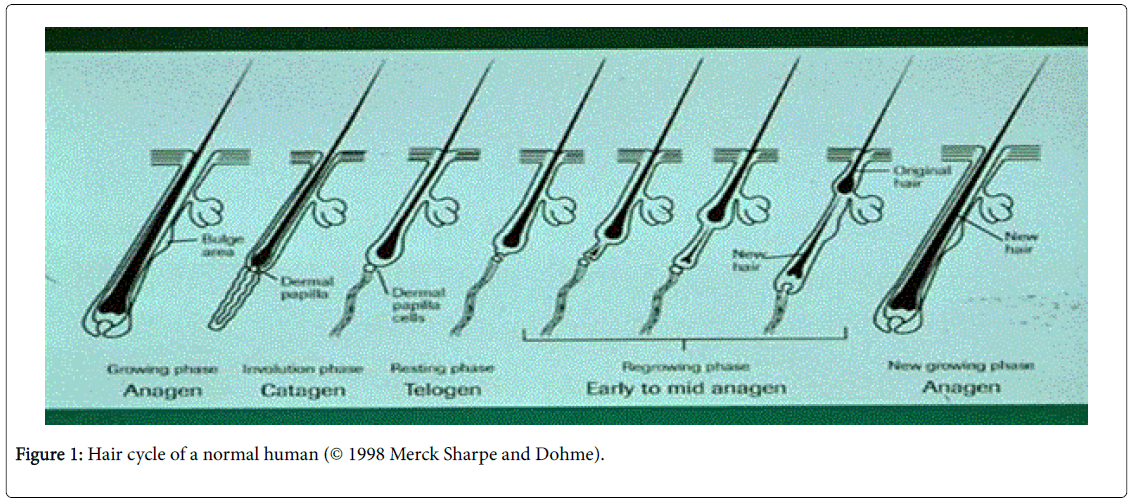
The cells produce the three layers of the hair shaft (medulla, cortex, cuticle), which are essentially made of the protein keratin. Hair growth follows a cycle. However, these phases are not synchronized and any hair may be at a particular phase at random (Table 1).
| Alopecia | Non scarring | Diffuse: Ageing telogen effluvium drug induced |
| Localized: Pattern areata mechanical | ||
| Scarring | Trauma | |
| Lichen planus | ||
| Lupus erythematosus | ||
| Hirsutism | Constitutional | |
| Acquired: Androgenisation and drug induced | ||
Table 1: Causes of alopecia and hirsutism.
The hair cycle can be divided into 3 main phases:
• Anagen: This is actively growing hair.
• Catagen: Transition phase of 2-3 weeks when growth stops and the follicle shrinks.
• Telogen: Resting phase for 1-4 months, up to 10% of hairs in a normal scalp.
Over shedding is known as telogen effluvium. It occurs 2-6 months after an inciting event that stops active hair growth (Table 2). Telogen effluvium is commonly caused by following reasons:
| Physiology | Anagen effluvium |
| Telogen effluvium | |
| Pregnancy | |
| Autoimmune disease | Alopecia areata |
| Pattern thinning of hair | Androgenic |
| Hair shaft abnormalities | Structural Abnormality |
| Medical disease | Inflammatory skin disease |
| Illness, surgery, anaemia, thyroid | |
| Trichotillomania | |
| Cancer treatment |
Table 2: Causes of hair loss.
• Fever, weight loss, pregnancy
• Surgical operation, illness or psychological stress
• Medications (contraceptives, anticoagulants, anticonvulsants)
• Others (unknown)
Shedding can persist for years (chronic telogen effluvium). Scalp hair continues to grow, but has a shorter natural length than normal. Pattern hair loss is due to hormonal influence and increases with age. Male pattern alopecia affects vertex and temporal scalp. Female pattern alopecia affects the anterior scalp. Hair shaft defects can be congenital, or acquired due to disease or injury. Hair shaft abnormalities can be diagnosed by dermatoscopy or more intensive examination of the hair. They include fractures, irregularities, coiling and twisting.
Conditions resulting in reversible patchy hair thinning include:
• Localized alopecia areata.
• Tinea capitis, psoriasis, seborrhoeic dermatitis, atopic dermatitis, pityriasis rubra pilaris, cutaneous lupus erythematosus, cutaneous T-cell lymphoma.
• Generalized skin disease (erythroderma), severe illness, iron, thyroid deficiency.
Hair length depends on the duration of anagen. Short hairs (eyelashes, eyebrows, hair on arms and legs) have a short anagen phase of one month. Anagen lasts up to 6 years or longer in scalp hair. Anagen shedding is known as anagen effluvium and has variable duration and sudden onset. Anagen effluvium is caused by autoimmune disease like severe diffuse alopecia areata, medications like cytotoxic/chemotherapy drugs and congenital condition like loose anagen syndrome (Figure 1).
Scarring alopecia can be due to injury, infections or inflammatory skin diseases. It is secondary to damage of the hair follicle. Infections include viral, bacterial and fungal. Inflammatory skin diseases like lupus, scleroderma and cellulitis can contribute to scarring alopecia. Hair loss can be frustrating, reducing quality of life and causing emotional problems. Loss of normal scalp hair increases the risk of sun related injury.
A careful history and full skin examination can help to identify the cause. Further tests may include, hair pluck test with trichogram to determine relative proportion of anagen and telogen hairs, wood’s lamp examination, swabs of pustules for culture, skin scrapings, hair clippings, blood tests.
Prevention of hair loss is important. It is prudent to stay clear of injury to the hair shaft through lifestyle changes, for example dry your hair with a towel or naturally, reduce chemical treatments and avoid tight hairstyles to reduce mechanical damage. The prognosis for hair loss depends on the cause. Scarring alopecia is irreversible. Anagen and telogen hair loss will cease with time. Early treatment of pattern alopecia can help slow down hair thinning. Finally, treatment of inflammatory disease is essential.
Management Of Hair Loss
It can be divided into surgical and non-surgical measures. Basically, infections and inflammation should be treated; dietary deficiencies fixed and causative drugs have to be stopped [5-7].
Medicine
Medication can be divided into local and systemic. Finasteride is FDA approved medicine for treating male hair loss. It mechanism of action is the stopping of the production of dihydrotestosterone, hence encouraging hair regrowth.
A topical medication for the scalp is 5% Minoxidil. It can stop hair thinning and stimulate hair growth. Concurrent use of a topical retinoid can enhance efficacy. Corticosteroid can be used topically or injected into your scalp to stop the inflammation during conditions like alopecia areata. Alternatives with weak evidence include tacrolimus 0.1% and dithranol and bimatoprost. Bimatoprost has been used to increase eyelash hair in off label us [6,7].
Systemic drugs include immunosuppressant like steroids, ciclosporin, methotrexate, but it is not recommended. Of special mention is a marine protein derivative, Viviscal, which has been FDA approved for hair loss. It is purported to enhance the hair cycle growth phase. Not much is known about the mechanism of action. That said, feedback from my patients have been positive.
Medical devices
Light therapy is safe and used to treat androgenetic alopecia. It is postulated to enhance blood flow in the scalp. It has also been suggested to improve the wound healing process in post hair transplant patients and hasten hair growth. However, the evidence is weak. A multicenter trial reported that male patients with androgenic alopecia exhibited a statistically significant increase in average hair density (p<0.0001) [8].
Similar results were shown in a study comprising women with androgenic alopecia [9]. In a second study of 103 males and 122 females with pattern alopecia that completed the study, HairMax® LaserComb (with 12, 9 and 7 beams) was reported to result in increase in terminal hair density versus trial subjects in the control group [10]. Ongoing trials are investigating the efficacy of other light therapy devices in various types of alopecia [11].
Lifestyle changes
Good scalp care to keep hair clean with stimulating massage, and the safe use of a hair dryer. Maintaining exercise and stress control, eating healthily food rich in protein, vitamins and minerals, like iron. One should avoid birth control pills, anabolic steroids, alcohol and smoking. Finally camouflage with wigs and hair pieces.
Surgical and injectable
Surgical treatment for hair loss will not be discussed in this paper. This can be referred from Sattur SS [12]. Several injectable can be used including:
Platelet Rich Plasma (PRP)
Finally, we should look into PRP. The use of platelet growth factors to stimulate hair growth and reduce hair loss has achieved quite effective results for both androgenic alopecia and alopecia areata, noted in small scale studies [13,14]. We await large scale randomized controlled studies on the use of this modality. This area is indeed promising, but it is clear that with the lack of intellectual property potential, pharmaceutical companies would hesitate to fund a large clinical trial.
Botulinum toxin
The science behind this is the relaxation of scalp musculature, hence decompressing blood vessels in the scalp and increasing oxygen delivery. DHT is converted to estradiol in oxygen rich medium. About a 60 week study has reported increase in hair growth and reduction in hair loss in males with androgenic alopecia [15].
Hirsutism
Hirsutism refers to excessive hair growth in women in a male type pattern. Hirsutism can involve a single site or multiple sites (Table 3).
| Facial hair | Moustache, beard, eyebrows |
| Abdomen | Diamond shape of pubic hair extending to umbilicus |
| Chest | Around nipples or more extensive growth |
| Upper back | Around the upper back areas |
| Inner thighs | Around the inner area of thighs |
Table 3: Sites of hirsutism.
A hirsute pattern of hair growth is usually pre-determined genetically. The degree varies across culture, ethnicity and race. Late onset hirsutism may be due to hyperandrogenism. Hyperandrogenism is often associated with polycystic ovaries, insulin resistance and obesity. Rare causes include, androgenic medications, congenital adrenal hyperplasia, tumor of adrenal gland or ovary and Cushing’s syndrome (Table 4) [16-19].
| Hyperandrogenism | Polycystic ovaries |
| Androgen medications | |
| Congenital adrenal hyperplasia | |
| Tumor of adrenal gland or ovary | |
| Cushing’s syndrome | |
| Increase androgen sensitivity | Insulin resistance |
| Obesity |
Table 4: Causes of hirsutism.
Different genes expressed in individual hair follicles vary in their response to androgens. Hair follicles in the secondary hair growth sites are more sensitive to androgens than those in other areas. Severity of hirsutism is assessed using the Ferriman-Gallwey visual scale or a modified version, which assesses 9 areas of the body.
• The score varies from 0 (no hair) to 4 (extensive hair growth) in each area.
• Total score<8: Normal hair growth.
• Total score 8-14: Mild hirsutes.
• Total score ≥ 15: Moderate to severe hirsutes.
General examination may point to the cause of hirsutism. Acanthosis nigricans suggests insulin resistance. Galactorrhoea suggests hyperprolactinaemia. Purple striae, thin skin, bruising and facial plethora suggest Cushing syndrome. Virilisation suggests hyperandrogenism. Signs include deepening voice, balding, acne, decrease in breast size, increased muscle bulk. Diagnostic features for polycystic ovary syndrome include signs of hyperandrogenism, oligo or anovulation and the pressure of sizeable follicles in each ovary, increased ovarian volume on ultrasound. Hirsutism is diagnosed clinically. Investigations are not usually necessary, unless a Ferriman- Gallwey score of >15. Blood tests are done to evaluate male hormone levels and underlying diseases. This can be followed by ovarian ultrasound scan.
Management Of Hirsutism
Management of hirsutism can be divided into mechanical and medical methods (Table 5).
| Temporary removal | Temporary to permanent reduction | Permanent removal |
| Shaving | Laser assisted | Electrolysis |
| Chemical depilation | Intense Pulse light | |
| Physical Epilation |
Table 5: Techniques of hair removal.
Mechanical treatment
Depilatory creams commonly contain thioglycolate, and can irritate skin. Shaving is another option. Waxing would need to be done every six weeks. All these carry a risk of folliculitis, which may take time to settle. Electrolysis or thermolysis consists of a small probe inserted along each hair, and a small electrical discharge destroys the hair. This carries a risk of scarring. Lasers and intense pulsed light are the most effective devices for hair removal. The long pulse 1064 nm ND Yag laser is ideal for darker skin patients Fitzpatrick 4 to 6, while the 755 nm alexandrite and IPL can be used for lighter skin types. Multiple treatments are required, spaced weeks apart [20-24].
Medical treatment of hirsutism
This can be Metformin or rosiglitazone can be prescribed to women with polycystic ovarian syndrome. Hormonal treatment with antiandrogen medicines may be used for women with hirsutism. Effects may take 6-12 months, and the medicine needs to be continued for years. Spironolactone can reduce excessive hair growth. A synergistic effect is achieved when combined with the contraceptive pill. Combined birth control pills that contain estrogen and progesterone: cyproterone are effective. Side effects include mood swings, loss of libido and weight gain.
Conclusion
In the realm of hair loss, low level light therapy is a fascinating area deserving of further research. With the interest in non-invasive treatments growing, personally I believe combination therapy with minoxidil, anti-androgens and low level light therapy would be the gold standard treatment for hair loss in the future. As for hirsutism, it is not yet possible to prevent a genetically predetermined cause. Insulin resistance associated with obesity can be reduced by diet and lifestyle changes. Prognosis is dependent on the cause. The most common types of excessive hair growth is permanent. Hirsutism has a tendency to worsen with age.
References
- Mounsey AL, Reed SW (2009) Diagnosing and treating hair loss. Am Fam Physician 80: 356-362.
- Nalluri R, Harries M (2016) Alopecia in general medicine. Clinical Medicine 16: 74-78.
- Mubki T, Rudnicka L, Olszewska M, Shapiro J (2014) Evaluation and diagnosis of the hair loss patient: Part I. J Am AcadDermatol 71: 415e1-e15.
- Franca K, Rodrigues TS, Ledon J, Savas J, Chacon A (2013) Comprehensive overview and treatment update on hair loss. J. Cosmetics, Dermatological Sciences and Applications 3: 1.
- Gordon KA, Tosti A (2011) Alopecia: Evaluation and treatment. ClinCosmetInvestigDermatol 4: 101-106.
- Ohyama M (2010) Management of hair loss diseases. Dermatologicasinica 28: 139-145.
- Rogers NE, Avram MR (2008) Medical treatments for male and female pattern hair loss. J Am AcadDermatol 4: 547-566.
- Leavitt M, Charles G, Heyman E, Michaels D (2009) HairMaxLaserComb laser phototherapy device in the treatment of male androgenetic alopecia: A randomized, double-blind, sham device-controlled, multicentretrial. Clin Drug Investig 5:283-292.
- Jimenez JJ, Wikramanayake TC, Bergfeld W, Hordinsky M, Hickman JG, et al. (2014) Efficacy and safety of a low-level laser device in the treatment of male and female pattern hair loss: a multicenter, randomized, sham device-controlled, double-blind study. Am J ClinDermatol 2: 115-127.
- Kalia S, Lui H (2013) Utilizing electromagnetic radiation for hair growth: A critical review of phototrichogenesis. DermatolClin 1:193-200.
- Sattur SS (2011) A review of surgical methods (excluding hair transplantation) and their role in hair loss management today. J CutanAesthetSurg 2: 89-97.
- Trink A, Sorbellini E, Bezzola P, Rodella L, Rezzani R, et al. (2013) A randomized, double-blind, placebo-and active-controlled, halfâ€head study to evaluate the effects of plateletâ€rich plasma on alopecia areata. Br J Dermatol 169: 690-694.
- Schiavone G, Raskovic D, Greco J, Abeni D (2014) Platelet-rich plasma for androgenetic alopecia: A pilot study. DermatolSurg 40: 1010-1019.
- Freund BJ, Schwartz M (2010) Treatment of male pattern baldness with botulinum toxin: A pilot study. PlastReconstrSurg 126: 246e-248e.
- Karasu T, Metwally M (2015) Hirsutism. ObstetGynaecolReprod Med 25: 213-216.
- Escobar HF, Carmina E, Dewailly D, Gambineri A, Kelestimur F, et al. (2012) Epidemiology, diagnosis and management of hirsutism: A consensus statement by the androgen excess and polycystic ovary syndrome society. Hum Reprod Update 18: 146-170.
- Dash K (2013) Evaluation and treatment of hirsutism. Apollo Medicin 10:138-145.
- Somani N, Harrison, S, Bergfeld WF (2008) The clinical evaluation of hirsutism. DermatolTher21: 376-391.
- Tremaine AM, Avram MM (2015) FDAMAUDE data on complications with lasers, light sources, and energy-based devices. Lasers Surg Med47: 133-140.
- Babilas P, Schreml S, Szeimies RM, Landthaler M (2010) Intense pulsed light (IPL): A review. Lasers Surg Med 42: 93-104.
- Dierickx CC (1999) Laser Hair Removal: Scientific principles and practical aspects. Coherent Medical pp: 1-8.
- Lepselter J,Elman M (2004) Biological and clinical aspects in laser hair removal. J Dermatolog Treat 15: 72-83.
Citation: Chang D (2017) Hair Loss and Hirsutism Management. Cosmetol & Oro Facial Surg 3: 120.
Copyright: © 2017 Chang D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 9857
- [From(publication date): 0-2017 - Nov 30, 2024]
- Breakdown by view type
- HTML page views: 9135
- PDF downloads: 722