Guillain-Barre Syndrome associated SARS-CoV-2: What Poses Less Risk, Vaccinate or Infected with COVID?
Received: 14-Mar-2022 / Manuscript No. JIDT-22-57034 / Editor assigned: 16-Mar-2022 / PreQC No. JIDT-22-57034(PQ) / Reviewed: 30-Mar-2022 / QC No. JIDT-22-57034 / Revised: 06-Apr-2022 / Manuscript No. JIDT-22-57034(R) / Published Date: 14-Apr-2022
Abstract
Introduction: Among the neurological diseases possibly associated with COVID-19 (coronavirus disease 2019) infection, Guillain-Barre syndrome has been postulated since the start of the pandemic, even more so when vaccination has also come into play.
Objectives: A bibliographic review is carried out to assess the true risks of suffering Guillain-Barre syndrome secondary to vaccination against SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) infection and of developing it secondary to SARS-CoV-2 infection.
Materials and methods: A search for articles was carried out in the PubMed-MEDLINE database between June 2021 and July 2021.
Results: The scarcity of studies that can provide solid evidence stands out, with most of the publications being clinical case reports or case series. Two epidemiological studies with contradictory results stand out.
Conclusion: With the information currently available, it is not possible to conclude that there is an association between SARS-CoV-2 infection or secondary to vaccination with Guillain-Barre syndrome. Therefore, the recommendation to avoid vaccination for fear of a recurrence of Guillain-Barre syndrome does not seem to be normative at the present time.
Keywords: COVID-19; SARS-CoV-2; Guillain-Barre syndrome; Pandemic; Causality
Introduction
From the first moments of the COVID-19 pandemic (coronavirus disease 2019), there began to be a concern about the possible subsequent appearance of Guillain-Barre syndrome, in a similar way to what happens with other respiratory viruses (especially with Mycoplasma Pneumonia or the influenza virus) [1,2], in which case a second parallel pandemic would be generated. In the midst of the oversaturation of the health systems of practically all the countries of the world, it was difficult to be able to collect data that would early generate solid evidence on the possible association of these two entities, as well as the association of the infection by SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) and any other neurological process.
The COVID-19 vaccine race to curb the virulence of this pandemic pathogen suggested another question: Could these vaccines also be a cause of Guillain-Barre syndrome? And if so, how would you be less likely to develop it, secondary to direct infection or secondary to vaccination?
Medical consultations received questions from patients who had previously suffered Guillain-Barre syndrome, and who had been informed at the time that the cause could be related to a vaccine or some type of infection in the previous weeks. "Doctor, is vaccination safe for me?"
The only possible solution to this type of question would be to take one of the following ways: referring the patient to the Preventive Medicine Service, where the uncertainty was probably not resolved either; to expose a personal point of view neither based on evidence nor experience, given the rapid development of events; or, to confess simply the lack of serious knowledge about it.
Objectives
The objective of this work is to carry out a review that allows estimating the risk of suffering Guillain-Barre syndrome secondary to vaccination against SARS-CoV-2 infection, respect to developing it secondary to SARS-CoV-2 infection.
Materials and Methods
A search for articles was carried out in the PubMed-MEDLINE database between June 2021 and July 2021. The keywords used on the one hand were "COVID-19" or "SARS-CoV-2", and "Guillain-Barre", using the Boolean operator “AND”; on the other hand, “COVID-19” or “SARS-CoV-2”, and “Guillain-Barre” and “vaccine” were used, using the Boolean operator “AND” in each case.
The exclusion criteria were those articles not written in English or Spanish, or those that did not deal with humans (for example, research articles on animal models). The PRISMA guideline was taken into account for systematic reviews [3].
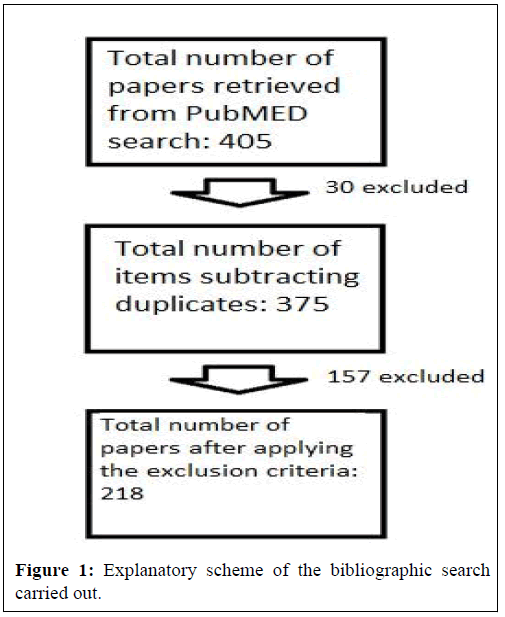
A total of 405 results were obtained, of which 30 were duplicates, resulting in 375 results, and applying the exclusion criteria, the total number of assessable articles was 218 (Figure 1). Of these, 6 corresponded to meta-analyses, 63 corresponded to reviews, and 24 to systematic reviews.
Results
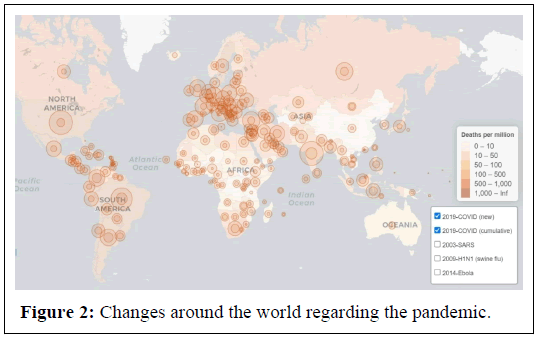
In the first place, the number of published case reports stands out [4-10], on presumed Guillain-Barre syndrome secondary to COVID-19 infection, including the Miller-Fisher syndrome variant [11]; from case series [12-15]; as well as letters to the director or to the editor [16,17], through which it is not possible to establish strong evidence of a causal relationship given the absence of any type of statistical analysis, even more so considering the high prevalence (cumulative incidence in June 2021 of more than 170,000,000 cases worldwide) of SARS-CoV-2 infection in the areas where these cases occurred (Figure 2), thus not being able to rule out the hypothesis that it was actually a simple coincidence of two relatively frequent pathologies [18,19].
In addition, it is important to be able to adequately differentiate, in the case of patients affected by severe pneumonia, between critically ill neuropathy and Guillain-Barre syndrome, given the possible semiological overlap [20], especially considering that not all reported cases shows differentiating signs such as the classic albumincytological dissociation in cerebrospinal fluid [21].
As well as in many cases the typical latency time period of approximately 3 weeks from the causal infection and the appearance of neurological symptoms did not exist. For this reason, various sources call it early Guillain-Barre syndrome [22], and it is necessary to take into account the very possible diagnostic confusion.
However, the systematic reviews carried out do show a strong association between both pathologies, in addition, the studies analyzed emphasize differences in the presentation of the disease with greater severity in Guillain-Barre syndrome associated with COVID-19 [23], compared to those described associated with other causes. In addition, an Italian multicenter observational study was published that showed an increase in the incidence of Guillain-Barre syndrome from the start of the pandemic in northern Italy [24], supporting the existence of a link with this pathogen. They also agreed on the aforementioned observation that it usually presents more seriously than in cases precipitated by other causes. However, the confidence intervals overlapped due to the small sample size, and this small increase from previous years could be due to a chance finding [25].
To add even more confusion, we have a paper published in December 2020 [26], which shows the results of a cohort study that found no association at all between Guillain-Barre syndrome and COVID-19 infection. The authors also did not find significant differences in the cases diagnosed during the pandemic, in terms of the pattern of weakness, latency time, neurophysiological patterns or findings in cerebrospinal fluid, compared to the cases diagnosed in the previous 3 years. Moreover, they corroborate a decrease in the incidence during the pandemic, which they explain as a consequence of the confinement measures adopted by the authorities, which would reduce the transmission of pathogens that induce Guillain-Barre syndrome, such as respiratory viruses or Campylobacter jejuni.
Generally, when measured, COVID-19 antibodies could not be determined in cerebrospinal fluid, except in one case [27]. The viral amino acid sequence has been compared with human auto antigens associated with immune-mediated polyneuropathies, showing that the peptides that comprise the immunoreactive epitopes of SARS-CoV-2 share the same sequence as heat shock proteins 90 and 60 that are associated with Guillain-Barre syndrome [28-30]. However, anti-ganglioside antibodies have only been detected very infrequently in some cases of Guillain-Barre syndrome associated with COVID-19 [31].
Regarding vaccination, the information we currently have is even scarcer than in the previous case, and even, of lower quality, highlighting some isolated case report published [32], some letter to the editor [33], and a study conducted in India [34], in which 80% of the population of Kerala (India) had received the ChAdOx1-S/ nCoV-19 vaccine. A period of 4 weeks (from March to April 2021) was evaluated in this population, observing 7 cases of Guillain-Barre syndrome, the incidence was therefore 1.4 to 10 times higher than that expected for such a period in a population of this magnitude. Guillain- Barre syndrome was also more severe, and the patients had frequently facial diplegia, a phenotype normally associated with post-vaccination Guillain-Barre syndrome [35].
On July 12, 2021, the FDA (Food and Drug Administration) referred that the Ad26.CoV-2.S (Janssen/Johnson & Johnson) vaccine registered an "increased risk" of Guillain-Barre syndrome. 100 cases were identified after the administration of 12.5 million doses of the vaccine. When making a critical reading, it is necessary to consider that if 4,000,000,000 people are immunized during a year, it would be expected that 68,000 cases of Guillain-Barre syndrome would occur naturally within this period, regardless of vaccination. Of these Guillain-Barre syndrome cases, 13,076 would occur in the 10-week window after double-dose vaccination with injections 4 weeks apart [36], which is even more than a hundred times more cases than reported by the FDA.
Therefore, weightier, serious, epidemiological studies that may or may not demonstrate a real association are lacking.
Discussion
Although there are many publications regarding Guillain-Barre syndrome and its possible relationship with COVID-19, however, we can observe the lack of strong sources of evidence. Moreover, when we come across structured epidemiological studies such as the one carried out by Keddie et al., we can see how this association is at least doubtful.
In the theoretical field, the hypothesis seemed consistent that SARS-CoV-2, as occurs with other respiratory viruses, and also as hypothesized in relation to other coronaviruses in the past [37,38], could trigger the appearance of a syndrome of Guillain-Barre, however, establishing evidence in this regard is an arduous task, especially taking into account the overflow of systems, the reorganization of medical services, and the high incidence of infections that a pandemic implies, with the consequent coincidence or co-occurrence of events. In addition, it is difficult to report possible specific adverse reactions due to the administration of a vaccine, when the entire population is vaccinated.
Although it may still be premature to rule out the association between the SARS-CoV-2 virus and the appearance of Guillain-Barre syndrome, however, it seems risky to assume this association as well. We have conflicting data at the present time, and, prudence in making judgments about it, will further aid scientific progress.
Without a doubt, it is important to carry out more systematic, epidemiological, prospective studies that assess cohorts with patients with different degrees of involvement secondary to the COVID-19 infection, as well as healthy, unexposed cohorts. Only in this way will it be possible to provide high, solid and reliable evidence to help clinical practice in the near future. Also when making consistent recommendations to patients [39-41].
Conclusion
There are still many questions to be resolved regarding this intricate subject. The sources of evidence, even with a large volume of publications, are still poor. With the current data, an association between COVID-19 infection and Guillain-Barre syndrome cannot be assumed, nor between vaccination against SARS-COV-2 and Guillain- Barre syndrome; In both cases, however, if cause-effect existed, the pathophysiological mechanism would be the same, by means of cross-immunity due to the similarity between a sequence of the antigenic proteins of the virus and the gangliosides or other regions of the peripheral nerve. It is striking, however, at the observational level that we are not facing a Guillain-Barre syndrome pandemic as would be expected if it were a strong association, either secondary to an infection as prevalent as COVID-19, or secondary to a vaccination that in some countries borders on proportions close to 100%.
When faced with a patient who doubts whether or not to be vaccinated, or with a patient who has already suffered from Guillain- Barre syndrome secondary to vaccination, even recurrently, there are no great recommendations based on the evidence that we currently have, except perhaps that there is no compelling reason, in relation to Guillain-Barre syndrome, not to be vaccinated.
References
- Meyer Sauteur PM, Huizinga R, Tio‐Gillen AP, Roodbol J, Hoogenboezem T, et al. (2016) Mycoplasma pneumoniae triggering the Guillain‐Barré syndrome: A case‐control study. Ann Neurol 80:566-580.
[Crossref] [Google Scholar] [PubMed]
- Vellozzi C, Iqbal S, Broder K (2014) Guillain-Barre syndrome, influenza, and influenza vaccination: The epidemiologic evidence. Clin Infect Dis 58:1149-1155.
[Crossref] [Google Scholar] [PubMed]
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 151:264-269.
[Crossref] [Google Scholar] [PubMed]
- El Otmani H, El Moutawakil B, Rafai MA, El Benna N, El Kettani C, et al. (2020) COVID-19 and Guillain-Barre syndrome: more than a coincidence!. Rev Neurol 176:518-519.
[Crossref] [Google Scholar] [PubMed]
- Paybast S, Gorji R, Mavandadi S (2020) Guillain-Barre syndrome as a neurological complication of novel COVID-19 infection: A case report and review of the literature. Neurologist 25:101-103.
[Crossref] [Google Scholar] [PubMed]
- Sedaghat Z, Karimi N (2020) Guillain Barre syndrome associated with COVID-19 infection: A case report. J Clin Neurosci 76:233-235.
[Crossref] [Google Scholar] [PubMed]
- Carrillo-Larco RM, Altez-Fernandez C, Ravaglia S, Vizcarra JA (2020) COVID-19 and Guillain-Barre syndrome: A systematic review of case reports. Wellcome Open Res 2020; 5:107.
[Crossref] [Google Scholar] [PubMed]
- Scheidl E, Canseco DD, Hadji‐Naumov A, Bereznai B (2020) Guillain‐Barr é syndrome during SARS‐CoV‐2 pandemic: A case report and review of recent literature. J Peripher Nerv Syst 25:204-207.
[Crossref] [Google Scholar] [PubMed]
- Virani A, Rabold E, Hanson T, Haag A, Elrufay R, et al. (2020) Guillain-Barré syndrome associated with SARS-CoV-2 infection. ID Cases 20: 00771.
[Crossref] [Google Scholar] [PubMed]
- Camdessanche JP, Morel J, Pozzetto B, Paul S, Tholance Y, et al. (2020) COVID-19 may induce Guillain–Barré syndrome. Rev Neurol 176:516-518.
[Crossref] [Google Scholar] [PubMed]
- Gutiérrez-Ortiz C, Méndez-Guerrero A, Rodrigo-Rey S, San Pedro-Murillo E, Bermejo-Guerrero L, et al. (2020) Miller Fisher syndrome and polyneuritis cranialis in COVID-19. Neurology 95:601-605.
[Crossref] [Google Scholar] [PubMed]
- Abu-Rumeileh S, Abdelhak A, Foschi M, Tumani H, Otto M (2021) Guillain-Barre syndrome spectrum associated with COVID-19: an up-to-date systematic review of 73 cases. J Neurol 268:1133-1170.
[Crossref] [Google Scholar] [PubMed]
- Alberti P, Beretta S, Piatti M, Karantzoulis A, Piatti ML, et al. (2020) Guillain-Barre syndrome related to COVID-19 infection. Neurol Neuroimmunol Neuroinflamm 7:741.
[Crossref] [Google Scholar] [PubMed]
- Arnaud S, Budowski C, Tin SN, Degos B (2020) Post SARS-CoV-2 Guillain-Barré syndrome. Clin Neurophysiol 131:1652-1654.
[Crossref] [Google Scholar] [PubMed]
- Bigaut K, Mallaret M, Baloglu S, Nemoz B, Morand P, et al. (2020) Guillain-Barre syndrome related to SARS-CoV-2 infection. Neurol Neuroimmunol Neuroinflamm 7:785.
[Crossref] [Google Scholar] [PubMed]
- Joob B, Wiwanitkit V (2020) COVID-19 and Guillain-Barré syndrome. Rev Neurol 176:637.
[Crossref] [Google Scholar] [PubMed]
- Toscano G, Palmerini F, Ravaglia S, Ruiz L, Invernizzi P, et al. (2020) Guillain-Barre syndrome associated with SARS-CoV-2. N Engl J Med 382:2574-2576.
[Crossref] [Google Scholar] [PubMed]
- Carod-Artal FJ (2020) Neurological complications of coronavirus and COVID-19. Rev Neurol 70:311-322.
[Crossref] [Google Scholar] [PubMed]
- Zhao H, Shen D, Zhou H, Liu J, Chen S (2020) Lancet Neurol 19:383-384.
[Crossref] [Google Scholar] [PubMed]
- Toscano G, Palmerini F, Ravaglia S, Ruiz L, Invernizzi P, et al. (2020) Guillain–Barré syndrome associated with SARS-CoV-2. N Engl J Med 382:2574-2576.
[Crossref] [Google Scholar] [PubMed]
- Whittaker A, Anson M, Harky A (2020) Neurological manifestations of COVID‐19: A systematic review and current update. Acta Neurol Scand 142:14-22.
[Crossref] [Google Scholar] [PubMed]
- Ottaviani D, Boso F, Tranquillini E, Gapeni I, Pedrotti G, et al. (2020) Early Guillain-Barré syndrome in coronavirus disease 2019 (COVID-19): A case report from an Italian COVID-hospital. Neurol Sci 41:1351-1354.
[Crossref] [Google Scholar] [PubMed]
- Gittermann LT, Feris SV, von Oetinger Giacoman A (2020) Relation between COVID-19 and Guillain-Barré syndrome in adults. Systematic review. Neurologia 35:646-654.
[Crossref] [Google Scholar] [PubMed]
- Filosto M, Piccinelli SC, Gazzina S, Foresti C, Frigeni B, et al. (2021) Guillain-Barré syndrome and COVID-19: an observational multicentre study from two Italian hotspot regions. J Neurol Neurosurg Psychiatry 92:751-756.
[Crossref] [Google Scholar] [PubMed]
- Lunn MP, Cornblath DR, Jacobs BC, Querol L, van Doorn PA, et al. (2021) COVID-19 vaccine and Guillain-Barre syndrome: let’s not leap to associations. Brain 144:357-360.
[Crossref] [Google Scholar] [PubMed]
- Keddie S, Pakpoor J, Mousele C, Pipis M, Machado PM, et al. (2021) Epidemiological and cohort study finds no association between COVID-19 and Guillain-Barré syndrome. Brain 144:682-693.
[Crossref] [Google Scholar] [PubMed]
- Gigli GL, Vogrig A, Nilo A, Fabris M, Biasotto A, et al. (2020) HLA and immunological features of SARS-CoV-2-induced Guillain-Barré syndrome. Neurol Sci 41:3391-3394.
- Lucchese G, Flöel A (2020) SARS-CoV-2 and Guillain-Barre syndrome: molecular mimicry with human heat shock proteins as potential pathogenic mechanism. Cell Stress Chaperones 25:731-735.
[Crossref] [Google Scholar] [PubMed]
- Venkatakrishnan AJ, Kayal N, Anand P, Badley AD, Church GM, et al. (2020) Benchmarking evolutionary tinkering underlying human–viral molecular mimicry shows multiple host pulmonary–arterial peptides mimicked by SARS-CoV-2. Cell Death Discov 6:96.
[Crossref] [Google Scholar] [PubMed]
- Kanduc D (2020) From anti-SARS-CoV-2 immune responses to COVID-19 via molecular mimicry. Antibodies 9:33.
[Crossref] [Google Scholar] [PubMed]
- Caress JB, Castoro RJ, Simmons Z (2020) COVID-19-associated Guillain-Barré syndrome: The early pandemic experience. Muscle Nerve 62:485-491.
[Crossref] [Google Scholar] [PubMed]
- Hasan T, Khan M, Khan F, Hamza G (2021) Case of Guillain-Barre syndrome following COVID-19 vaccine. BMJ Case Rep 14:243629.
[Crossref] [Google Scholar] [PubMed]
- Aomar-Millán IF, de Victoria-Carazo JM, Peregrina-Rivas JA, Villegas-Rodríguez I (2021) COVID-19, Guillain-Barré syndrome, and the vaccine. A dangerous combination. Rev Clin Esp 221:555-557.
[Crossref] [Google Scholar] [PubMed]
- Maramattom BV, Krishnan P, Paul R, Padmanabhan S, Cherukudal Vishnu Nampoothiri S, et al. (2021) Guillain-Barre Syndrome following ChAdOx1-S/nCoV-19 Vaccine. Ann Neurol 90:312-314.
[Crossref] [Google Scholar] [PubMed]
- Masucci EF, Kurtzke JF (1971) Diagnostic criteria for the Guillain-Barré syn-drome. An analysis of 50 cases. J Neurol Sci 13:483-501.
- Lunn MP, Cornblath DR, Jacobs BC, Querol L, Van Doorn PA, et al. (2021) COVID-19 vaccine and Guillain-Barré syndrome: let's not leap to associations. Brain 144:357-360.
[Crossref] [Google Scholar] [PubMed]
- Tsai LK, Hsieh ST, Chao CC, Chen YC, Lin YH, et al. (2004) Neuromuscular disorders in severe acute respiratory syndrome. Arch Neurol 61:1669-1673.
[Crossref] [Google Scholar] [PubMed]
- Montalvan V, Lee J, Bueso T, De Toledo J, Rivas K (2020) Neurological manifestations of COVID-19 and other coronavirus infections: A systematic review. Clin Neurol Neurosurg 194:105921.
[Crossref] [Google Scholar] [PubMed]
- Willison HJ, Jacobs BC, Van Doorn PA (2016) Guillain-Barre syndrome. Lancet 388:717-727.
[Crossref] [Google Scholar] [PubMed]
- Kaida K (2019) Guillain-Barre Syndrome. Adv Exp Med Biol 1190:323-331.
[Crossref] [Google Scholar] [PubMed]
- Roper TA, Alani SM (1995) Recurrent Guillain-Barre syndrome: lightning does strike twice. Br J Hosp Med 53:403-407.
Citation: Gallego MDC (2022) Guillain-Barre Syndrome associated SARS-CoV-2: What Poses Less Risk, Vaccinate or Infected with COVID? J Infect Dis Ther. S3:001.
Copyright: © 2022 Gallego MDC. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 960
- [From(publication date): 0-2022 - Nov 21, 2024]
- Breakdown by view type
- HTML page views: 752
- PDF downloads: 208