Case Report Open Access
Gorhams Disease of a Mandible: A Case Report
Norliwati Ibrahim1*, Nurshaline Pauline Kipli2, Ahmad Toha3 and Rosli Ismail41Department of Oral Medicine and Oral Pathology, Faculty of Dentistry, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
2Dental Specialist Clinic, Sarawak General Hospital, Kuching, Sarawak, Malaysia
3Department of Pathology, Hospital Raja Permaisuri Bainun, Ipoh, Perak, Malaysia
4Pantai Hospital Ayer Keroh, Melaka, Malaysia
- *Corresponding Author:
- Dr. Norliwati Ibrahim
BDS MClinDent, Lecturer at the Department of Oral
Medicine and Oral Pathology, Faculty of Dentistry
Universiti Kebangsaan Malaysia, Malaysia
Tel: 60392897998
Fax: 60392897798
E-mail: norliibrahim@gmail.com
Received date: October 19, 2015; Accepted date: December 28, 2015; Published date: December 31, 2015
Citation: Ibrahim N, Kipli NP, Toha A, Ismail R (2015) Gorham’s Disease of a Mandible: A Case Report. Cosmetol & Oro Facial Surg 1:103. doi:10.4172/jcofs.1000103
Copyright: © 2015 Ibrahim N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Cosmetology & Oro Facial Surgery
Abstract
Gorham’s disease is a rare disorder characterized by progressive bone destruction and proliferation of vascular channels with replacement of fibrous connective tissue. The aetiology remains poorly understood while both diagnosis and management were challenging. We reported a case of an 18 year-old Ibanese girl of Sarawak with massive mandible destruction, whom initial complaint was gingival swelling of the right mandible with affected teeth mobility.
Keywords
Gorham’s disease; Gorham-stout disease; Disappearing bone disease; Immunohistochemistry
Introduction
Gorham’s disease is a rare bone disorder characterized by massive and spontaneous osteolysis where the bone is destroyed by osteolysis and does not regenerate or repair. Instead, it is replaced by dense fibrous tissue with the eventual disappearance of the bone. This disease is also known as the Gorham-Stout disease, disappearing bone disease, vanishing bone disease or massive osteolysis.
In 1838, Jackson [1] was the first to describe a different entity of multiple osteolysis in an 18-year-old male whose humerus slowly and completely resorbed following a fracture. Then, in 1954 it was reported by Gorham [2], and subsequently in the following year by Gorham and Stout who reviewed the first 24 cases and defined it as a specific pathologic entity [3].
The disease is extremely rare with less than 200 cases reported. Moller reported approximately 175 cases whereas Holroyd reported only 140 cases were seen since 1838. The first facial case was described by Römer in 1928 and to date 37 out of 41 maxillofacial cases were in mandible as reviewed by Escande [4].
Clinically, patients were usually young adults, but it may involve a wide age range from birth to 75 years of age. Symptoms depending on the area involved although pain or pathologic fracture are the usual clinical presentations. The diagnosis is established by exclusion, where patients show unremarkable biochemistry and haematology findings, radiographic evident of osteolytic lesions in association with histological proliferation of capillary and small lymphatic vessels [5].
We report here a case of a young lady with massive destruction of her mandibular jaw bone. The main concern of this case report is the prevention of disease progression because progression from the mandible to the maxilla, skull, and spine has been reported [1].
Report of a case
The patient is an 18-year-old Ibanese girl from Sarawak who complained of a swelling on her right lower gum in March 2009. It started approximately 3 months from the first dental visit where she noted an increase in size but generally painless gingival swelling. She reported a toothache-like pain prior to the swelling but there was no bleeding or pus seen. She had cervical tuberculosis infection of a cervical region about 2 years ago but had no history of cough or pulmonary symptoms. She completed her antituberculous treatment a year after being diagnosed. She has no other medical problem nor allergy to any medication and no history of previous trauma.
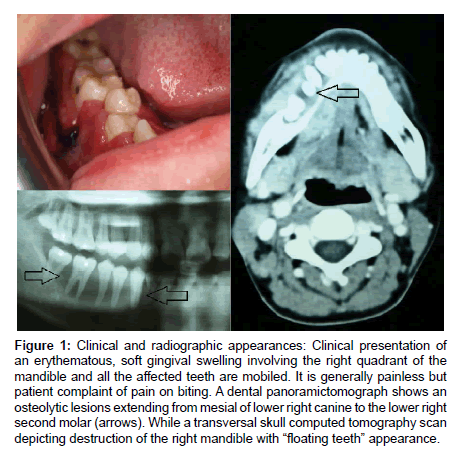
Upon examination, there were bilateral palpable submandibular lymph nodes with no obvious facial swelling. Intraorally, there was a diffuse lower right gingival swelling extending from the mesial of lower right canine to the lower right second molar and a bucco-lingual soft tissue expansion (Figure 1). Dental examination revealed all teeth to be vital and free of caries.The involved teeth on the right mandible were mobile and the gingiva was soft, fluctuant and erythematous, non tender to palpation but painful on biting. Biochemical and hematology tests were within normal range.
Radiographically, panoramic dental tomograph, revealed bone resorption extending from the lower right canine to the lower right second molar with involvement of the apex and bifurcation areas resulting in the appearance of ‘floating teeth’ (Figure 1). Computed tomography (CT) scan revealed an aggressive lesion in the right mandible with local soft tissues extension and cervical lymphadenopathy (Figure 1).
Figure 1: Clinical and radiographic appearances: Clinical presentation of an erythematous, soft gingival swelling involving the right quadrant of the mandible and all the affected teeth are mobiled. It is generally painless but patient complaint of pain on biting. A dental panoramictomograph shows an osteolytic lesions extending from mesial of lower right canine to the lower right second molar (arrows). While a transversal skull computed tomography scan depicting destruction of the right mandible with “floating teeth” appearance.
Histopathology findings
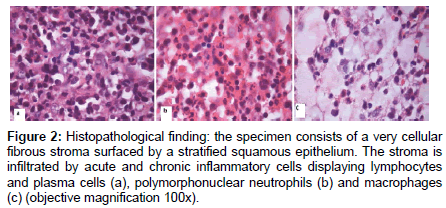
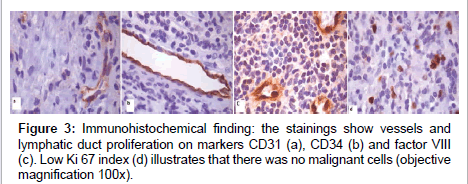
An incisional biopsy under general anaesthesia was done and histopathology report discovered a reactive plasmacytosis for the affected gingival lesion while the submental lymph nodes swelling showed a reactive lymphoid tissues. The subsequent incisional biopsy and curretage with removal of all the lower right dentition was done and resulted in a non-specified acute into chronic inflammatory lesion (Figure 2). In addition, there was no granuloma seen in the sections examined and this excluded tuberculosis infection. Immunohistochemical stainings demonstrate evidence of blood and lymphatic vessels proliferation (Figure 3).
Figure 2: Histopathological finding: the specimen consists of a very cellular fibrous stroma surfaced by a stratified squamous epithelium. The stroma is infiltrated by acute and chronic inflammatory cells displaying lymphocytes and plasma cells (a), polymorphonuclear neutrophils (b) and macrophages (c) (objective magnification 100x).
Follow-up
A 3-month review post-operatively showed no progression of the lesion on the right mandibular region. Nevertheless, a small lytic lesion was distinguished on the right maxilla around the second molar tooth. A one-year review also showed that there was no disease progression and the radiolucency noted around the right upper second molar has remained the same. Patient is currently wearing lower partial denture and have no difficulty in eating. She is being reviewed at 6-monthly interval.
Discussion
History
Gorham’s disease is a rare disorder characterized by progressive osteolysis and proliferation of vascular channels with replacement of fibrous connective tissue. It was categorized pathologically by Gorham and Stout more than five decades ago, however the precise aetiology of this massive osteolytic disease remains poorly understood. There is no predilection for age, race or sex, but the young adults are the most common group being affected and there is no evidence of a malignant, neuropathic, or infectious component involved in the causation of this disorder. Additionally, the mechanism of bone resorption is unclear.
The disease can affect any bone, either in a single or multiple contiguous bones in which commonly involved sites include the mandible (15%), ribs (12%), scapula (10%), humerus (8%), pelvis (10%), and femur (11%) [6,7]. Römer reported the first facial case of the disease in 1928 [5]. Since then, review showed that jaw is the most common site to be affected among the maxillofacial cases and the disease can be unicentric or multicentric [5,8,9].
Investigations
Biochemical and haematological tests are important to exclude other diagnoses. These tests were unremarkable as noted in our case as well as the other Gorham’s disease of maxillofacial cases [5,8-10]. Alkaline phosphatase may be elevated in a patient with an associated fracture [11]. Radiographic examination revealed massive bone resorption with widening of the periodontal ligament spaces of the affected teeth. The histopathology reports were usually inconclusive, designating a nonspecific inflammation [5,10]. The present case also showed the same non specific microscopic result until further immunohistochemical investigations were done.
Presentation
Gorham’s disease is usually monocentric where it starts in a particular bone and secondarily involve adjacent bones and soft tissue. However, Tsang and Zhang reported multicentric maxillofacial cases simultaneously affected frontal bone, zygoma, mandible and maxilla. The present case showed an initial involvement of the mandible and later the disease progressed to involve the maxilla as viewed in the radiograph during a 3-month post-operation review [12].
The disease had been described as having two-stage or fourstage phases depending on clinical and microscopic characteristics respectively. Klein described 2 phases of disease and the first phase involves pain and swelling with associated massive osteolysis while the second one is the quiescent phase. The duration of each phase may last for several weeks. While Moller described a four-stage phases : the first stage or the early intraosseous stage, is characterized by multiple ‘‘patchy’’ intramedullary and subcortical lucencies resembling osteoporosis. The second stage involves the coalescence of these lucencies and further development of new radiolucent areas at the periphery of the involved region. The third stage or the extraosseous stage, is characterized by cortical erosion and adjacent soft-tissue involvement. The fourth and final stage, the remaining bone is reabsorbed and finally replaced by fibrous tissue. The concentric shrinkage of the bone results in tapering of the involved end giving the appearance commonly described as ‘‘sucked candy’’. The present case showed a smooth tapering surface of bone resorption concentrating on the both premolars and first molar regions, consistent with the “sucked candy” appearance.
Aetiology
The cause of massive osteolysis in Gorham’s disease remains obscure, and no evidence of underlying metabolic or endocrine disorders has yet been found. However, there are many hypotheses of the aetiologies including post-traumatic hyperaemia, changes in blood pH, hypoxia, unrestricted growth of granulation tissue and endothelial cell-mediated absorption of bone matrix [13]. Gorham and Stout hypothesised that trauma may trigger this disease process by stimulating the production of vascular granulation tissue. As for the present case, there was no history of traumatic event experienced by the patient. While Devlin claimed the role of interleukin-6 (IL-6) as a potential humoral mediator where in Gorham’s disease, it is increased up to seven times the normal. IL-6 is produced by osteoclasts or as a response from muscular cells to IL-1 and tumor necrosis factor alpha (TNF) or from vessel dilatation which will then induce bone resorption through osteoclast cells stimulation [14]. In addition Heyden et al. proposed that the wide lumen of these vessels results in slowed blood flow leading to local hypoxia, lowering of pH and enhanced activation of various hydrolytic enzymes, thus facilitating bone resorption. The latest study has implicated that cells of monocyte-macrophage lineage may play an essential role in the pathogenesis of Gorham’s disease, with cytokine circuits accelerating angiogenesis and osteoclastogenesis [15].
Differential diagnoses
Differential diagnoses for Gorham’s disease include any possible causes of osteolysis for instance chronic infection, chronic inflammation, endocrine disease and local pathology of either cysts and tumors. However, to any inexperience practitioners, the clinical presentation of this disease may resembles localized periodontal disease, thus, it is crucial to have radiographic investigation.
Osteomyelitis is a common example of chronic infection. The clinical signs of this condition is compatible with this case, and include pain aggravated by movement (when patient closed her jaws together) and the presence of swelling. However, there is no history of a local or distant infectious process when patient was first diagnosed with Gorham’s disease and there was no associated suppuration.
Chronic inflammation process like juvenile rheumatoid arthritis is not as rapidly destructive as seen in this case, and is usually presented bilaterally [16].
Central giant cell lesion is compatible with younger age-group patients usually younger than 30 years where anterior of mandible is the commonest site. Similar to this case is the aggressive variants of the giant cell lesion which is characterized by pain, rapid growth and radiolucent bone defects. “Brown” tumors of hyperparathyroidism will then need to be ruled out by evaluating serum calcium, phosphorus, and parathyroid hormone levels. The simple bone cyst is consistent with this young age-group however acute pain is very uncommon but may also cause a large multilocular expansion. An aneurysmal bone cyst may occur in patients younger than 20 years, with the posterior mandible being a common site. Patients usually complaint of pain and rapidly develop swelling. In addition, radiographically aneurysmal bone cyst can gives either a unilocular or a multilocular appearance.
Primary tumors that show similar clinical appearance consistent with this scenario include fibrosarcoma, osteoscarcoma and chondrosarcoma that may present with swelling and pain, in addition to the radiographic findings and reports of a wide age range of involved patients. Mesenchymal chondrosarcoma is more likely to occurs in young patients between the age of 10 and 30 and clinically compatible with the findings in this case. Similarly, osteoblastoma is usually slow growing, but an aggressive subtype of osteoblastoma is larger and more destructive. Fibro-osseous lesions and Langerhans cell diseases should also be considered. Patients with fibro-osseous lesions exhibit bony enlargement of the affected site with facial asymmetry. The enlargement can be quite dramatic with apparent bony destruction. Furthermore, radiographically the lesion usually present with varying degrees of radiopacity and radiolucency. In Langerhans cell histiocytosis, presence of a solitary intraosseous lesion, multiple “scooped-out” and sclerotic bone lesions with a well-defined periphery, periosteal new bone formation and slight root resoption are the characteristics in addition to histology features. But in the present case, there where no new bone formation seen within or at the periphery, pale-staining Langerhans’ cells were not evident histologically and there was no root resoption seen in the radiograph [17-20].
Microscopic findings
There are numbers of reports indicate similar findings which is the presence of a benign vascular proliferation of thin-walled endothelial capillaries vascular spaces of various sizes [5,15,21,22]. These vessels have the potential to extend into the adjacent bone and soft tissues, resulting in replacement of bone by connective tissue containing many thin walled vessels. Over time, the vascular component of the lesion is almost completely replaced by fibrous connective tissue [23]. The destruction of the bone is contiguous and it is becoming thin and soft, with subsequent fracture [6,24,25]. Small capillaries with prominent endothelial cells, lymphoid infiltrates, and occasional eosinophils and plasma cells can also be found in focal areas as evident in the present case. As the lesion matures, abundant lipid-laden macrophages can be seen [16]. However, many of the older cases lack verifiable and consistent histopathology information making diagnosis of Gorham’s disease difficult [4]. Hefez listed criterias for diagnosing Gorham’s disease (Table 1) and many authors used these criterias as a guide to diagnose.
| Positive biopsy showing angiomatosis |
| Absence of tumour/cellular atypia |
| Little or no osteoblastic response |
| No dystrophic calcification |
| Local progressive resorption |
| Non-expansile, non-ulcerative lesion |
| Absence of visceral involvement |
| Osteolytic radiographic pattern |
| No hereditary, metabolic, immunologic or infectious cause |
Table 1: Clinical criteria for diagnosis for Gorham's disease.
Immunohistochemical stains for CD31, CD34 and Factor VIII confirmed a vascular origin of the lesion. CD31 and CD34 revealed vessels and lymphatic ducts while Factor VIII showed endothelial cells. Ki67 stain showed low cellular proliferative activity which signifies a nonmalignant proliferation. These immunostains were consistent with Ricalde and Escande findings. In addition, we also did other immunohistochemical investigations including CD20 and CD79a which confirmed B lymphocytes, CD3 showed T-lymphocytes, kappa and lambda light chains confirmed polyclonality of plasma cells and PGM1 showed presence of neutrophils and foamy histiocytes [26,27]. In view of the presence of many inflammatory cells (acute and chronic inflammatory cells), absence of malignant cells and evidence of blood and lymphatic vessel proliferation, the hypothesis of Gorham’s disease is considered.
Treatment
In most cases, surgery and/or radiation therapy have been used for treatment and the surgery may provides the best chance for cure [25,28]. Treatment using bone grafting in an effort to avoid amputation can be complicated by frequent absorption of the graft [28]. Radiation therapy is reported effective to produce arrest of osteolysis where it can reduce capillary proliferation and occasional recalcification. Some author suggested the use of radiation therapy as soon as the diagnosis is established and the area irradiated should include the surrounding soft tissues that show clinical or imaging evidence of disease [29]. Nevertheless, the response is unpredictable and in the case of Gorham’s disease, it’s use is still controversial in literature [11,29]. Use of various analgesics, chemotherapy, biphosphonate, calcium, fluoride, vitamin D, hormones, amino acids, adrenal extracts, UV radiation, somatotrophin, and transfusions of placental blood or blood from growing young children resulted in limited success [11,23,30,31]. Spontaneous recovery has also been reported [32]. As in our case, the mandibular bone is stabilized after the surgical intervention without any exploit of medications except calcium and vitamin D.
Conclusion
This case illustrates the difficulty in order to achieve a definitive diagnosis of this rare, little known disease where the initial histopathology biopsy reports confirmed non-specified inflammatory process. However, later investigations using immunohistochemistry showed proliferation of vascular channels thus permit elimination of a diagnosis of tumour, cyst, granulomatouslesion or other chronic infection or inflammation. Additionally, clinical biochemistry andhematology results proved to be normal thus exclude other clinical diagnoses. A list of criterias for diagnosing Gorham’s disease by Hefez is very helpful. Treatment is controversial and responses may vary among patients but sometimes it is better to be on the safe side as the disease has a tendency to spontaneously healed.
References
- Jackson JBS (1838) A boneless arm. Boston Med Surg J 10:368.
- Gorham LW, Wright AW, Shultz HH, MaxonFC Jr (1954) Disappearing bones: a rare form of massive osteolysis; report of two cases, one with autopsy findings.Am J Med 17: 674-682.
- Gorham LW, Stout AP (1955) Massive osteolysis (acute spontaneous absorption of bone, phantom bone, disappearing bone); its relation to hemangiomatosis.J Bone Joint Surg Am 37-37A: 985-1004.
- Holroyd I, Dillon M, Roberts GJ (2000) Gorham's disease: a case (including dental presentation) of vanishing bone disease.Oral Surg Oral Med Oral Pathol Oral RadiolEndod 89: 125-129.
- Escande C, Schouman T, Françoise G, Haroche J, Ménard P, et al. (2008) Histological features and management of a mandibular Gorham disease: a case report and review of maxillofacial cases in the literature.Oral Surg Oral Med Oral Pathol Oral RadiolEndod 106: e30-37.
- Choma ND, Biscotti CV, Bauer TW, Mehta AC, Licata AA (1987) Gorham's syndrome: a case report and review of the literature.Am J Med 83: 1151-1156.
- Duffy BM, Manon R, Patel RR, Welsh JS (2005) A case of Gorham's disease with chylothorax treated curatively with radiation therapy.Clin Med Res 3: 83-86.
- Tsang WM, Tong AC, Chow LT, Ng IO (2004) Massive osteolysis (Gorham disease) of the maxillofacial skeleton: report of 2 cases.J Oral Maxillofac Surg 62: 225-230.
- Zhong LP, Zheng JW, Zhang WL, Zhang SY, Zhu HG, et al. (2008) Multicentric Gorham's disease in the oral and maxillofacial region: report of a case and review of the literature.J Oral Maxillofac Surg 66: 1073-1076.
- Motamedi MH, Homauni SM, Behnia H (2003) Massive osteolysis of the mandible: a case report.J Oral Maxillofac Surg 61: 957-963.
- Möller G, Priemel M, Amling M, Werner M, Kuhlmey AS, et al. (1999) The Gorham-Stout syndrome (Gorham's massive osteolysis). A report of six cases with histopathological findings.J Bone Joint Surg Br 81: 501-506.
- Klein M, Metelmann HR, Gross U (1996) Massive osteolysis (Gorham-Stout syndrome) in the maxillofacial region: an unusual manifestation.Int J Oral Maxillofac Surg 25: 376-378.
- Chung C, Yu JS, Resnick D, Vaughan LM, Haghighi P (1997) Gorham syndrome of the thorax and cervical spine: CT and MRI findings.Skeletal Radiol 26: 55-59.
- Heyden G, Kindblom LG, Nielsen JM (1977) Disappearing bone disease. A clinical and histological study.J Bone Joint Surg Am 59: 57-61.
- Colucci S, Taraboletti G, Primo L, Viale A, Roca C, et al. (2006) Gorham-Stout syndrome: a monocyte-mediated cytokine propelled disease.J Bone Miner Res 21: 207-218.
- Möller G, Priemel M, Amling M, Werner M, Kuhlmey AS, et al. (1999) The Gorham-Stout syndrome (Gorham's massive osteolysis). A report of six cases with histopathological findings.J Bone Joint Surg Br 81: 501-506.
- Moenning JE, Williams KL, McBride JS, Rafetto LK (1998) Resorption of the mandibular condyle in a 6-year-old child.J Oral Maxillofac Surg 56: 477-482.
- Neville BW, Damm DD, Allen CM and Bouquot JE (2002) Soft tissue tumours. In: Oral and Maxillofacial Pathology (2ndedn) Saunders.
- Neville BW, Damm DD, Allen CM,Bouquot JE (2002) Bone pathology. In:. Oral and Maxillofacial Pathology (2ndedn) Saunders
- Greenberg MS, Glick M and Jonathan AS (2008) Infectious disease. In:Burkets Oral Medicine, (11thedn).
- Shives TC, Beabout JW, Unni KK (1993) Massive osteolysis.Clin Orthop Relat Res: 267-276.
- Devlin RD, Bone HG 3rd, Roodman GD (1996) Interleukin-6: a potential mediator of the massive osteolysis in patients with Gorham-Stout disease.J Clin Endocrinol Metab 81: 1893-1897.
- Mendez AA, Keret D, Robertson W, MacEwen GD (1989) Massive osteolysis of the femur (Gorham's disease): a case report and review of the literature.J Pediatr Orthop 9: 604-608.
- Drewry GR, Sutterlin CE 3rd, Martinez CR, Brantley SG (1994) Gorham disease of the spine.Spine (Phila Pa 1976) 19: 2213-2222.
- Yoo SY, Hong SH, Chung HW, Choi JA, Kim CJ, et al. (2002) MRI of Gorham's disease: findings in two cases.Skeletal Radiol 31: 301-306.
- Heffez L, Doku HC, Carter BL, Feeney JE (1983) Perspectives on massive osteolysis. Report of a case and review of the literature.Oral Surg Oral Med Oral Pathol 55: 331-343.
- Ricalde P, Ord RA, Sun CC (2003) Vanishing bone disease in a five year old: report of a case and review of the literature.Int J Oral Maxillofac Surg 32: 222-226.
- Dunbar SF, Rosenberg A, Mankin H, Rosenthal D, Suit HD (1993) Gorham's massive osteolysis: the role of radiation therapy and a review of the literature.Int J Radiat Oncol Biol Phys 26: 491-497.
- Vinée P, Tanyü MO, Hauenstein KH, Sigmund G, Stöver B, et al. (1994) CT and MRI of Gorham syndrome.J Comput Assist Tomogr 18: 985-989.
- Fisher KL, Pogrel MA (1990) Gorham's syndrome (massive osteolysis): a case report.J Oral Maxillofac Surg 48: 1222-1225.
- Auge B, Toussirot E, Kantelip B, Wendling D (1998) From polycystic bone angiomatosis to Gorham's disease. Two case-reports and literature review.Rev Rhum Engl Ed 65: 201-206.
- Spieth ME, Greenspan A, Forrester DM, Ansari AN, Kimura RL, et al. (1997) Gorham's disease of the radius: radiographic, scintigraphic, and MRI findings with pathologic correlation. A case report and review of the literature.Skeletal Radiol 26: 659-663.
Relevant Topics
- Blepharoplasty
- Bone Anchored Hearing Aids
- Chemical peel
- Cleft Surgery
- Congenital Craniofacial Malformations
- Cosmetic Facial Surgery
- Craniofacial Surgery
- Dental Orofacial Surgery
- Dentoalveolar Surgery
- Head and Neck Reconstruction
- Injectable Cosmetic Treatments
- Lip Reconstruction
- Mandibular Nerve Surgery
- Maxfax Surgery
- Maxillofacial Surgery
- Neck Liposuction
- Oral and Maxillofacial Surgery
- Oral Surgery Surgeon
- Orofacial Surgery Braces
- Pediatric Maxillofacial Surgery
- Rhytidectomy
- Sleep Apnea Orofacial Surgery
- Temporomandibular Joint Disorders
- Upper Jaw Surgery
Recommended Journals
Article Tools
Article Usage
- Total views: 12482
- [From(publication date):
December-2015 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 11603
- PDF downloads : 879