Case Report Open Access
Giant Gastrointestinal Stromal Tumor with Double Bowel Obstruction: Diagnostic and Therapeutic Challenges-Case Report
Freddy Houehanou Rodrigue Gnangnon1*, Souaibou Yacoubou Imorou1, Dansou Gaspard Gbessi1, Anicet Meli1, Romulus Takin2, Ismail Lawani1, Raimi Kpossou3, Francis Moïse Dossou1 and Jean Leon Olory-Togbe11Department of Surgery, Faculty of Medicine, University of Abomey-Calavi, Benin
2Department of Pathology, Troyes General Hospital, Troyes, France
3Department of Gastroenterology and Hepatology, University of Abomey-Calavi, Benin
- *Corresponding Author:
- Gnangnon FHR
Assistant Professor of Surgical Oncology
Department of Surgery, Faculty of Medicine
University of Abomey-Calavi, Benin
Tel: 0022967648699
E-mail: fredgnang@yahoo.fr
Received Date: February 20, 2017; Accepted Date: February 28, 2017; Published Date: March 07, 2017
Citation: Gnangnon FHR, Yacoubou IS, Gaspard GD, Anicet M, Romulus T, et al. (2017) Giant Gastrointestinal Stromal Tumor with Double Bowel Obstruction: Diagnostic and Therapeutic Challenges-Case Report. Cancer Surg 2: 112.
Copyright: © 2017 Gnangnon FHR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.
Visit for more related articles at Cancer Surgery
Abstract
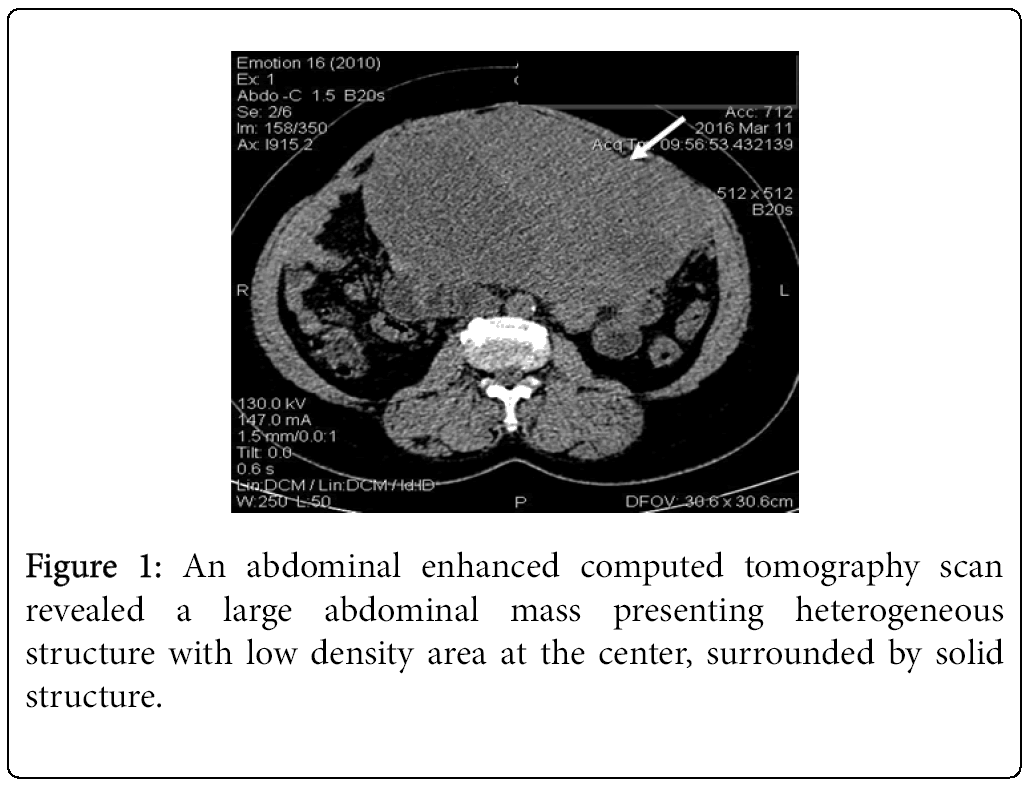
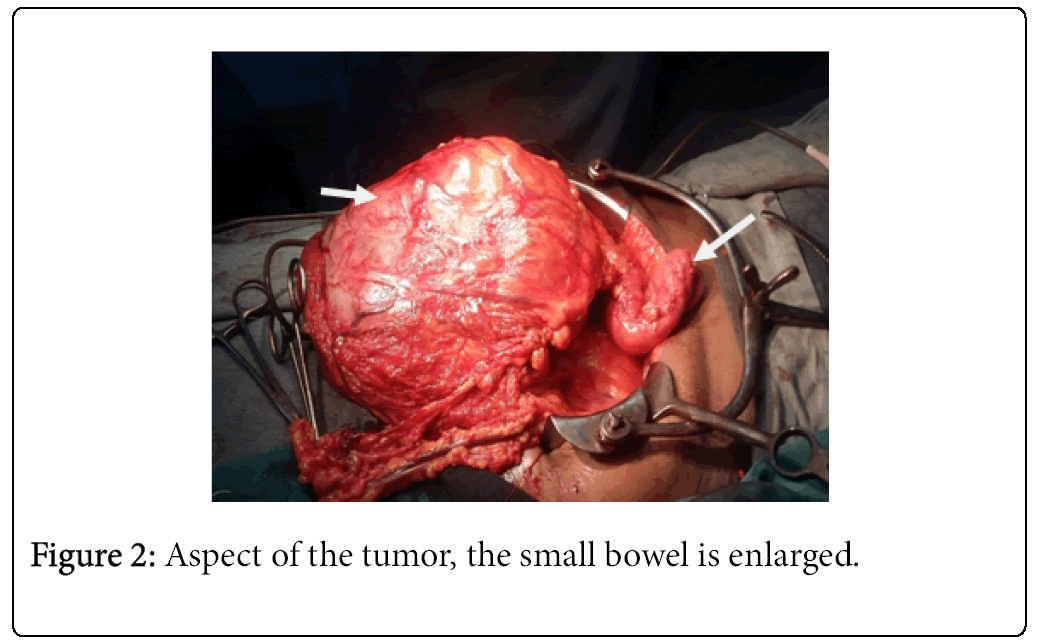
Background: Gastrointestinal stromal tumors are the most common mesenchymal tumors of the digestive tract with expression of phenotype KIT/CD117 and CD34+. The stomach and small intestine are the favored sites of occurrence. The most common complication is a gastrointestinal bleeding, bowel obstruction being rare and often associated with very large tumors. Case report: We describe a 62-years-old woman presented with symptoms of abdominal pain, increased volume of the abdomen. Clinical examination revealed mild abdominal distension and a large epigastric mass. Abdominal CT scan revealed a large abdominal mass presenting mixed structure. Intraoperative findings showed a large cystic mass with solid area of 30/20 cm invading the jejunum and the transverse colon. We performed an en-block resection of the mass with a segmental resection of the transverse colon and jejunum followed by manual end-toend anastomosis. Histo-pathological examination revealed a large gastrointestinal stromal tumor invading the jejunum and the colon. Conclusion: Jejunal and colonic gastrointestinal stromal tumors are not common and can present as bowel obstruction. The surgical management of a giant GIST can be a particularly complex challenge. It is imperative to avoid rupture of the tumor capsule as it is associated to poor outcomes. Tumor size is one of the main prognosis factors.
Keywords
Giant tumor; Colon; Jejunum; GIST; Bowel obstruction
Introduction
Gastrointestinal stromal tumours (GISTs) are the most common mesenchymal tumours of the digestive tract arising from interstitial cells of Cajal (ICC). GISTs are characterized by expression of phenotype KIT/CD117 (95%) and CD34+ (70%) [1]. Although they represent 85% of all mesenchymal neoplasms that affect the gastrointestinal tract, GISTs are rare mesenchymal tumours of the digestive tract (less than 1 to 3% of the digestive tract neoplasia) [2,3]. The most frequent locations are stomach and small intestine followed by colon, rectum and oesophagus. Usually, the size ranges from small tumours less than 1 cm, typically incidentally discovered [2], up to large tumours of 35 cm. They have various and non-specific symptomatology [3]. The most common symptoms are abdominal pain, epigastric mass and GI bleeding. Bowel obstruction is a rare complication and is often associated with very large tumour. The main prognostic factors are tumour size, mitotic index and metastasis. Surgical resection is the main treatment for focal disease.
We present an unusual case of giant GIST of jejunum and colon that presented as bowel obstruction, significant due to per-operative surgical challenge.
Case Presentation
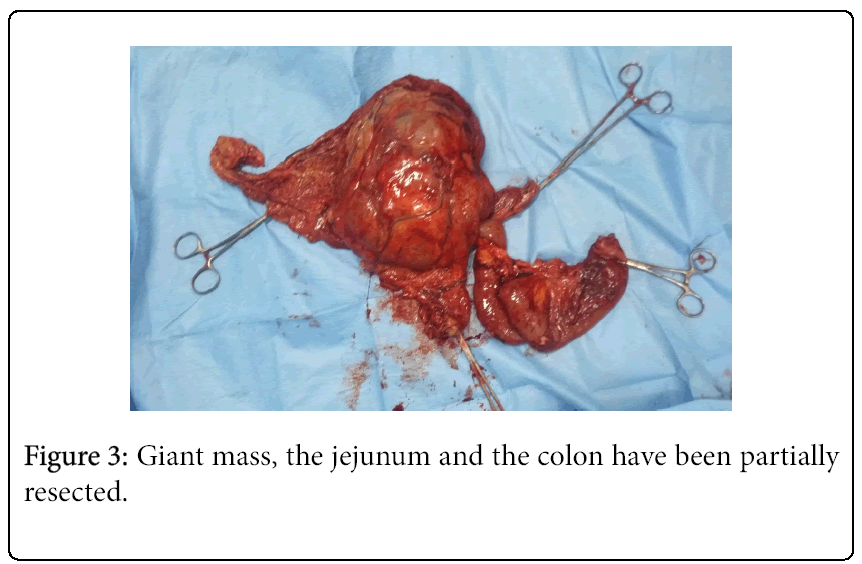
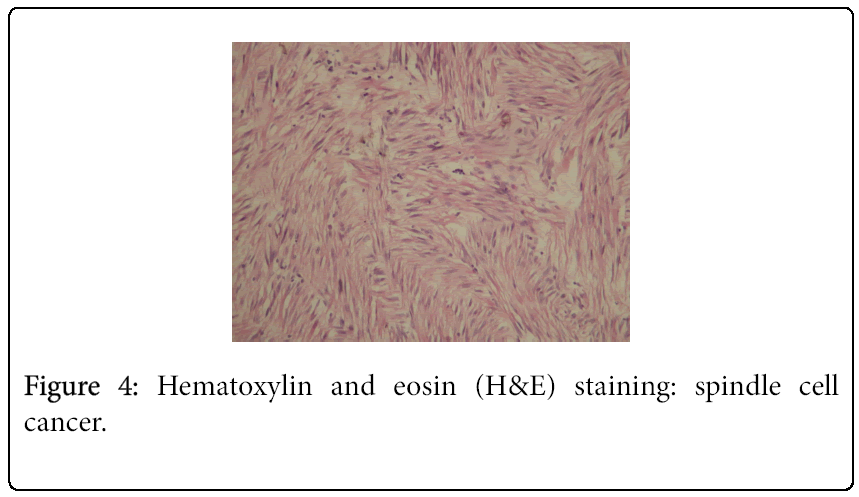
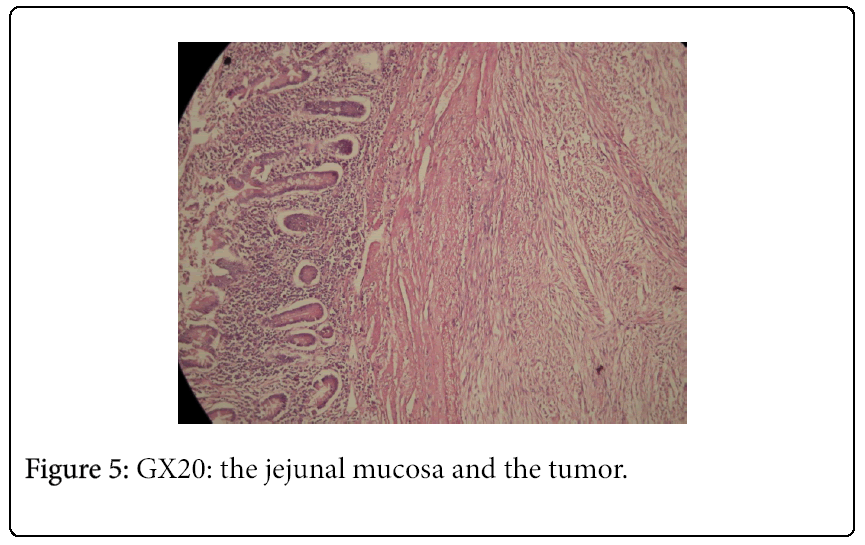
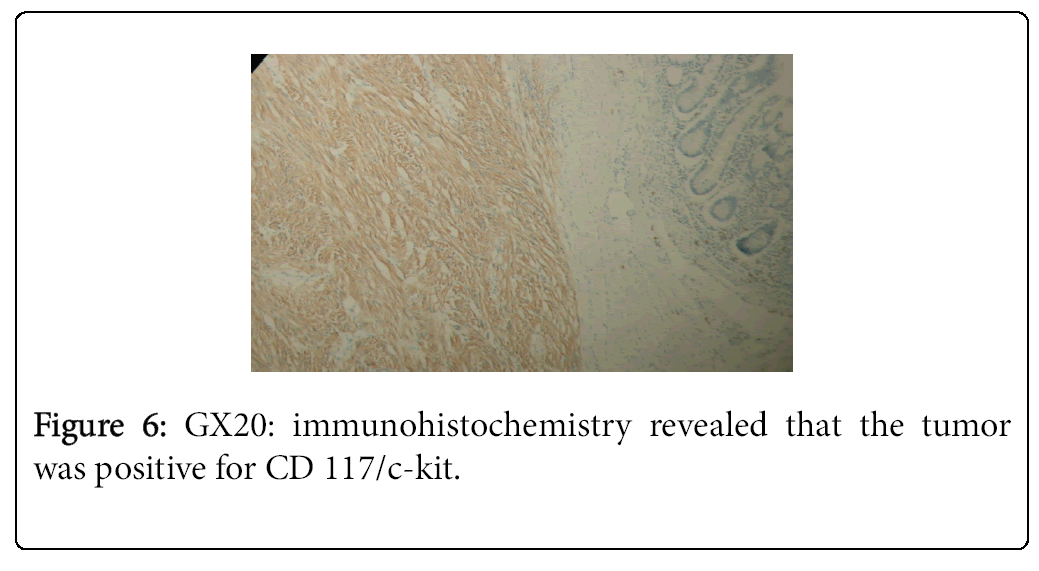
A 62-year-old black woman with medical history of high blood pressure and diabetes mellitus, presented with symptoms of abdominal pain, increased volume of abdomen, nausea, vomiting and constipation. The general condition was poor, with weight lost. There was no episode of gastrointestinal bleeding. The symptoms appeared two years ago, worsening progressively. The patient was hemodynamically stable. Clinical examination revealed abdominal distension and a large epigastric mass. Blood count revealed an anemia (9.3 g/dl) and thrombocytosis (456 G/L). A previous abdominal CT scan, performed one month before admission, had revealed a large abdominal mass, measuring 20.5 × 18 × 11.5 cm (Figure 1). The mass presented mixed structure with low density area at the centre, surrounded by solid structure. Workup for distant metastasis was negative. The surgery was performed via a midline incision after a quick resuscitation. Intraoperative findings showed a large cystic mass with solid area of 30/20 cm arising from the mesentery, intimately adherent to the jejunum and the transverse colon (Figures 2 and 3). The small intestine and the right colon were distended. There was no liver and peritoneal metastasis. We performed an “en-block resection” of the mass with a segmental resection of the transverse colon and jejunum followed by end-to-end anastomosis and mesenteric lymph nodes biopsy. Resection margin was of 5 cm on the colon and 10 cm on the jejunum. The tumour was not ruptured. Histopathological examination revealed a large tumour invading the jejunum and the colon (Figure 4). It was not possible to determine the primary site. The tumour has heterogeneous consistency, with alternating solid structure and multiple areas of necrosis. Immunohistochemical staining showed positive results for KIT (CD 117) and CD 34 (Figures 5 and 6). Mitotic rate was 5/50 HPF (high-power field), recurrence risk was 52% based on Miettienen classification [4]. Resected lymph nodes did not show any metastatic spread. Resected jejunum and colon showed clear margins. The postoperative course was uneventful and the patient was discharged 10 days after the surgery. She received an adjuvant therapy: imatinib mesylate, 400 mg daily for 6 months. Currently, eight months after the beginning of the treatment, she is alive with no sign of reoccurrence.
Discussion
Gastrointestinal stromal tumours (GISTs) are rare but challenging tumours especially due to the diagnosis and therapy [3]. The surgical management of a giant GIST is a complex issue [2]. GIST tumour biology allows the development to giant sizes without altering the general condition, which is a clinical characteristic of these tumours [3]. Our patient’s general condition was impaired due to the late diagnosis and the bowel obstruction.
GISTs are found most commonly in the stomach (60-70%) and small intestine (20-30%), whereas colon, rectum and oesophagus are rarely affected (5-10%). In our case, it was difficult for the pathologist to determine clearly the primary site as the tumour invaded both the jejunum and the colon.
GISTs of the colon frequently occur in the left or transverse colon [1,4,5]. About 20% of GISTs do originate from the jejunum or ileum. GISTs usually occur as isolated lesions in stomach, small intestine or colon. However, association of small bowel GIST with synchronous colonic GIST is exceptional.
The size of these tumours varies greatly. Small GISTs (less than 1 to 2 cm) are clinically silent and are often diagnosed incidentally during endoscopy. They usually behave like benign tumors whereas large tumours often behave like malignant tumours and present with nonspecific symptomatology like epigastric mass, gastrointestinal bleeding (GI bleeding) or bowel obstruction [4]. The most common acute presentation requiring surgical management is GI bleeding; bowel obstruction is being much less common. Bowel obstruction may result from intraluminal growth of the tumour or luminal compression from an exophytic lesion [6-8]. In our case, we think that the symptoms are related to intraluminal compression although the epithelium was free of tumour.
The diagnosis of the GISTs is largely histopathological. That diagnosis can be particularly difficult in low income countries like Benin. In our case we had to send the specimen to France for immunohistochemistry.
Size, mitotic index, and metastasis are the main prognosis factors. New classification based on tumour location, size, and mitotic rate has been used to evaluate the risk of recurrence and metastasis. Jejunum GIST more than 2 cm with mitotic index of 5/50 HPF are considered as high risk tumours [1]. In our case the tumour was 30 × 15 ×11 cm in size with mitotic rate of 5/50 HPF and recurrence risk was 52% based on Miettienen classification.
Surgical resection with clear margin is the main treatment for focal tumors and is sometimes technically challenging with patient on occlusion [7,9]. Lymph nodes resection has been performed in our case as enlarged lymph node was seen in the mesentery but routine lymph node resection is not recommended since they are rarely invaded [6]. In our case, all the lymph nodes were free of tumor. There was no intraoperative tumor rupture in our case. The surgeon has to avoid tumor rupture to reduce risk of peritoneal recurrence [9]. In our case, the tumor was not rupted.
Targeted therapy with imatinib, a tyrosine kinase inhibitor has provided excellent results for many patients with both resectable and unresectable GISTs [10,11]. Development of targeted therapies has contributed to the stabilization of cancer mortality in many countries. Worldwide, however, one of the main factors that limit patient access to these important new drugs is their cost, which is higher than traditional chemotherapy [12]. Benin is a low income country and access to such drugs is a particular challenge for all patients.
Conclusion
We presented in this article the issue of diagnosis and treatment of a giant GIST invading both the jejunum and the colon. The surgical management of such large tumors invading many organs can be a complex challenge. Resection with clear margins is the best treatment when possible. It is imperative to avoid rupture of the tumor capsule as it is associated to poor outcomes. Tumor size is one of the main prognosis factors. Adjuvant therapy involving selective receptor tyrosine kinase inhibitors should be considered in high-risk GIST patients.
The diagnosis is particularly difficult in low income countries due to the lack of immunohistochemistry. That fact may explain the limited number of articles in sub-Saharan Africa on the subject. In those countries, access to targeted therapies is problematic.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal.
Competing Interests
The authors declare that they have no competing interests.
References
- Graadt van Roggen JF, van Veithuysen MLF, Hogendoorn PCW (2001) The histopathological differential diagnosis of gastrointestinal tumors. J Clin Pathol 54: 96-102.
- Cappellani A, Piccolo G, Cardì F, Cavallaro A, Lo Menzo E, et al. (2013) Giant gastrointestinal stromal tumor (GIST) of the stomach cause of high bowel obstruction: surgical management. World J Surg Oncol 11: 172.
- Constantinoiu S, Gheorghe M, Popa L, Ciocea C, Iosif C, et al. (2015) Giant Esophageal GIST: Diagnostic and therapeutic challenge-Case report. Chirurgia 110: 300-307.
- Miettinen M, Lasota J (2006) Gastrointestinal stromal tumors: Pathology and prognosis at different sites. Semin Diagn Pathol 23: 70-83.
- Iwamoto R, Kataoka TR, Furuhata A, Ono K, Hirota S, et al. (2016) Perivascular epithelioid cell tumor of the descending colon mimicking a gastrointestinal stromal tumor: A case report. World J Surg Oncol 14: 285.
- Burkill GJC, Badran M, Thomas JM, Judson IR, Fisher C, et al. (2003) Malignant gastrointestinal stromal tumour: Distribution, imaging features, and pattern of metastatic spread. Radiology 226: 527-532.
- Sezer A, Yagci M, Hatipoglu A (2009) A rare cause of intestinal obstruction due to an exophytic gastrointestinal stromal tumor of the small bowel. Signa Vitae 4: 32-34.
- Fischer C, Nagel H, Metzger J (2009) Image of the month. Gastrointestinal stromal tumor of the small bowel. Arch Surg 144: 379-380.
- Rammohan A, Sathyanesan J, Rajendran K, Pitchaimuthu A, Perumal SK, et al. (2013) A gist of gastrointestinal stromal tumors: A review. World J Gastrointest Oncol 5: 102-112.
- Van Oosterom AT, Judson I, Verweij J, Stroobants S, Donato di Paola E, et al. (2001) Safety and efficacy of imatinib (STI 571) in metastatic gastrointestinal stromal tumours: A phase I study. Lancet 358: 1421-1423.
- DeMatteo RP, Ballman KV, Antonescu CR, Maki RG, Pisters PW, et al. (2009) Adjuvant imatinib mesylate after resection of localised, primary gastrointestinal stromal tumor: a randomised, double-blind, placebo-controlled trial. Lancet 373: 1097-1104.
- Dranitsaris G, Truter I, Lubbe MS, Amir E, Evans W, et al. (2011) Advances in cancer therapeutics and patient access to new drugs. Pharmacoeconomics 29: 213-224.
Relevant Topics
- Breast Cancer Surgery
- Colon Cancer Surgery
- Dermatologic Surgery
- Kidney Cancer Surgery
- Leukemia Surgery
- Lung Cancer Surgery
- Lymphoma Surgery
- Oesophageal Cancer Surgery
- Pancreatic Cancer Surgery
- Prostate Cancer Surgery
- Radiation Therapy
- Skin Cancer Surgery
- Stomach Cancer Surgery
- Throat Cancer Surgery
- Thyroid Cancer Surgery
Recommended Journals
Article Tools
Article Usage
- Total views: 4512
- [From(publication date):
March-2017 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 3627
- PDF downloads : 885