Case Report Open Access
Giant Dedifferentiated Liposarcoma of the Retroperitoneum
In-Hwan Kim and Hyun-Dong Chae*
Department of Surgery, School of Medicine, Daegu Catholic University Hospital, Daegu, Korea
- *Corresponding Author:
- Hyun-Dong Chae
Department of Surgery, School of Medicine
Daegu Catholic University Hospital, 3056-6
Daemyung-4-Dong, Namgu, 705-718, Daegu, Korea
Tel: 82536504429
Fax: 82536247185
E-mail: hdchae@cu.ac.kr
Received date: January 13, 2017; Accepted date: February 15, 2017; Published date: February 23, 2017
Citation: Kim I, Chae H (2017) Giant Dedifferentiated Liposarcoma of the Retroperitoneum. J Gastrointest Dig Syst 7:487. doi: 10.4172/2161-069X.1000487
Copyright: © 2017 Kim I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
A retroperitoneal liposarcoma is a rare tumor. It is classified as several subtypes according to the quantity of lipid, mucoid lipid, and the differentiation of cells. When a tumor is histologically composed of well to poorly differentiated liposarcoma and non-lipomatous sarcoma, it is called a dedifferentiated liposarcoma. Although the prognosis of most liposarcomas are better than other sarcomas, dedifferentiated liposarcoma could be life-threatening because of its higher malignant potential. A dedifferentiated retroperitoneal liposarcoma is a rare disease and there are only a few studies reported, especially in Korea and Asian countries. Despite the relative rarity, these tumors can cause significant morbidity and mortality in affected patients, and complete resection is only the principal treatment. Therefore, we report a case of a giant dedifferentiated liposarcoma of the retroperitoneum in a 66-year-old man who underwent complete resection.
Keywords
Retroperitoneum; Liposarcoma; Dedifferentiation
Introduction
Liposarcoma is a malignant tumor of mesenchymal origin. The most common sites of liposarcomas are the extremities, followed by retroperitoneum, and inguinal area [1]. Retroperitoneal liposarcoma is a rare tumor, with an incidence of 2.5 per million, accounting for 10-15% of soft tissue tumors. Because of rarity, biological behavior of this tumor is not well-known [2]. However, among retroperitoneal tumors, liposarcoma is the most common tumor reported as 26-57%, followed by leiomyosarcoma, malignant fibrous histiocytoma, malignant peripheral nerve sheath tumor, and others [3].
Retroperitoneal liposarcomas grow slowly and silently and may not become symptomatic until they are very large, so diagnosis is often delayed. Only complete excision provides hope for a cure, but this is often difficult because the margins are not grossly apparent, so a contiguous organ may have to be resected. Resection of adjacent structures is required in 57-77% of cases to achieve complete tumor resection [3].
These tumors are classified into subtypes according to their pathological features including the amount of intracellular lipid, the quantity of mucoid lipid, and the differentiation of cells [1]. The most common type is well differentiated liposarcoma. Dedifferentiated type of liposarcoma is relatively rare, which is defined by histological coexistence of well and poorly differentiation. Although well differentiated and dedifferentiated subtypes share common morphological features, dedifferentiated liposarcoma has much higher malignant potential with poor prognosis [2].
We report a case of a giant dedifferentiated liposarcoma of the retroperitoneum, to emphasize the importance of complete surgical resection and necessity of close follow up for the dedifferentiated liposarcoma.
Case Report
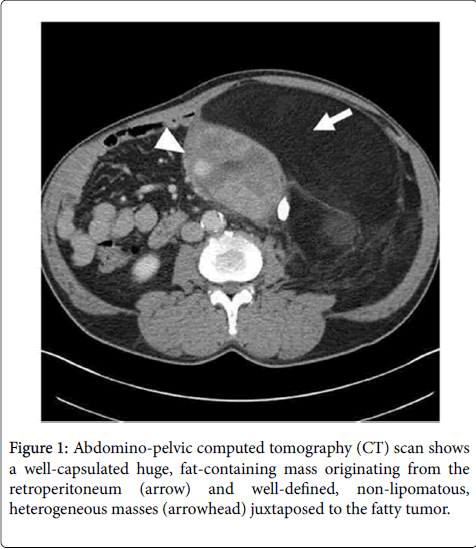
A 66-year-old man was admitted with complaints of vague abdominal pain on left side that had persisted for 1 year, an abdominal palpable mass with increasing size for several months, and postprandial satiety for 2 years. The patient had noticed a rapid progression of increased abdominal girth. There was no history of trauma, drug, or alcohol abuse. A physical examination revealed a large mass like lesion in the left upper abdominal quadrant, but no tenderness, guarding or rigidity were noted. There was no specific problem in laboratory markers. An abdominal X-ray examination showed deviation of intestinal gas shadow to the right side of abdomen, which was a finding, suggested a huge mass on left side. An abdomino-pelvic computed tomography (CT) scan showed a mass with 40 cm in largest dimension composed of a 25 × 16 cm sized hypodense and a 15 × 12 cm sized hyper-dense lesion in the retroperitoneal area of left upper abdominal quadrant, but no adjacent organ was involved (Figure 1). An ultrasono-guided needle biopsy was performed for the diagnosis of this tumor, and the pathologic result showed suggestive of sarcoma.
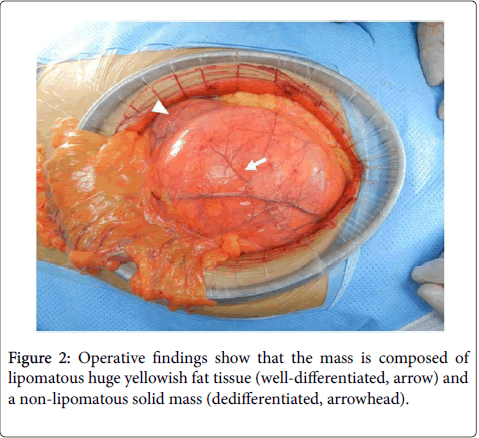
Based on the radiologic and pathologic findings, surgery was decided because of the compression symptoms and the possibility of malignancy. Peritoneal cavity was explored through median abdominal incision, and retroperitoneum was dissected to identify the retroperitoneal tumor. The tumor was composed of a large amount of lipomatous yellowish fat tissue and a non-lipomatous solid mass with well circumscribed, encapsulated, and distinct lobulated pattern that was almost uniformly yellow (Figure 2). The mass was carried out successfully with en bloc resection with a complete gross R0 resection, because there was no invasion to adjacent organ with little adhesion to surrounding tissues. After confirmation of no other organ injury or abnormality, peritoneal irrigation was done and abdominal wall was closed.
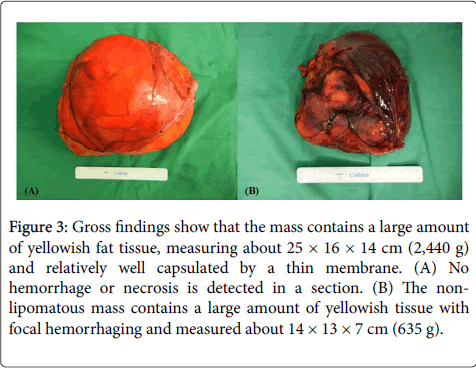
The huge mass had a clearly distinguishable outer membrane, a smooth, polished surface, and composed of 25 × 16 × 14 cm (2,440 g) and 14 × 13 × 7 cm (635 g) masses with histologically negative resection margin (Figure 3). The histopathological findings revealed that the tumor was composed of a well-differentiated lesion, which included mature adipocytes and a few scattered lipoblasts, and a dedifferentiated lesion, which consisted of spindle cells with highgrade atypia.
Figure 3: Gross findings show that the mass contains a large amount of yellowish fat tissue, measuring about 25 × 16 × 14 cm (2,440 g) and relatively well capsulated by a thin membrane. (A) No hemorrhage or necrosis is detected in a section. (B) The nonlipomatous mass contains a large amount of yellowish tissue with focal hemorrhaging and measured about 14 × 13 × 7 cm (635 g).
The patient recovered uneventfully and was discharged on postoperative day 9. No evidence of recurrence or metastasis was noted on a follow-up CT scan at the 2-year follow-up examination which had been taken every 3 months.
Discussion
Liposarcoma is the most common soft tissue sarcoma, accounting for 10-20% of all cases. It commonly occurs between 40-60 years of age and has a 1:1 ratio between genders [4]. Retroperitoneal liposarcoma is rare disease, but it is the most common subtype of retroperitoneal tumors. Mendenhall et al. [4] reported that 26-57% of retroperitoneal tumor was liposarcoma, followed by leiomyosarcoma (17-29%), malignant fibrous histiocytoma (7-17%), malignant peripheral nerve sheath tumor (8%), rhabdomyosarcoma (7%), synovial sarcoma (2%), and Ewing sarcoma (2%).
Retroperitoneal liposarcomas grow slowly and no symptoms occur in their initial periods and may not become symptomatic until they are very large, so they usually reach quite large size as 30 cm in largest dimension at diagnosis [2]. Complete resection of retroperitoneal liposarcoma remains the principal treatment, regardless of tumor size. When the tumor is well encapsulated by soft tissue, complete surgical resection can be achieved without resection of adjacent organ. However, resecting contiguous organs is necessary for an R0 resection in many cases and includes en bloc resection of other retroperitoneal organs, including the kidney, adrenal gland, pancreas, spleen, and even a vascular resection (inferior vena cava) if indicated [3]. One report stated that combined resection of adjacent organs is required in 75% of retroperitoneal tumors [5]. Partial or subtotal resection is generally not recommended in the case that complete resection is impossible, but partial resection can be performed for relief of symptom such as intestinal obstruction or vascular compression [3]. Radiation therapy or additional chemotherapy is controversial.
Liposarcomas can be classified into five types, based on morphological features and cytogenetic aberrations [6]. The most common forms of liposarcoma are well differentiated (46%), followed by dedifferentiated (18%), myxoid (18%), round cell (10%), and pleomorphic (8%). Well and dedifferentiated types occur more commonly in retroperitoneum compared with Myxoid and cellular cell type, which are predominant at extremities [3].
Dedifferentiated liposarcoma is histological coexistence of well to poorly differentiated liposarcoma and non-lipomatous differentiated areas [7], and is thought to be a malignant change from a welldifferentiated liposarcoma. Dedifferentiated liposarcomas are characterized by a supernumerary ring or giant chromosomes derived from the 12q region, which is a finding identical to that displayed by well-differentiated liposarcomas [8].
The sarcoma subtypes are closely related to the prognosis, so a histological examination is important. Although well differentiated and dedifferentiated subtypes share common morphological features and genetic events, their biologic behaviors are quite different. A dedifferentiated tumor tends to present more often as a recurrence, requires multi-organ resection more frequently, and has a shorter disease-free interval compared to those of well differentiated subtypes. Lahat et al. [9] reported that 5-year relapse free survival of dedifferentiated liposarcoma was 7.8% compared to well differentiated type (41.9%), and overall survival rate of dedifferentiated and well differentiated type was 36.5% versus 92.1%. Therefore, in the cases of dedifferentiated liposarcoma, close follow up and careful surveillance are warranted for the detection of recurrence.
Factors associated with a poor survival prognosis include the dedifferentiated subtype, grade 2-3, stage II-III, size >20 cm, and involved surgical margins. Distant metastasis is more common with de-differentiated, grade II-III, and the deep seated (retroperitoneal) tumor location. Zhang et al. [10] proposed that a CT scan should be taken every 3 months for the first 2 years, every 6 months for 2-5 years and annually thereafter to detect recurrence. In the current case, despite of large size of the tumor reaching 40 cm in largest dimension, complete resection was performed with clear resection margins. No recurrence has been observed for 2 years after the surgery, and the patient is undergoing regular follow-up check-ups.
Local recurrence following complete resection of primary retroperitoneal liposarcoma is common with 50% of well-differentiated and 80% of dedifferentiated tumors recurring within 5 years, and most patients who die of retroperitoneal soft tissue sarcoma die from the effects of local recurrence [11]. There is limited data to guide the management of locally recurrent retroperitoneal liposarcoma following complete resection of the primary [11]. The efficacy of chemotherapy has not been demonstrated in any hitherto published study. In fact, significant side effects and high morbidity rates have been detected. Therefore, one could conclude that chemotherapy presents very limited importance regarding the treatment of liposarcomas [12]. Although response to irradiation may be variable and unpredictable, the primary limitation of radiotherapy lies in its toxic effects on the adjacent intra-abdominal and retroperitoneal organs, and recurrent liposarcomas are less radiosensitive than primary tumors. Chemotherapy and radiation therapy have shown little efficacy in the treatment of locally recurrent tumor, and the treatment of choice is still to remove the recurrence [12].
In summary, retroperitoneal liposarcoma is an uncommon tumor which usually reaches large size when diagnosed. Complete surgical resection is important for treatment, and adjacent organ resection is often necessary. Histologic subtype of liposarcoma is important for the prognosis. Because dedifferentiated liposarcomas have high malignant potential with risk of recurrence and distant metastasis, careful surveillance is warranted.
Conflicts of Interest
We have no conflicts of interest to disclose and received no funding from the manufacturer of any drug, treatment, or device for conducting this study.
References
- Antinori A, Antonacci V, Magistrelli P (2002) Giant retroperitoneal liposarcoma. Am J Surg184:56-57.
- Neuhaus SJ, Barry P, Clark MA, Hayes AJ, Fisher C, et al. (2005) Surgical management of primary and recurrent retroperitoneal liposarcoma. Br J Surg92: 246-252.
- Lewis JJ, Leung D, Woodruff JM, Brennan MF (1998) Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg228: 355-365.
- Mendenhall WM, Zlotecki RA, Hochwald SN, Hemming AW, Grobmyer SR, Cance WG (2005) Retroperitoneal soft tissue sarcoma. Cancer 104: 669-675.
- Kim ES, Jang SH, Park HC, Jung EH, Moon GB(2010)Dedifferentiated Liposarcoma of the Retroperitoneum. Cancer Res Treat42:57-60.
- Fletcher CM, Akerman P, Cin I, de Wever I, Mandahl N, et al. (1996) Correlationbetween clinical pathological features and karyotype in lipomatous tumors. Am J Pathol 148: 623-630.
- Tateishi U, Hasegawa T, Beppu Y, Satake M, Moriyama N (2003) Primary dedifferentiated liposarcoma of the retroperitoneum. Prognostic significance of computed tomography and magnetic resonance imaging features. J Comput Assist Tomogr 27:799-804.
- Nascimento AG (2001) Dedifferentiated liposarcoma. SeminDiagnPathol18: 263-266.
- Lahat G, Anaya DA, Wang X, Tuvin D, Lev D, Pollock RE(2008)Resectable Well-differentiated versus Dedifferentiated Liposarcomas: Two Different Diseases Possibly requiring Different treatment approaches. Ann SurgOncol6:1585-1593.
- Zhang WD, Liu DR, Que RS, Zhou CB, Zhan CN, et al. (2015) Management of retroperitoneal liposarcoma: A case report and review of the literature. OncolLett 10:405-409.
- Park JO, Qin LX, Prete FP, Antonescu C, Brennan MF, Singer S (2009) Predicting outcome by growth rate of locally recurrent retroperitoneal liposarcoma: the one centimeter per month rule. Ann Surg 250: 977-982.
- Maamouri N, Cheikh I, Ouerghi H, Oukaà A, Belkahla N, Mnif E (2005) Giant retroperitoneal liposarcoma.One case report. Rev Med Interne 26: 145-148.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 8660
- [From(publication date):
February-2017 - Apr 11, 2025] - Breakdown by view type
- HTML page views : 7743
- PDF downloads : 917