Case Report Open Access
Giant Cell Tumor in a Patient with Osteopetrosis: A Case Report
Andalib A1 and Rahimian A2*1Department of Orthopedics, Al-Zahra Hospital, Isfahan University of Medical Sciences, Isfahan, Iran
2Spinal Surgery subspecialist, Department of Orthopedics, Al-Zahra Hospital, Isfahan University of Medical Sciences, Isfahan, Iran
- *Corresponding Author:
- Rahimian A
Department of General Surgery, Al-Zahra Hospital, Sofeh street
Isfahan, Iran
Tel: +989166318339
E-mail: rahimian521@gmail.com
Received date: August 27, 2017; Accepted date: September 05, 2017; Published date: September 12, 2017
Citation: Andalib A, Rahimian A (2017) Giant Cell Tumor in a Patient with Osteopetrosis: A Case Report. J Orthop Oncol 3:122. doi:10.4172/2472-016X.1000122
Copyright: © 2017 Andalib A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Orthopedic Oncology
Abstract
Introduction: Osteopetrosis, a rare disorder due to osteoclast dysfunction, which causes bone resorption dysfunction. These patients have brittle bones prone to osteomyelitis.
Case presentation: A 14-years male referred with complaint of chronic low back pain. He was treated with analgesics but with no pain relief, thus imaging was requested and a mass at the site of left body and pedicle of L5 was detected. The patient underwent tumor resection. The mass was diagnosed as giant cell tumor (GCT).
Conclusion: Due to the association of osteoclast dysfunction with both GCT and osteopetrosis, patients with osteopetrosis may be at higher risk of GCT.
Keywords
Osteopetrosis; Giant cell tumor; Osteoclast dysfunction
Introduction
Osteopetrosis, marble bone or Albers-Schonberg disease, all are names of an inherited disorder which happens due to osteoclast dysfunction that causes less bone resorption, thus increased bone density and hardening [1]. This extremely rare disorder is estimated to be inherited 1 in 100000 to 500000 births [2].
Osteopetrosis has two main types, autosomal recessive and autosomal dominant. Malignant type is autosomal recessive associated with infantile or early childhood death while autosomal dominant form is benign and patients usually present few or even no symptoms. There is another intermediate recessive type with less severe symptoms [3].
This disorder is usually diagnosed clinically, thorough radiological imaging. The characteristic finding of spine imaging is called “sandwich vertebrae” which is associated with demonstration of vertebral endplate sclerosis and central vertebral body lucency [4]. Contrary to expectation, patients with osteopetrosis have brittle bones and are also prone to osteomyelitis [5].
Case Presentation
In June, 2016, a fourteen year-old Iranian male was admitted to Kashani Hospital affiliated to Isfahan University of Medical Sciences for a chronic low back pain evaluation. The patient was aware of his disease and consumed calcium capsules prescribed for spontaneous fracture prevention that is usual in these patients. The patient was complaining from a six-month low back pain that was not cured in previous visits as general practitioners hypothesized that this pain is associated with his underlying disease or is musculoskeletal. Thus the patient was recommended to use analgesics (e.g. NSAIDS). He mentioned pain relief by these medications but the hallmark that was considered by orthopedist was pain exacerbation occurred at night and also as he lied supine. The patient was suspected to have primary spinal tumor or metastasis. Therefore, tumor work up was considered for him.
In examinations the orthopedist found point tenderness in percussion of fifth lumbar spine. Other examinations including; spinal flexion, extension and lateral bending was normal.
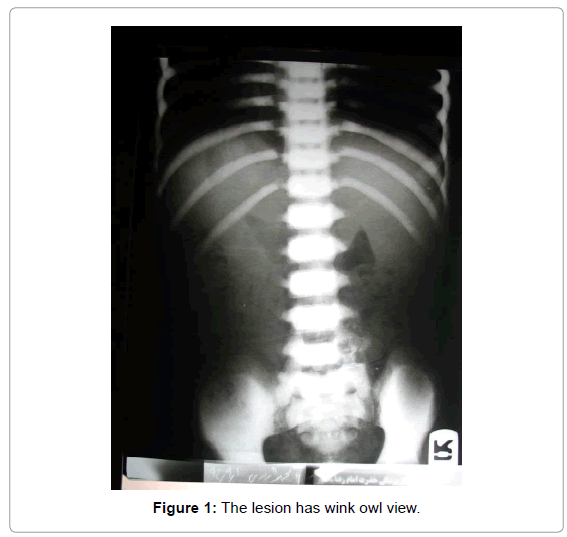
The findings of spinal X-ray radiography were characteristic for osteopetrosis and in left region of fifth lumbar (L5) vertebral, an expansile osteolytic lesion with involvement of body and pedicle was seen. The lesion has wink owl view (Figure 1).
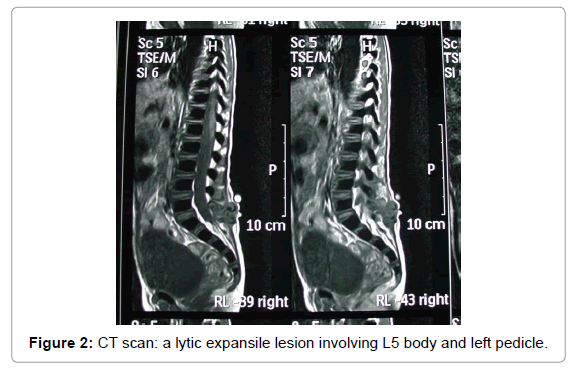
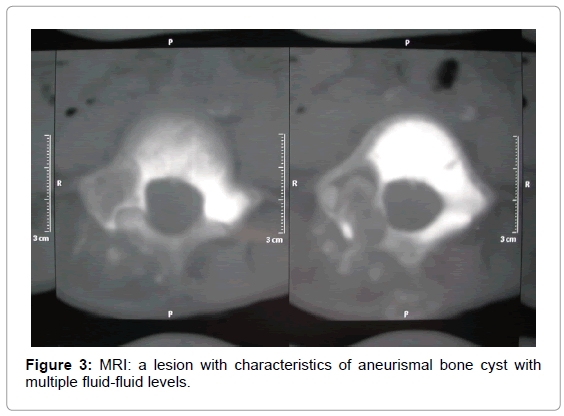
According to radiography, a computed tomography (CT-scan) and magnetic resonance imaging (MRI) were requested. Reports of these two modalities were as following;
CT scan: a lytic expansile lesion involving L5 body and left pedicle (Figure 2).
MRI: a lesion with characteristics of aneurismal bone cyst with multiple fluid-fluid levels (Figure 3).
Laboratory tests including; lactate dehydrogenase, alkaline phosphatase, calcium and phosphorus were checked. All of them were in normal range. In addition to these tests, the patient was sent for a whole bone scan and report indicated no bone metastasis.
By primary bone tumor confirmation, the patient was admitted for tumor resection operation. The patient underwent general anesthesia achieved by propofol (2-3 mg/kg.min). After anesthesia, patient was placed in prone position, the midline skin incision was made posteriorly, then fascia was incised in midline, paraspinal muscles were retracted and midline laminectomy from under surface of cephalad lamina to caudal was done. Pathologic tissue with safe margin was removed and sent to pathologist. Then after irrigation and meticulous hemostasis, three layer closure of wound was done.
The resected tumor was sent to pathology and the tumor was diagnosed as giant cell tumor (GCT). Thus no other follow-up medication (e.g. chemoradiation) was needed.
By the end of procedure, 10 mg/kg cephazolin was injected every 6 hours for 24 hours and patient was ordered to use thoracolumbosacral orthosis for 3 months. In three-month follow-up the patient presented pain relief and no other complaint due to surgery.
Discussion
Osteopetrosis refers to group of rare hereditary disorders with underlying bone metabolism dysfunction. Normal bone metabolism is achieved by balanced functioning of both osteoblasts and osteocalsts that play role in bone formation and resorption respectively. Osteopetrosis occurs when bone resorptin is impaired but the exact mechanism of this osteoclast dysfunction is unknown [6].
In malignant type of osteopetrosis the patient dies in infancy or in first life decade due to sepsis or pancytopenia posed by bone expansion, thus bone marrow filling [7]. Benign form causes less symptoms but the only available way for improving these cases survival is supportive care [3].
The most important complications of benign osteopetrosis are fractures in 78% of patients and chronic osteomyelitis in 10% (5). This study is about a 14 year-old male with osteopetrosis diagnosed with giant cell tumor (GCT) located in fifth lumbar vertebral body. This patient was complaining from a chronic low back pain exacerbated at nights. The number of studies about bone tumor occurrence in osteopetrosis is a few. But in general GCT is associated with genes which are highly expressed on stromal cells. Also these stromal cells are responsible for recruitment and maturation of osteoclasts from precursors [8]. As mentioned above osteoclastic dysfunction plays the most important role in osteopetrosis.
GCT should be removed from the patient’s body and was done by laminectomy from under surface of cephalad lamina to caudal and then pathologic tissue with safe margin was removed. Bone fractures are the most significant complication of this disorder and bone repair was really important in this patient as iatrogenic fractures can occur in osteopetrotic patients easily [9]. In order to achieve best bone repair, 3 month thoracolumbosacral orthosis was used for patient.
Conclusion
In conclusion, due to the association of osteoclast dysfunction with both GCT and osteopetrosis, patients with osteopetrosis may be at higher risk of GCT and also other osteoclastic related bone tumors. In current case by consideration of underlying osteopetrosis disorder, early diagnosis of tumor and operating appropriate procedure for tumor resection and bone repair, the patient relieved from pain.
Acknowledgment
We are grateful to Alzahra Hospitals’ nurses and employees.
Conflict of Interest
No Conflict of interest.
References
- Arumugam E, Harinathbabu M, Thillaigovindan R, Prabhu G (2015) Marble bone disease: a rare bone disorder. Cureus 7.
- Yadav S, Chalise S, Chaudhary S, Shah GS, Gupta MK, et al. (2016) Osteopetrosis in two siblings: two case reports. BMC research notes 9: 1.
- Coudert AE, de Vernejoul MC, Muraca M, Del Fattore A (2015) Osteopetrosis and its relevance for the discovery of new functions associated with the skeleton. International journal of endocrinology 20: 115.
- Kirkland JD, O’Brien W (2015) Osteopetrosis–Classic Imaging Findings in the Spine. Journal of clinical and diagnostic research: JCDR 9: TJ01.
- Liu YP, Lin XH, Yan MY, Lin BQ, Zhuo MY (2016) Debridement in chronic osteomyelitis with benign osteopetrosis: A case report. Experimental and Therapeutic Medicine 12: 2811-2814.
- Lam DK, Sándor GK, Holmes HI, Carmichael RP, Clokie CM (2007) Marble bone disease: a review of osteopetrosis and its oral health implications for dentists. Journal of the Canadian Dental Association 73: 839-448
- García CM, García MAP, García RG, Gil FM (2013) Osteomyelitis of the Mandible in a Patient with Osteopetrosis. Case Report and Review of the Literature. Journal of maxillofacial and oral surgery 12: 94-99.
- Tkins GJ, Haynes DR, Graves SE, Evdokiou A, Hay S, et al. (2000) Expression of osteoclast differentiation signals by stromal elements of giant cell tumors. Journal of Bone and Mineral Research 15: 640-649.
- van Hove RP, de Jong T, Nolte PA (2014) Autosomal dominant type I osteopetrosis is related with iatrogenic fractures in arthroplasty. Clinics in orthopedic surgery 6: 484-488.
Relevant Topics
- 3D Printing in Limb-Sparing Surgery
- Adamantinoma
- Aneurysmal Bone Cysts
- Chondrosarcoma
- Chordomas
- Cryosurgery
- Enchondroma
- Ewing’s Sarcoma
- Fibrous Dysplasia
- Giant Cell Tumor of Bone
- Immunotherapy for Osteosarcoma
- Liquid Biopsy in Orthopedic Oncology
- Malignant Osteoid
- Metastatic Bone Cancer
- Molecular Profiling of Bone Tumors
- Multilobular Tumour of Bone
- Orthopaedic Oncology
- Osteocartilaginous Exostosis
- Osteochondrodysplasia
- Osteoma
- Osteonecrosis
- Osteosarcoma
- Primary Bone Tumors
- Sarcoma
- Secondary Bone Tumours
- Targeted Therapy in Bone Sarcomas
- Tumours of Bone
Recommended Journals
Article Tools
Article Usage
- Total views: 3252
- [From(publication date):
September-2017 - Jul 06, 2025] - Breakdown by view type
- HTML page views : 2393
- PDF downloads : 859