Case Report Open Access
Giant Abdominal Wall Pseudocyst with Recurrent Incisional Hernia Following Mesh Repair Hernioplasty
Amey Narkhede, Sapna S. Marda, Ankit Balani*, Surendar Alwala, Milap Shah, RajeshwariZanke, Sandhya Sarjare and Anjani Kumar
Department of Radiology, Yashoda Hospital, Secunderabad, Telangana, India
- *Corresponding Author:
- Ankit Balani
61, Shyam Nagar
Pal Link Road
Jodhpur, Rajasthan, India
Tel: +91-9951853242
E-mail: drankitbalani@gmail.com
Received date: August 25, 2015 Accepted date: September 22, 2015 Published date: September 27, 2015
Citation: Narkhede A, Marda SS, Balani A, Alwala S, Shah M, et al. (2015) Giant Abdominal Wall Pseudocyst with Recurrent Incisional Hernia Following Mesh Repair Hernioplasty. J Gastrointest Dig Syst 5:349. doi:10.4172/2161-069X.1000349
Copyright: © 2015 Narkhede A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
We report clinical details and imaging findings of a case of giant pseudocyst occurring in the anterior abdominal wall as a late complication following mesh repair of incisional hernia in a 36-year-old female. Findings included a giant well encapsulated cyst lacking an epithelial lining filled with brownish coloured fluid and histopathology confirming an inflammatory reaction.
Keywords
Abdominal wall pseudocyst; Incisional hernia; Mesh repair; Contrast enhanced computed Tomography
Introduction
Repair of hernias is one of the common surgical procedures performed worldwide. Incisional hernia is mostly repaired by implanting a synthetic mesh to cover the hernial defect and reinforcing the abdominal wall to prevent recurrence [1]. The most commonly performed procedure is the placement of polypropylene mesh by onlay technique [2].
The most common complications include seromas and hematomas [3]. One of the rare late complications after mesh repair is formation of giant pseudocyst. This complication was first described in 1993 by Waldrep et al. [4].
According to some authors this might not be such a rare complication as thought to be instead its incidence may have been underestimated due to underreporting [5]. Hence we wish to propose consideration of pseudocyst formation as a late complication following mesh repair surgery for incisional hernias.
Case Report
A 36-year-old non-diabetic, obese female presented to the surgical out-patient department of our hospital with the chief complaint of a huge lump originating from the lower anterior abdominal wall. There was history of gradual increase in the size of the mass over a period of one year. There were no other complaints.
She had undergone incisional hernioplasty one and a half years back using a polypropylene mesh for the repair.
The patient was evaluated further with ultrasound of abdomen and pelvis which revealed a large, well-defined, cystic lesion of approximate size 20 x 18 cms (mediolateral X anteroposterior) with thick septae and low level internal echoes within.
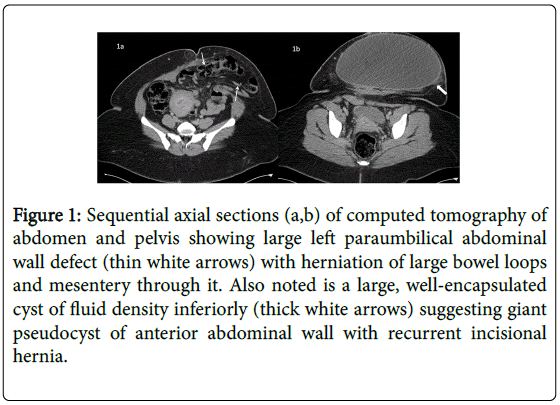
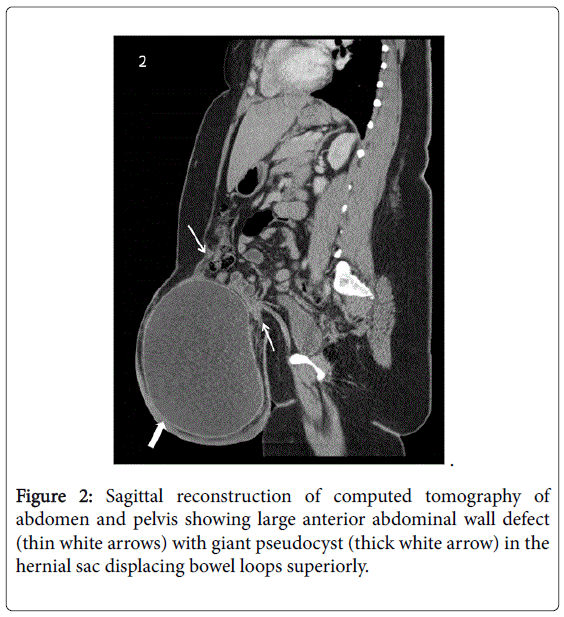
There was no evidence of any solid/vascular component in the lesion. The computed tomography (CT) of abdomen and pelvis showed a large left para and supra umbilical hernia with herniation of omentum, large bowel loops, small bowel loops and its mesentery with the abdominal wall defect measuring 62 x 67 mm (mediolateral x superoinferior).
A large well encapsulated cyst of size 24 x 15 x 21 cm (mediolateral x anteroposterior x superoinferior) was noted within hernial sac inferiorly with bowel loops along its superior aspect. There was no evidence of bowel obstruction/strangulation in the present study.
The patient was explored surgically and the cyst was completely excised with closure of the underlying defect in the abdominal wall. Brownish coloured turbid fluid was aspirated from the cyst which showed a predominance of cyst macrophages, few histiocytic giant cells admixed with few neutrophils which were typical of inflammation.
There was no bacterial growth in culture of the fluid after 1 week of incubation (Figures 1 and 2).
Figure 1: Sequential axial sections (a,b) of computed tomography of abdomen and pelvis showing large left paraumbilical abdominal wall defect (thin white arrows) with herniation of large bowel loops and mesentery through it. Also noted is a large, well-encapsulated cyst of fluid density inferiorly (thick white arrows) suggesting giant pseudocyst of anterior abdominal wall with recurrent incisional hernia.
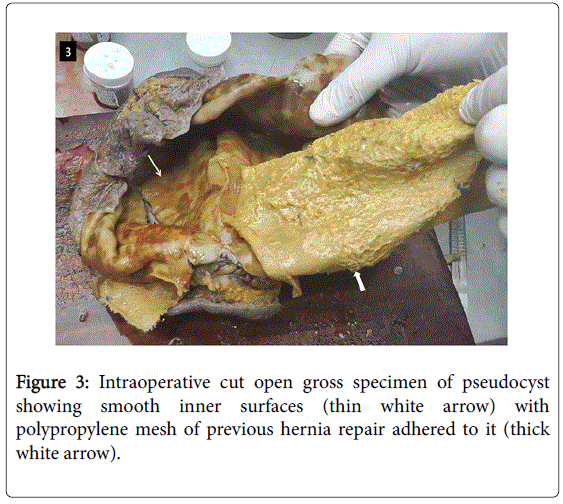
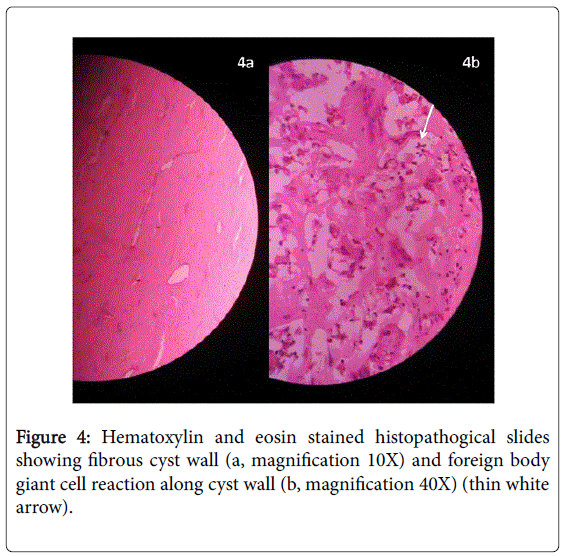
The excised specimen was sent for histopathological examination. Gross examination of the frozen section showed that the external and the inner surfaces were smooth. The inner surface showed the polypropylene mesh of previous hernia repair adhered to it. The microscopic examination of multiple sections showed collagenous tissue devoid of lining epithelium. Granulation tissue was seen. The wall showed congested blood vessels. Hemosiderophages were seen along with inflammatory cells and focal areas showed cholesterol cleft with giant cell reaction. No epithelial lining was seen lining the cyst (Figure 3).
These features confirmed the anterior abdominal wall lump to be a pseudocyst of anterior abdominal wall following mesh repair surgery (Figure 4).
Discussion
The placement of mesh for the repair of incisional hernia is related to development of few complications. The most common complication being fluid collections which may either contain serous fluid(seromas) or blood (hematomas) seen in the early post operative period [3]. Their formation is associated to both the surgical procedure performed and the type of mesh used [6].
Seromas are serous fluid collections occurring in the early post operative period. According to the recent studies an incidence of 17% [7] has been reported. Usually seromas tend to resolve within 8 weeks. If they persist for a longer period percutaneous aspiration is done. The other indications for aspiration of seromas include pain and infection. The CT appearance of seroma is a fluid density collection located deep to the prosthetic mesh usually with thin enhancing rim whereas hematomas are similar blood collections appearing hyperdense on plain CT.
One of the late occurring complications is the formation of pseudocyst which is rarely reported. The etiology is unclear and postulated to be related to long standing unresolving seroma or hematoma [8]. Some authors have proposed that it does not have any relation to the properties of mesh used or to the technique of mesh repair, however, a few are of the opinion that its occurrence might be related to use of polypropylene mesh [9]. On CT pseudocyst appears as a well defined fluid density collection usually located adjacent to the hyperdense prosthetic mesh. It may sometimes be seen along with the displacement of mesh leading to the recurrence of hernia. The pseudocyst contains brownish coloured turbid fluid which on cytopathology shows predominance of inflammatory cells with no bacterial growth on culture as seen in our case. Thus the formation of pseudocyst can be considered an inflammatory response to chronic long standing pathology.
Pseudocysts are unresponsive to aspiration with high incidence of recurrence after aspiration [4]. The only definitive treatment is complete cyst excision. It is also suggested that the use of minimally invasive surgical procedures and sublay technique of mesh placement can prevent formation of pseudocysts [10].
References
- Houck JP, Rypins EB, Sarfeh IJ, Juler GL, Shimoda KJ (1989) Repair of incisional hernia. SurgGynecolObstet 169: 397-399.
- Kingsnorth AN, Shahid MK, Valliattu AJ, Hadden RA, Porter CS (2008) Open onlay mesh repair for major abdominal wall hernias with selective use of components separation and fibrin sealant. World J Surg 32: 26-30.
- Lelpo B, Cabeza J, Jimenez D, Delgado I, Torres AJ. Abdominal pseudocyst complicating incisional hernia repair: our experience and literature review. Hernia : the journal of hernias and abdominal wall surgery 15: 233-7.
- Waldrep DJ, Shabot MM, Hiatt JR (1993) Mature fibrous cyst formation after Marlex mesh ventral herniorrhaphy: a newly described pathologic entity. Am Surg 59: 716-718.
- Omundsen M, Zargar H, Purchas S (2008) Giant cyst: an underreported complication of hernia mesh repairs? ANZ J Surg 78: 822-823.
- Lin BH, Vargish T, Dachman AH (1999) CT findings after laparoscopic repair of ventral hernia. AJR Am J Roentgenol 172: 389-392.
- Bendavid R (1998) Complications of groin hernia surgery. SurgClin North Am 78: 1089-1103.
- Arya N, Batey NR (1998) Pseudocyst formation after mesh repair of incisional hernia. J R Soc Med 91: 647-649.
- Hoefkens MF, Vles WJ (2008) [A giant pseudocyst following repair of an incisional hernia by a propylene mesh]. Ned TijdschrGeneeskd 152: 216-220.
- Sahin-Tóth G, Halász T, Viczián C, Oláh T (2007) [Late complication after mesh repair of incisional hernias: pseudocyst formation]. MagySeb 60: 293-296.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 12825
- [From(publication date):
December-2015 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 11967
- PDF downloads : 858