Case Report Open Access
GERD: A Debated Background of Achalasia
Laura Bognar*, Ors Peter Horvath, Gabor Jancso and Andras Vereczkei
Department of Surgery, University of Pecs, Pecs, Hungary
- *Corresponding Author:
- Dr. Laura Bognár
Department of Surgery, University of Pécs, Pécs
7624, Pécs, Ifjúság Street 13, Hungary
Tel: +3672533126
E-mail: laura.bognar@pte.aok.hu
Received date: Apr 25, 2016; Accepted date: May 20, 2016; Published date: May 27, 2016
Citation: Bognar L, Horvath OP, Jancso G, Vereczkei A (2016) GERD: A Debated Background of Achalasia. J Gastrointest Dig Syst 6:432. doi:10.4172/2161-069X.1000432
Copyright: © 2016 Bognar L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Achalasia is a primary esophageal motility disorder of unknown etiology, characterized by aperistalsis of the esophageal body and impaired lower esophageal sphincter (LES) relaxation. Available data suggest that the disease is multifactorial, but the exact initiating factors that may play a role in the development of the disease remain unclear. Case presentation: We report the case of a 65 year-old woman who had typical reflux symptoms with heartburn and regurgitation for about seven years. During the year before her admission to our clinic her reflux symptoms resolved and dysphagia developed. Endoscopy revealed esophageal dilatation with erosive esophagitis, narrowed cardia and hiatal hernia. Barium swallow test, manometry and 24 hour pH monitoring confirmed the development of achalasia with accompanying gastroesophageal reflux disease (GERD). The patient underwent laparoscopic surgery, the hiatal hernia was reconstructed and a Heller’s myotomy with a 360 degree Nissen fundoplication was performed. At the 3-year follow-up the patient was symptom free. Conclusion: Based on our experience and the review of the literature we believe that there is a cause-and-effect relationship between gastroesophageal reflux and the development of achalasia. In these cases a laparoscopic Heller’s myotomy completed with a 360 degree Nissen fundoplication should be the recommended surgical treatment to minimize the possibility of postoperative reflux disease.
Keywords
Achalasia; Case report; Gastroesophageal reflux disease; Nissen-Fundoplication
Abbreviations
GERD: Gastroesophageal Reflux Disease; HM: Heller’s Myotomy; LES: Lower Esophageal Sphincter; PPI: Proton Pump Inhibitor
Introduction
Achalasia is the most common primary esophageal motor disorder, resulting from the irreversible degeneration of inhibitory nerve endings in the myenteric plexus of the esophagus. This leads to aperistalsis or uncoordinated contractions of the esophageal body and failure of the lower esophageal sphincter to relax after swallowing. However achalasia is the best characterized esophageal motility disorder, its pathogenesis is still not entirely clarified. Though several studies have attempted to explore initiating agents that may play a role in the development of the disease, the exact factors responsible for the degeneration of ganglion cells in the myenteric plexus are poorly understood. Available data suggest that the disease is multifactorial, involving hereditary, autoimmune and environmental factors, such as viral infections [1]. Our hypothesis is that one possible initial insult that leads to the development of achalasia can be the gastroesophageal reflux disease. A previous study showed that antineuronal antibodies of very similar properties were found in the serum of both achalasia and GERD patients, therefore one can assume that the two diseases may not appear independantly of one another, but they may have common autoimmun mechanisms in their pathogenesis [2]. In another study, comparing LES muscle samples of reflux patients with those of a control group, Altorjay et al. revealed that reflux patients had enteric ganglionitis and smooth muscle hypertrophy at the gastroesophageal junction, and they suggested that these morphological changes might result in various functional esophageal diseases [3]. The theory that GERD could be an etiologic factor in the development of achalasia was first proposed by Smart et al. in 1986, who described 5 patients presenting with reflux, who subsequently developed achalasia over the years [4]. Based on our clinic’s experience and the review of the literature we suggest that in certain cases GERD can progress to achalasia. In these cases the treatment of choice should be different from that of pure achalasia patients.
Case Report
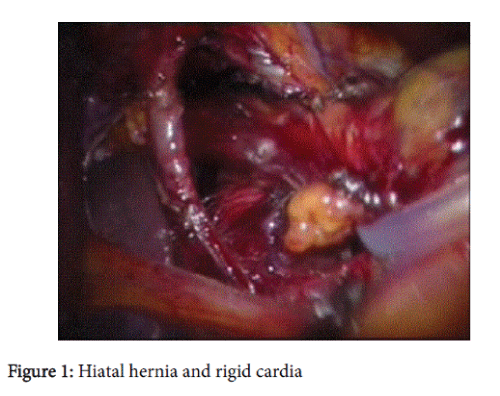
In the present case study we report a case of a 65 year-old woman. In her medical history she had typical reflux symptoms with heartburn and regurgitation for about seven years. She had no complaints of dysphagia at that time. She had her first upper gastrointestinal endoscopy two years before her admission to our clinic. Savary-Miller grade II esophagitis was described and the patient was put on PPI (Proton Pump Inhibitor) therapy. Control endoscopy the following year showed no signs of esophagitis, with normal cardia and stomach. Over the one year between the control examination and her admission to our clinic the patient’s reflux symptoms disappeared and dysphagia developed. Endoscopy revealed esophageal dilatation with erosive esophagitis, narrowed cardia and hiatal hernia. Biopsies from the distal esophagus showed chronic esophagitis and Barrett’s metaplasia. Barium swallow showed dilated esophageal body with decreased peristalsis, nonrelaxing sphincter and retention of barium. Manometry and 24-hour pH monitoring was performed. The LES pressure was 34.5 mmHg with 11.9% relaxation. 24-hour pH-metry showed acid reflux, with multiple sharp dips characteristic of typical gastroesophageal reflux, with total DeMeester score of 94.6. Using pH 3 as a discriminatory threshold for GERD the reflux score was 64.2. Achalasia and concomitant GERD was diagnosed and the patient underwent laparoscopic surgery. During operation an approximately 6 cm hiatal hernia and rigid cardia (Figure 1) were found. The hiatal hernia was reconstructed with four interrupted stitches, without mesh implantation, and a Heller’s myotomy with 360 degree Nissen fundoplication was performed. At the 2-year follow-up the patient was fine and had no dysphagia or reflux symptoms.
Discussion
Achalasia is a rare esophageal motor disorder of unknown etiology causing aperistalsis of the esophageal body and impaired deglutitive LES relaxation. This results in functional obstruction and dilatation of the esophagus. Unfortunately in many cases the diagnosis of achalasia is delayed. Clinical symptoms including heartburn and retrosternal pain can be observed in achalasia patients and these overlap with GERD symptoms [5].
However, there are a few reports where gastroesophageal reflux has been well documented to occur in patients prior to the development achalasia [4,6]. In our clinic, in the past 15 years we operated on 40 patients with achalasia and in 4 patients among them (10%) the etiologic role of reflux arose. Other reports showed that approximately 10-20% of untreated achalasia patients had abnormal acid exposure on pH monitoring [5-7]. Question rises how reflux can occur in untreated achalasia patients, as the two diseases represent opposite ends of abnormal LES function. Interestingly, the 24-hour pH-metry of our patient revealed prolonged reflux episodes during night, when the patient was in recumbent position. Therefore we presumed that a transient complete relaxation of the LES caused acid regurgitation from the stomach, and the poor clearance of the aperistaltic esophagus could result in such a prolonged acidification. This hypothesis is supported by Hirano et al. who demonstrated that transient LES relaxation can be observed in achalasia patients [8], explaining the observed pathologic acid exposures. However, the heartburn experienced by achalasia patients is not always due to real acid reflux, but can be also caused by lactate accumulation from food fermented by Lactobacillus in the dilated esophagus [7]. The pH of this fermented acid can be as low as 3.5 [9] and the onset of heartburn has been reported to occur at pH 4. In our case we used pH 3 as a threshold to distinguish real acid reflux from food fermentation. Even with the lower threshold, the DeMeester score was in the abnormal range.
Different observations support the idea that longstanding gastroesophageal reflux may truly preced and therefore be an etiologic factor in the development of achalasia. First, development of Barrett’s esophagus and even esophageal adenocarcinoma among untreated achalasia patients have been previously reported in the literature [10], which generally develop as a consequence of prolonged gastroesophageal reflux disease. Second, the coexistence of hiatal hernia and achalasia has already been described, and it is well known that hiatal hernia facilitates the development of GERD.
Achalasia is not curable; all the available treatments are palliative, aiming at relieving symptoms, improving esophageal emptying and preventing the development of megaesophagus. The commonly used treatments of achalasia involve pneumatic ballon dilatation, surgical myotomy with or without a fundoplication, and endoscopic botulinum toxin injection. The incidence of postoperative reflux is lower when a fundoplication is added to the laparoscopic myotomy. Still, questions arise why some patients have reflux after simple Heller’s myotomy (HM), while others haven’t. We suppose that reflux after Heller’s myotomy is not a failure and does not happen as a random fate. The frequency of reflux induced achalasia among all achalasia patients is considered to be around 6% to 11%. [8]. These values equal the frequency of reflux detected as a complication after Heller’s myotomy completed with partial fundoplication. One can assume that those patients who developed achalasia as a consequence of longstanding reflux disease will be more susceptible to develop postmyotomy or postdilatation reflux [11]. The role of GERD in other esophageal motility disorders, such as hypertensive lower esophageal sphincter has been recognized. Similarly, the cause-and-effect relation between GERD and Zenker diverticulum has been described in the literature. Evidence exists that long-standing reflux may evoke hypertension in the upper esophageal sphincter, as a protective reaction of the esophagus to defend the body from extended acid exposure and aspiration, and as a consequence leading to the formation of Zenker diverticulum [12]. In order to avoid postoperative reflux we propose to perform a 360 degree Nissen fundoplication instead of a partial fundoplication after HM in patients where GERD preceded the development of achalasia. This was performed in our patient and even at the 2-year follow-up no dysphagia or symptomatic GER was observed. This is in accordance with several studies that showed that 360 degree fundoplication is not an obstacle to esophageal emptying after laparoscopic Heller’s myotomy [13], achieving excellent results in terms of dysphagia, while Nissen fundoplication seems superior to partial fundoplication in preventing postoperative esophageal acid exposure [14].
In summary, based on the facts that similar antimyenteric neuronal antibodies were found in both achalasia and GERD patients, and just like in our case, reflux-associated diseases - such as Barrett’s esophagus and hiatal hernia - have been reported to occur in untreated achalasia patients, we suppose that the two diseases do not appear randomly at the same time, but there is a cause-and-effect relationship between them. In our report we presented a typical case of reflux induced achalasia, where the patient had reflux symptoms with heartburn for years, then these complaints resolved and dyphagia developed.
Acknowledgement
The authors would like to express their gratitude to Dr. Ágnes Király, Gastroenterologist colleague, who provided general support in writing the manuscript.
References
- Ghoshal UC, Daschakraborty SB, Singh R (2012) Pathogenesis of achalasia cardia. World J Gastroenterol 18: 3050-3057.
- Moses PL, Ellis LM, Anees MR, Ho W, Rothstein RI, et al. (2003) Antineuronal antibodies in idiopathic achalasia and gastro-oesophageal reflux disease. Gut 52: 629-636.
- Altorjay A, Szilagyi A, Arato G, Balazs P, Juhasz A, et al. (2006) Morphological changes in the lower esophageal sphincter influencing the result of antireflux surgical interventions in chronic gastroesophageal reflux disease. Hepatogastroenterology 53: 342-347.
- Smart HL, Mayberry JF, Atkinson M (1986) Achalasia following gastro-oesophageal reflux. J R Soc Med 79: 71-73.
- Anderson SH, Yadegarfar G, Arastu MH, Anggiansah R, Anggiansah A (2006) The relationship between gastro-oesophageal reflux symptoms and achalasia. Eur J GastroenterolHepatol 18: 369-374.
- Shoenut JP, Micflikier AB, Yaffe CS, Den Boer B, Teskey JM (1995) Reflux in untreated achalasia patients. J ClinGastroenterol 20: 6-11.
- Crookes PF1, Corkill S, DeMeester TR (1997) Gastroesophageal reflux in achalasia. When is reflux really reflux? Dig Dis Sci 42: 1354-1361.
- Hirano I, Tatum RP, Shi G, Sang Q, Joehl RJ, et al. (2001) Manometric heterogeneity in patients with idiopathic achalasia. Gastroenterology 120: 789-798.
- Streets CG, DeMeester TR (2003) Ambulatory 24-hour esophageal pH monitoring: why, when, and what to do. J ClinGastroenterol 37: 14-22.
- Guo JP, Gilman PB, Thomas RM, Fisher RS, Parkman HP (2002) Barrett's esophagus and achalasia. J ClinGastroenterol 34: 439-443.
- Horváth OP, Kalmár K, Varga G (2007) Reflux after Heller's myotomy for achalasia. Ann Surg 245: 502-503.
- Morales-Divo C, Jecker P, Lippert B, Mann WJ (2007) [Extraesophageal reflux in patients suffering from Zenker's diverticulum]. HNO 55: 546-550.
- Rossetti G, Brusciano L, Amato G, Maffettone V, Napolitano V, et al. (2005) A Total Fundoplication Is Not an Obstacle to Esophageal Emptying After Heller myotomy for Achalasia Results of a Long-term Follow Up. Ann Surg241:614-621.
- Wei MT, He YZ, Deng XB, Zhang YC, Yang TH, et al. (2013) Is Dor fundoplication optimum after laparoscopic Heller myotomy for achalasia? A meta-analysis. World J Gastroenterol 19:7804-7812.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 12046
- [From(publication date):
June-2016 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 11106
- PDF downloads : 940