Generation of Recombinant GroEL (HSP60) of Bacillus anthracis in Heterologous System E. coli and Evaluation of its Humoral Immune Response in Mouse Model
Received: 09-Jan-2020 / Accepted Date: 03-Feb-2020 / Published Date: 10-Feb-2020 DOI: 10.4172/2157-2526.1000165
Abstract
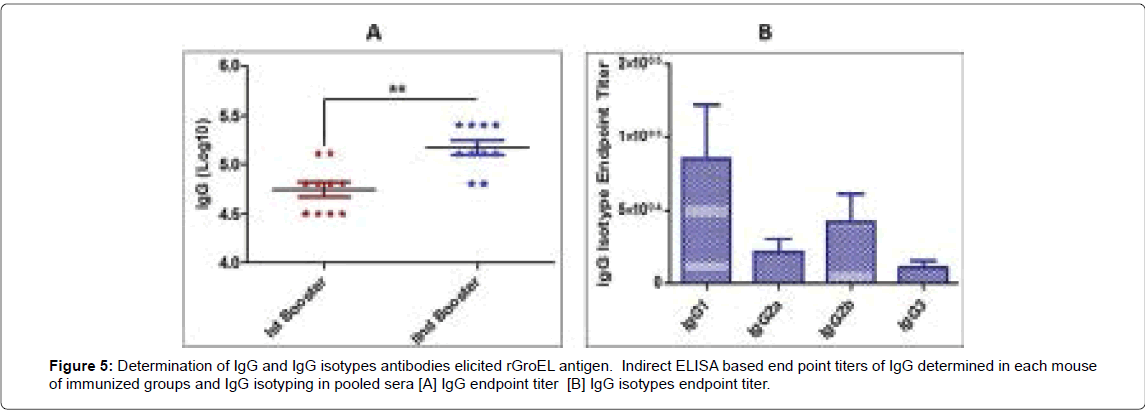
Anthrax, a disease of public health as well as bio-warfare potential is caused by Gram positive, non-motile and spore forming Bacillus anthracis. Bacteraemia and toxaemia of B. anthracis is responsible to cause lethality in anthrax-infected host. In this study, GroEL (HSP60) gene was cloned in pET28a+ vector and expressed in heterologous system E. coli. Over expressed recombinant GroEL was purified by IMAC chromatography and analysed on 10% SDS-PAGE. In western blot analysis, the rGroEL reacted with mouse anti-his antibody and anti-B. anthracis Sterne mouse serum. The immunogenicity of GroEL with aluminium hydroxide was evaluated in BALB/c mouse model. The endpoint titer of anti-rGroEL circulating antibodies in mouse serum was found high by indirect ELISA after first and second booster doses. IgG1 and IgG2b isotypes were found dominating in comparison to other isotypes. Humoral immune response generated by rGroEL indicated that it is immuno-dominant antigen of B. anthracis, which could be further evaluated as a subunit vaccine candidate against anthrax.
Keywords: Anthrax; Bacillus Anthracis; GroEL; HSP60; Vaccine
Introduction
Bacillus anthracis is a Gram-positive spore forming bacterium, which is the causative agent of deadly disease anthrax. In 19th century, Robert Koch for the first time isolated B. anthracis and explained its microbial and pathological etiology [1,2]. B. anthracis has potential to form rigid spores under adverse environmental conditions. B. anthracis spores are highly resistant to dehydration, high temperature, chemicals, high pressure and UV radiation. B. anthracis spores can maintain viability for decades in dormant state, and resume germination and rapid growth on getting favourable environment [3- 5]. Anthrax is an endemic disease, mainly in several agrarian countries. Anthrax is primarily a disease of domestic and wild animals, mainly grazing animals, and human is infected on coming in contact directly or indirectly with the diseased animals [6]. Clinical manifestations of human anthrax depend on the route of exposure of B. anthracis spores, which may be cutaneous, gastrointestinal, inhalational or injectional. Cutaneous anthrax causes up to 20% mortality, if not treated with antimicrobial agents. Ingestion of spore-contaminated food can cause gastrointestinal anthrax, which accounts about 25%- 60% mortality. The most fatal and fulminant manifestation of anthrax is due to inhalation of B. anthracis spores called as inhalational anthrax. Inhalational anthrax has the highest mortality even after antibiotics therapy. Injectional anthrax is caused by taking drugs with anthrax spores contaminated needles [1,6-8]. The pathogenesis of B. anthracis depends primarily on the two large virulent plasmids, pXO1 and pXO2, which harbour genes to encode anthrax toxins and a poly-Dglutamate capsule, respectively. Tripartite anthrax toxin i.e. Protective antigen (PA), Lethal factor (LF) and Edema factor (EF) are encoded by pXO1. PA is a central component of anthrax toxins and makes lethal toxin with LF, and edema toxin with EF. Zinc metalloprotease LF inactivates the MAPKK that impairs the signalling pathway and calmodulin dependent EF catalyzes the formation of cAMP from ATP which induces edema [9,10].
Due to ease of aerosolization, B. anthracis has been categorized as one of the top priority bio-warfare agents [11,12]. Anthrax has been used as bioweapon during World War-I and World War-II [6]. Since 2009, a new threat of anthrax has emerged throughout the Europe in the form of anthrax spore contaminated heroin needles in drug users [8].
In 1881, Louis Pasteur first developed live attenuated anthrax vaccine Pasteur I and Pasteur II. Afterwards, Max Sterne developed non-capsulated live attenuated B. anthracis Sterne spore vaccine [13]. Anthrax Vaccine Adsorbed/Biothrax (AVA) and Anthrax Vaccine Precipitated (AVP), acellular vaccines have been licensed in USA and UK for human use under the animal rule. AVA and AVP acellular vaccines are prepared from culture supernatant of pXO1+/pXO2‾ B. anthracis strains (V770-NP1-R or Sterne 34F2) which contains mainly PA with small amount of other bacterial proteins [14,15]. Despite of severe adverse effects of AVA and AVP vaccines, both vaccines induce long durable humoral and cellular immune response with annual boosters. Several studies have established that PA based vaccines generate immunity against toxin, but not against B. anthracis bacterium [16,17]. Several immunodominant antigens of B. anthracis have been identified to develop effective anthrax subunit vaccines. These immunodominant antigens of B. anthracis were evaluated as vaccine candidates either alone or in combination with PA [17-20].
Membranous and secreted antigens have been considered as potent vaccine candidate due to first line interaction between host and pathogen [21]. In the era of next generation subunit vaccine development, researchers are looking towards use of membrane component as well as secreted proteins to elicit humoral and cellular immune response. The heat shock protein, GroEL (HSP60) is present on the spore surface as well on bacterial membrane and in the secretome of bacteria [21-24].
Therefore, in the current study, GroEL (BA0267) gene of B. anthracis. was cloned and expressed in heterologous system E. coli. Recombinant GroEL protein was purified, and administered with aluminium hydroxide in BALB/c mice via subcutaneous route to study the humoral immune response. Immunological response elicited by GroEL indicated that GroEL is a potent immunodominant antigen of B. anthracis.
Materials and Methods
Ethical statement
All animal care and experimental procedures were conducted as per the approved protocols of Institutional Animal Ethics Committee (IAEC) of Defence Research and Development Establishment (Reg. No.37/Go/C/1999/CPCSEA) and Institutional Biosafety Committee (Protocol no. IBSC/12/BT/AKG/22). All the experimental mice were maintained in pathogen free facility.
Bacterial strains and vector
Strain of B. anthracis bearing plasmids pXO1 and pXO2 was isolated from cutaneous anthrax sample from Andhra Pradesh, India [25]. Glycerol stock of B. anthracis was streaked and grown on Brain Heart Infusion (BHI) agar plate at 37°C for 16 h. Genomic DNA of B. anthracis was isolated by using QIAamp DNA Mini Kit (Qiagen, USA). Bacterial strains viz. E. coli host strains BL-21 (DE3) and DH5α, and vector pET 28a+ were outsourced from Invitrogen and Novagen, USA.
Construction of recombinant plasmid of GroEL
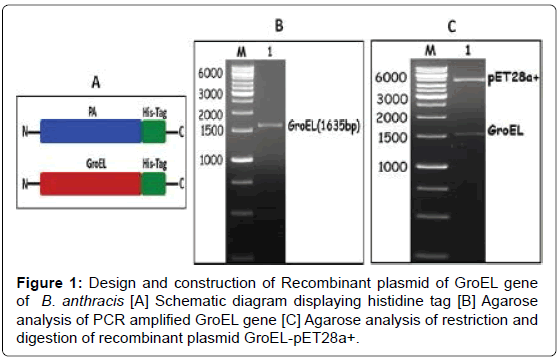
The gene of GroEL (1635 bp) was amplified from genomic DNA of B. anthracis using forward primer (5’-ATTCCATGGGCATGGCAAAAGATATTAAATTTAGTGAAG -3’) and reverse primers (5’-TTACTCGAGCATCATTCCGCCCATACC -3’) containing NcoI and XhoI restriction site, respectively. The PCR amplicon of GroEL and pET28a+ vector were digested individually using the respective aforementioned restriction enzymes. Ligation of digested inserts and vector was performed with T4 DNA ligase at 16 °C for overnight. Ligated plasmids were transformed into chemically competent E. coli DH5α cells and grown on Luria Bertani (LB) agar plate containing 50 μg/ml kanamycin. The positive clones of transformed E. coli DH5α were selected and recombinant plasmids were isolated using QIAprep Spin Miniprep Kit (Qiagen, USA).
Expression and localization of rGroEL
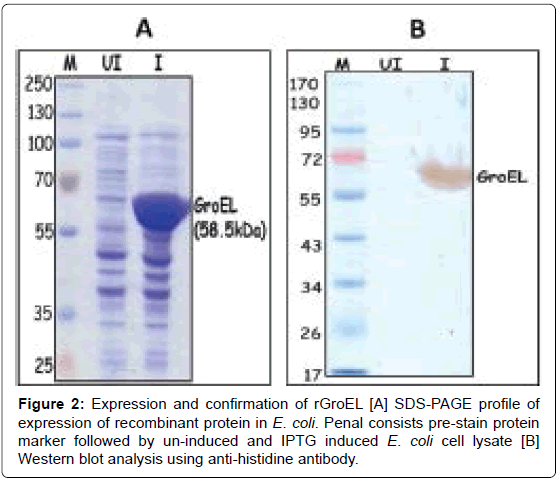
Recombinant plasmid GroEL-pET28a+ were transformed into chemically competent cells of E. coli BL21(DE3) and isolated colonies of GroEL were grown in LB broth containing 50 μg/ml kanamycin and induced at 0.6 optical density (OD) of cells with 1 mM Isopropyl β-D- 1-thiogalactopyranoside (IPTG; Sigma, USA) for 4 h at 37°C. Induced and un-induced culture pellets were harvested and analysed on 10% SDS-PAGE. Expression of recombinant GroEL was confirmed with Western blot using anti-His HRP conjugated antibody (Qiagen, USA). For localization, induced culture pallet was re-suspended in native lysis buffer (50 mM NaH2PO4, 300 mM NaCl and 10 mM imidazole) and physically lysed by using sonicator (BioLogics Inc., USA). Soluble fraction and pallets were analysed on 10% SDS-PAGE.
Purification of rGroEL
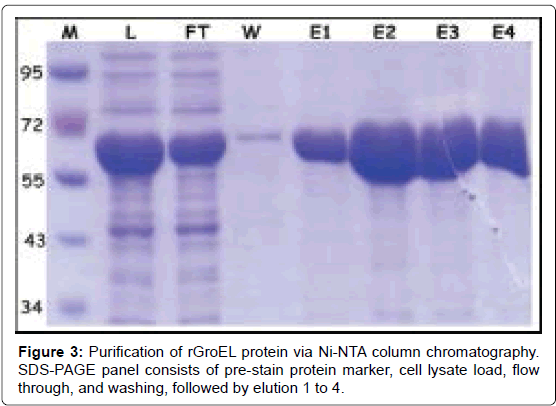
Purification of His-tagged recombinant GroEL was performed by immobilized metal affinity chromatography (IMAC) in native conditions. Pallet of GroEL was re-suspended in lysis buffer (50 mM NaH2PO4, 300 mM NaCl and 10 mM imidazole; pH-8) and lysed by sonicator. Soluble fraction of GroEL was added to equilibrate Ni-NTA column for binding followed by column washing with wash buffer (50 mM NaH2PO4, 300 mM NaCl and 20 mM imidazole; pH-8). After washing, the protein was eluted with elution buffer (50 mM NaH2PO4, 300 mM NaCl and 250 mM imidazole; pH-8). The purified rGroEL was analysed on 10% SDS-PAGE, dialysed and estimated by BCA method (Sigma, USA). The level of Lipo-polysaccharide (endotoxin) was measured by Limulus Amebocyte Lysate assay, and endotoxin free rGroEL antigen was used for immunizations.
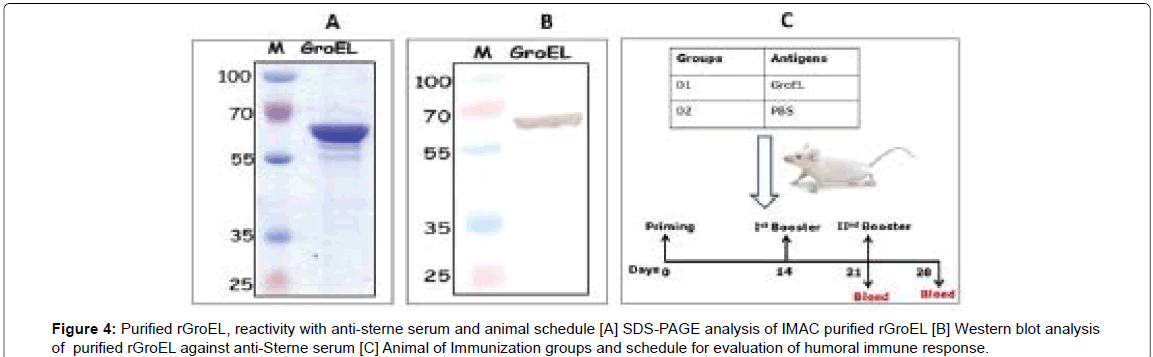
Interaction of rGroEL with serum generated against B. anthracis Sterne
Sub-lethal dose of B. anthracis Sterne spores was injected intraperitoneally on 0th day and 12th days in BALB/c mice (n=5). After second dose, serum was collected on 7th day. Purified rGroEL antigen was separated on 10% SDS-PAGE, transferred onto nitrocellulose membrane, treated with 1:1000 pooled anti-B. anthracis Sterne mouse serum, and probed with rabbit anti-mouse HRP conjugate antibody (Sigma, USA) followed by development with HRP substrate 3,3’-diaminobenzidine (DAB).
Mouse immunization
Six to eight weeks old female BALB/c mice were received from animal facility, DRDE, Gwalior and randomly grouped. Recombinant antigen GroLE was adsorbed on 0.35% aluminium hydroxide (Alhydrogel® adjuvant, InvivoGen, USA). One group of BALB/c mice (n=6) was immunized subcutaneously with 10 μg of aluminium hydroxide adsorbed GroEL. The second group of mice was kept as control and administered with PBS only (Figure 1A). Blood of animals was collected at day 0 (before immunization) and prime dose was given followed by two boosters on day 14 and 21. The serum of immunized mice was collected on day 21 (1st booster serum) and 28 (2nd booster serum, Figure 1A). Level of anti-GroEL IgG antibodies and its isotypes were determined in serum collected after first and second booster.
Determination of IgG and IgG subtypes antibodies
IgG and IgG subtypes of anti-GroEL were measured in hyper immune sera of first and second booster by indirect ELISA. Briefly, 96 well ELISA plate (Nunc-Immuno Plate, Denmark) were coated with 0.1 μg/well of rGroEL antigen in 0.1 M carbonate-bicarbonate buffer (pH 9.6) and incubated at 4 °C for overnight. Coated plates were washed thrice with 0.05% Tween-20 containing PBS (PBS-T) and blocked with 250 μl/well of 5% skim milk powder (Sigma, USA) in PBS for 1 h at room temperature (RT). Following three washes, 100 μl of mouse serum at different dilutions were added in triplicates and incubated for 1 h at RT. Unbound antibodies were removed by washing and 100μl of rabbit anti-mouse HRP conjugate (Sigma, USA) was added at a dilution of 1:10000.
For the subtyping of anti-GroEL antibodies (serum after second booster), sera were serially diluted from 1:1000 to 1:512000 and added in triplicates and incubated for 1 h at RT. The plates were washed and incubated with rabbit anti-mouse IgG1, IgG2a, IgG2b and IgG3 (Mouse monoclonal antibody isotyping reagents, Sigma, USA) as per manufacturer’s instructions. After 1 h of incubation, five times washed plates were incubated with 100 μl of o-phenylenediamine dihydrochloride (OPD; Sigma, USA) as HRP substrate for 10 min at RT and the reaction was stopped by 2N H2SO4. The absorbance was taken at 490 nm by ELISA reader (BioTek instruments, USA).
Statistical analysis
Statistical analysis of data and graphical representation was performed by GraphPad Prism 5 software. T-test method was used for statistical comparisons of data of different groups. Statistical significance was settled by the value of p (*p ≤ 0.05, **p ≤ 0.001).
Results and Discussion
Anthrax caused by Bacillus anthracis is a highly devastating disease, which is mainly found in agrarian countries. B. anthracis is considered as a bioterrorism agent due to its aerosolization and dissemination properties. Besides, it poses challenges to public health system also in the form of cutaneous anthrax. Several types of post-exposure prophylactic therapies are recommended for anthrax treatment including antibiotics and antitoxins. However, for pre-exposure therapy, only AVA or AVP vaccines are available. B. anthracis causes pathogenesis by two factors viz; toxins and bacterial sepsis. Current licensed anthrax vaccines (AVA and AVP) are effective mainly against anthrax toxins but probably provides limited protection against B. anthracis. So, it is desirable to include a component in vaccine which could provide protection against spores and vegetative cells to restrict the anthrax infection. Spore antigens and vegetative components of B. anthracis enhance the protective efficacy of PA based subunit vaccines. In order to develop next generation subunit vaccines, several recombinant antigens viz. Lethal Factor, Edema Factor, Extractable Antigen 1, Poly-D-glutamic acid, and BclA of B. anthracis have been evaluated for their ability to enhance protective efficacy of PA based vaccines [23]. In this study, we cloned and expressed the rGroEL (HSP60) of B. anthracis in E. coli for its immunological characterization in mouse model.
To prepare recombinant antigen, PCR amplified GroEL gene of B. anthracis was cloned in pET28a+ vector (Figures 1B and 1C). The location of histidine tag and open reading frame of GroEL has been shown in Figure 1A. The expressed recombinant GroEL protein (~58 kDA) was analysed on SDS PAGE and by Western blot with anti-His antibodies (Figures 2A and 2B). The recombinant GroEL was purified from soluble fraction of cell lysate using IMAC affinity chromatography (Figure 3). The yield of purified GroEL was approximately 15 mg/L (Figure 4A). The LPS contents in purified protein, as determined by Limulus Amebocyte Lysate assay were below 5EU/ml. Purified rGroEL reacted with anti-Sterne serum on PVDF membrane (Figure 4B). Thus, the reactivity of rGroEL with anti-Sterne serum corroborated that it is a potent immunogenic antigens of B. anthracis. Therefore, the immunogenicity of rGroEL was evaluated in mouse model to determine the humoral immune response. Immunological characteristics of rGroEL could be important parameters to develop subunit vaccine either alone or in combination with other antigens of B. anthracis against anthrax.
Specific immunological response elicited by subunit vaccine candidates is necessary to provide protection against pathogens. Humoral and cellular immune response relies upon the IgG and its isotypes secreted by plasma B cells, which efficaciously neutralize toxins and opsonize the free extracellular pathogens [26-28]. Aluminium hydroxide adsorbed rGroEL was administered in mice via subcutaneous route and evaluated its immunogenicity. In order to determine the inductive anti-GroEL antibodies, mice sera were collected separately from all the individual immunized mice (Figure 4C). The cut-off value of IgG titer was calculated from the mice sera of control group as the mean OD plus 2SD at 1:200 dilutions. Anti-GroEL antibodies in individual mouse serum of immunized animals were measured on 7th days after first and second boosters. All immunized animals generated significantly high endpoint IgG titers. The endpoint titers of IgG antibody in GroEL immunized animals were observed up to 1:48000 (Log 4.74 ± 0.230) and 1:170000 (Log 5.31 ± 0.20) after first and second boosters (Figure 5A). Significant IgG endpoint titer elicited by GroEL indicated that GroEL antigen evokes strong humoral immune response. Among IgG subclasses, higher titers of IgG1 and IgG2b than the titers of IgG2a and IgG3 indicate the Th2 type responses to a particular antigen [28]. In the present study, the titre of IgG1 and IgG2b subtypes were dominating over IgG2a and IgG3 (Figure 5B). IgG antibodies tires and IgG sub-class prolife against GroEL has established Th2 type immune response, which may play an important role in stimulation and maintenance of B cells.
Conclusion
In conclusion, the humoral immune response elicited by rGroEL indicated that it is potent immunodominant antigen of B. anthracis. Therefore, the GroEL could be used further for evaluation as subunit vaccine candidate either alone or in combination with other immunodominant antigens of B. anthracis against anthrax.
Conflict of Interest
The authors declare that they have no conflict of interest.
Acknowledgements
The authors are thankful to Director, DRDE, Gwalior for his keen interest, constant support and providing necessary facilities for this study (Acc no. DRDE/ BPT/41/2019). MK and NP are thankful to DRDO for providing Senior Research Fellowship.
References
- Moayeri M, Leppla SH, Vrentas C, Pomerantsev AP, Liu S (2015) Anthrax Pathogenesis. Annu Rev Microbiol 69:185-208.
- Nicholson WL, Schuerger AC (2005) Bacillus subtilis spore survival and expression of germination-induced bioluminescence after prolonged incubation under simulated Mars atmospheric pressure and composition: implications for planetary protection and lithopanspermia. Astrobiology 5:536-544.
- Setlow P (2006) Spores of Bacillus subtilis: their resistance to and killing by radiation, heat and chemicals. J Appl Microbiol 101:514-525.
- Moir A (2006) How do spores germinate? J Appl Microbiol 101 (3):526-530.
- Goel AK (2015) Anthrax: A disease of biowarfare and public health importance. World J Clin Cases 3:20-33.
- Ramsay CN, Stirling A, Smith J, Hawkins G, Brooks T, et al. (2010) An outbreak of infection with Bacillus anthracis in injecting drug users in Scotland. Euro Surveill 15 (2).
- Berger T, Kassirer M, Aran AA (2014) Injectional anthrax - new presentation of an old disease. Euro Surveill 19.
- Mikesell P, Ivins BE, Ristroph JD, Dreier TM (1983) Evidence for plasmid-mediated toxin production in Bacillus anthracis. Infect Immun 39:371-376
- Collier RJ (1999) Mechanism of membrane translocation by anthrax toxin: insertion and pore formation by protective antigen. J Appl Microbiol 87:283.
- Jernigan DB, Raghunathan PL, Bell BP, Brechner R, Bresnitz EA, et al. (2002) Investigation of bioterrorism-related anthrax, United States, 2001: epidemiologic findings. Emerg Infect Dis 8 (10):1019-1028.
- Inglesby TV, O'Toole T, Henderson DA, Bartlett JG, Ascher MS, et al. (2002) Anthrax as a biological weapon. JAMA 287 (17):2236-2252.
- Turnbull PC (1991) Anthrax vaccines: past, present and future. Vaccine 9:533-539.
- Plotkin S, Grabenstein JD (2008) Countering Anthrax: Vaccines and Immunoglobulins. Clin Infect Dis 46:129-136.
- Wright JG, Quinn CP, Shadomy S, Messonnier N, Centers for Disease C, Prevention (2010) Use of anthrax vaccine in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2009. MMWR Recomm Rep 59 (RR-6):1-30
- Friedlander AM, Little SF (2009) Advances in the development of next-generation anthrax vaccines. Vaccine 27:28-32.
- Whiting GC, Rijpkema S, Adams T, Corbel MJ (2004) Characterisation of adsorbed anthrax vaccine by two-dimensional gel electrophoresis. Vaccine 22:4245-4251.
- Liu X, Wang D, Ren J, Tong C, Feng E, et al. (2013) Identification of the immunogenic spore and vegetative proteins of Bacillus anthracis vaccine strain A16R. PLoS ONE 8:57959.
- Ghosh N, Goel AK, Alam SI (2014) Exoproteome analysis of a novel strain of Bacillus cereus implicated in disease resembling cutaneous anthrax. Infect Genet Evol 22:1-11.
- Varshney A, Puranik N, Kumar M, Goel AK (2016) The humoral immune response to various domains of protective antigen of Bacillus anthracis in cutaneous anthrax cases in India. Def Sci J 66:645-650.
- Sinha K, Bhatnagar R (2010) GroEL provides protection against Bacillus anthracis infection in BALB/c mice. Mol Immunol 48:264-271.
- Uchida M, Harada T, Enkhtuya J, Kusumoto A, Kobayashi Y, et al. (2012) Protective effect of Bacillus anthracis surface protein EA1 against anthrax in mice. Biochem Biophys Res Commun 421:323-328.
- Aggarwal S, Somani VK, Gupta S, Garg R, Bhatnagar R (2019) Development of a novel multiepitope chimeric vaccine against anthrax. Med Microbiol Immunol 208:185-195.
- Chitlaru T, Altboum Z, Reuveny S, Shafferman A (2011) Progress and novel strategies in vaccine development and treatment of anthrax. Immunol Rev 239:221-236.
- Varshney A, Kumar M, Nagar DP, Pal V, Goel AK (2019) Development of a novel chimeric PA-LF antigen of Bacillus anthracis, its immunological characterization and evaluation as a future vaccine candidate in mouse model. Biologicals 61:38-43.
- Tao P, Mahalingam M, Zhu J, Moayeri M, Kirtley ML, et al. (2017) A Bivalent Anthrax-Plague Vaccine That Can Protect against Two Tier-1 Bioterror Pathogens, Bacillus anthracis and Yersinia pestis. Front Immunol 8:687.
- Froude JW II, Thullier P, Pelat T (2011) Antibodies against anthrax: mechanisms of action and clinical applications. Toxins (Basel) 3 :1433-1452.
- Siegrist CA (2008) Vaccine Immunology (General Aspects of Vaccination).
Citation: Kumar M, Puranik N, Tripathi NK, Pal V, Goel AK (2020) Generation of Recombinant GroEL (HSP60) of Bacillus anthracis in Heterologous System E. coli and Evaluation of its Humoral Immune Response in Mouse Model. J Bioterror Biodef 11:165. DOI: 10.4172/2157-2526.1000165
Copyright: © 2020 Kumar M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2077
- [From(publication date): 0-2020 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 1353
- PDF downloads: 724