Case Report Open Access
Gastric Ulcer: An Old Disease - A New Cause
Silke Urban1*, Michael Manz1, Andreas Zettl2, Thomas Peters3, Katrin Baumann4 and Markus von Flüe1
1Gastrointestinal Unit , St. Claraspital Basel, Switzerland
2Department of Pathology Viollier AG, Switzerland
3Department of Endocrinology St. Claraspital Basel, Switzerland
4GP surgery Dr. K. Baumann Muttenz, Switzerland
- *Corresponding Author:
- Silke Urban
GI Unit, St. Claraspital Basel
Switzerland
Tel: 0041 61 685 8585
Fax: 0041 61 685 8182
E-mail: Silke.Urban@claraspital.ch
Received date: October 22, 2014; Accepted date: November 24, 2014; Published date: November 29, 2014
Citation: Urban S, Manz M, Zettl A, Peters T, Baumann K, et al. (2014) Gastric Ulcer: An Old Disease - A New Cause . J Gastrointest Dig Syst 4:241. doi:10.4172/2161-069X.1000241
Copyright: © 2014 Urban S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
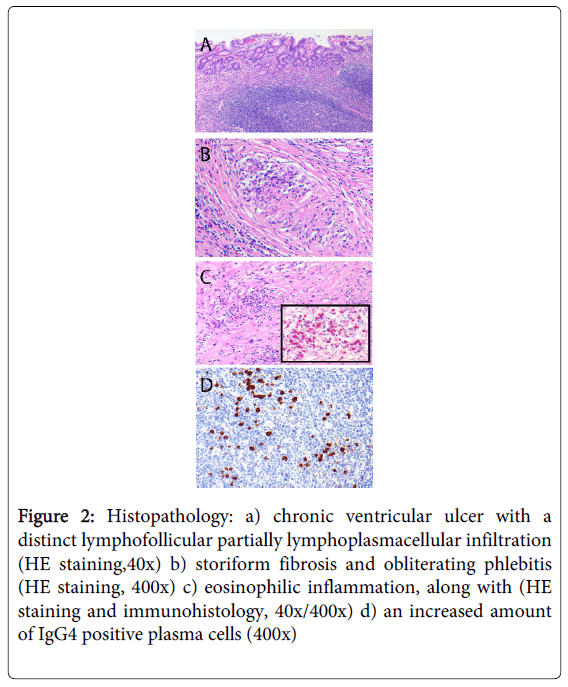
A 73 year patient presented with melena to our endoscopy unit. He was hemodynamically stable and the haemoglobin was decreased with 113 g/l. The remaining blood tests were normal. Upper endoscopy showed a large bleeding ulcer along the lesser curvature, macroscopically suspicious for malignancy. To control the bleeding and to rule out gastric cancer, the patient was referred to surgery. Two thirds of the stomach, a segment of the transverse colon with mesocolon had to be resected en bloc. Final histology revealed a chronic ventricular ulcer with a distinct lymphofollicular, lymphoplasmacellular and eosinophilic inflammation. The number of IgG4 plasma cells was increased (60 IgG4 positive cells per microscopic visual field, 70-80% IgG4 out of all IgGs). Storiform fibrosis and obliterating phlebitis were found not only within the ulcer base but also extensively in the adjacent soft tissue.
Summarizing, our patient suffered from a rare form of a chronic gastric ulceration as a manifestation of IgG4-related disease.
IgG4-related disease is an increasingly recognized condition presenting with specific pathological, serologic and clinical features. Its hallmark is the typical histopathological finding as in our case. Type 1 autoimmune pancreatitis and salivary gland disease are the two typical presentations, but IgG4-disease can affect each organ.
Because of no further organ involvement, consecutive immunosuppressant treatment was not required. Seven months later gastroscopy showed no signs of recurrence.
A gastric ulcer can be the first presentation of IgG4 related disease which needs to be considered as a differential diagnosis in refractory gastritis and cancer suspicious lesions.
Keywords
Gastric ulcer; Gastric cancer; IgG4 related Gastritis; IgG4 related disease
Description
A 73-year-old man presented to our endoscopy unit with melena. He complained of upper abdominal pain, which had started two months earlier, permanent fatigue, low appetite and some weight loss. Beyond this, his general health condition was fine.
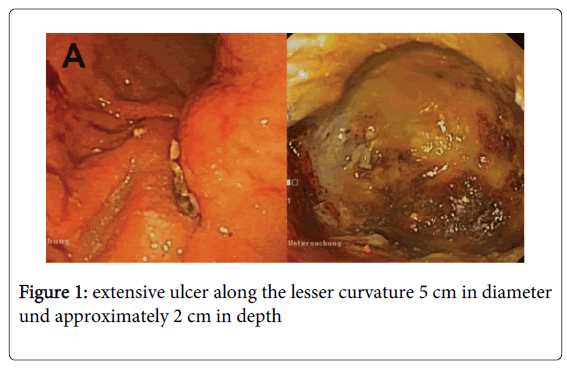
The GI bleeding was not life threatening, the haemoglobin was slightly decreased at 113 g/l. The remaining blood count, CRP, pancreatic enzymes, renal and liver function were normal. The upper panendoscopy revealed a huge bleeding ulcer along the lesser curvature (Figure 1). The biopsies showed pronounced chronic inflammation with plenty of eosinophils and scanty Helicobacter pylori without signs of malignancy.
CT scan showed the huge ulcer, enlarged perigastric lymphadenopathy and no distant metastases. To control chronic blood loss and to rule out definitely gastric cancer, we decided for surgical therapy.
Intraoperatively, a huge ulcer along the lesser curvature and dorsal gastric body infiltrating the transverse mesocolon was found. Perigastric lymph nodes were markedly enlarged. Two thirds of the stomach, a segment of the transverse colon including the mesocolon had to be resected en bloc.
Definite histology revealed a chronic gastric ulcer with a distinct lymphofollicular lymphoplasmacellular, eosinophilic infiltrate (Figure 2a), storiform fibrosis and obliterating phlebitis (Figure 2b/c) being indicative for IgG4 related disease. The latter could be confirmed by immunohistology with 60 IgG4 positive cells/ high power field (increased>30 cells/HPF) 3 and 70-80% IgG4/ IgG (increased>50%) (Figure 2c/d). In summary our patient suffered from a chronic gastric ulcer, a rare manifestation of IgG4-related disease.
Figure 2: Histopathology: a) chronic ventricular ulcer with a distinct lymphofollicular partially lymphoplasmacellular infiltration (HE staining,40x) b) storiform fibrosis and obliterating phlebitis (HE staining, 400x) c) eosinophilic inflammation, along with (HE staining and immunohistology, 40x/400x) d) an increased amount of IgG4 positive plasma cells (400x)
IgG4-related disease is an increasingly recognized condition presenting with specific pathological, serologic, and clinical features. Its hallmark is the histopathological finding of a lymphoplasmacytic tissue infiltrate with a predominance of IgG4-positive plasma cells accompanied by storiform fibrosis and obliterative phlebitis. Serum levels of IgG4 are often elevated. However, less than 40% of patients have normal serum IgG4 concentrations despite the presence of the classic histopathological changes in tissue [1]. Our case belonged to the latter minority with a normal IgG4-plasma level of 0.53 g/l (normal range 0.05–1.96 g/l).
IgG4-related disease affects mainly men (62 to 83%) aged over 50 and can involve multiple organs (in 60 to 90%) [2]. It usually presents subacutely or is found incidentally by radiology or histopathology. Most patients are not constitutionally ill; fever and raised CRP levels are uncommon. The disease was not recognized as a systemic condition until 2003, when extrapancreatic manifestations were identified in patients with autoimmune pancreatitis [3]. Even if type 1 autoimmune pancreatitis and salivary gland disease are the major presentations of this condition, it can affect any organ. Lymphoplasmacytic gastritis associated with autoimmune pancreatitis and chronic gastric ulceration has been described so far only by a few case reports [4,5].
The term, IgG4-related disease, now includes a number of medical conditions, until 2003 not known to be interrelated (Table 1) [3]. Mikulicz’s syndrome, Küttner’s tumor and Riedel’s thyroiditis may be reclassified in the future.
| List of previously described conditions being reclassified as “IgG4 related disease” 3 |
|---|
| Type 1 autoimmune pancreatitis IgG4-related sclerosing cholangitis Miculicz’s disease (sialadenitis) Sclerosingsialadenitis (Suttner’s tumor) Inflammatory orbital pseudotumor Chronic sclerosingdacryoadenitis (lacrimal glands) “Idiopathic” retroperitoneal fibrosis (Ormond’s disease) Chronic sclerosingaortitis and periaortitis Riedel’s thyroiditis IgG4-related interstitial pneumonitis and pulmonary inflammatory pseudotumors IgG4-related kidney disease IgG4- related hypophysitis IgG4-related pachymenigitis |
Table 1: List of IgG4 related disease.
Medical treatment includes glucocorticoids, azathioprine and mycophenolate [3].
In our case diagnosis was made by histopathology - the hallmark of IgG4-related disease (Figure 2). Clinical examination, laboratory tests und CT scan did not reveal further organ involvement, making immunosuppressant treatment unnecessary.
Seven months later gastroscopy showed no signs of recurrence; blood tests were within normal range.
Concluding gastric ulcer can be the first presentation of IgG4-related disease, which has to be considered as a differential diagnosis in refractory gastritis and cancer-suspicious lesions.
References
- Cheuk W, Chan JK (2010) IgG4 related sclerosing disease: a critical appraisal of an evolving clinicopathologic entity. AdvAnatPathol 2010; 17: 303-332.
- Sato Y, Ohshima K, Ichimura K, Sato M, Yamadori I, et al. (2008) Ocular adnexal IgG4-realted disease has uniform clinicopathology. PatholInt 58: 465-470.
- Stone JH, Zen Y, Deshpande V (2012) IgG4-related disease. N Engl J Med 366: 539-551.
- Uehara T, Hamano H, Kawa S, Sano K, Oki K, et al. (2010) Chronic gastritis in the setting of autoimmune pancreatitis. Am J SurgPathol 34: 1241-1249.
- Bateman AC, Sommerlad M, Underwood TJ (2012) Chronic gastric ulceration: a novel manifestation of IgG4-related disease? J ClinPathol 65: 569-570.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14768
- [From(publication date):
November-2014 - Dec 03, 2024] - Breakdown by view type
- HTML page views : 10384
- PDF downloads : 4384