Case Report Open Access
Gastric Desmoid Tumor: An Infrequent Case of Intra-Abdominal Fibromatosis
Macias N1, Abdel-lah O1*, Parreño FC1, Blanco O2, Bengoechea O2 and Martínez SC2
Gastric Esophageal Pathology Unit, Department of General Surgery and Gastroenterology, University Welfare Complex of Salamanca, Salamanca, Castilla y Leon, Spain
- *Corresponding Author:
- Dr. Omar Abdel-lah Fernández
Gastric Esophageal Pathology Unit
Department of General Surgery and Gastroenterology
University Welfare Complex of Salamanca
Salamanca, Castilla y Leon, Spain
Tel: +34 923261198
E-mail: omarabdellah@gmail.com
Received date: August 10, 2015 Accepted date: September 02, 2015 Published date: September 09, 2015
Citation: Macias N, Abdel-lah O, Parreño FC, Blanco O, Bengoechea O, et al. (2015) Gastric Desmoid Tumor: An Infrequent Case of Intra-Abdominal Fibromatosis. J Gastrointest Dig Syst 5:332. doi:10.4172/2161-069X.1000332
Copyright: © 2015 Macias N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background and purpose: Desmoid tumors or aggressive fibromatosis are infrequent conditions, with a large clinical variability, and preferencial location on abdominal wall, extra-abdominal soft tissue, and mesentery. Histologically benign but locally aggressive, they have a marked tendency to recurrence. There are two known variants: sporadic and associated to familial adenomatous polyposis. Its etiology remains unknown, but it appears to be related to estrogenic estimulation, surgical aggression and mutations of the short arm of chromosome 5. Diagnosis is usually difficult, and must combine medical history, semiology and imaging, though only histological analysis of the specimen will provide a definitive diagnosis after surgical resection, which is potentially curative. Gastric location has not been reported so far. Case report: 37-year-old woman with recent delivery, presenting abdominal lump with non specific clinical semiology and rapid growth rate. After diagnostic tests, a hypervascular mass of about 15 centimeter of diameter, depending on gastric wall is found. She underwent an elective distal gastrectomy and Billroth I reconstruction. Histology confirms a mesenchymal desmoid gastric tumor. Discussion: The differential diagnosis for abdominal oligosymptomatic lumps which respect the mucosa of the gastrointestinal tract lead clinical suspicion to mesenchymal tumors such as sarcomas, desmoids, or GIST. Radiologic tests are useful to confirm resectability and detect complications. When facing unresectable disease, planning a biopsy and systemic treatment with chemotherapy and/or radical radiotherapy should be considered. Diagnosis is reached after histological and inmunohistochemical analysis of the specimen, which in case of a desmoid, will show negative expression to markers of sarcoma (actin, desmin, S100) or GIST (CD117, DOG1, PDGFRA), and positive staining with anti-beta-catenin. Conclusion: Desmoid tumors should be considered in the differential diagnosis of abdominal oligosymptomatic masses, specially in fertile women or if history of surgical trauma. Patients with desmoid tumors should undergo colonic polyposis screening, as well as patients with adenomatous polyposis and an abdominal lump should lead suspected diagnosis to the possibility of a desmoid tumor.
Keywords
Neoplasms; Stomach; Abdominal fibromatosis; Desmoid; Gastrectomy
Introduction
Desmoid tumors are also known as deep fibromatosis, aggressive fibromatosis, or low grade fibrosarcoma (grade I fibrosarcoma). They are rare in clinical practice, with an incidence of 2.4 to 4.3 cases per million inhabitants. These tumors represent 0.03 to 0.1% of all neoplasms, and 1-3% of those affecting soft tissues [1-6]. They are more frequent on the third and fourth decades, specially in fertile women (O.R.: 1.6-2.5) [1,2,4,6]. Although they could theoretically arise from any muscular tissue in the human body, three preferent locations have been reported: abdominal wall (50%), extra-abdominal soft tissues in trunk or limbs (40%), and bowel wall and mesentery (10%) [1,5]. Histologically benign in appearance, they are locally aggressive, infiltrating surrounding structures with a slow-growing, well-differentiated miofibroblastic stroma [5,6]. They have a significant propensity for local recurrence (25-65%) even after complete surgical resection, and a low rate of spontaneous regression (4-17%), but no metastatic potential [1,7]. Their different and variable clinical presentations make early diagnosis a challenge for the clinician [1,5,6,7]. Desmoid tumors usually manifest as slow-growing, deepseated, painless or slightly painful masses that can develop at virtually any anatomical site. Usually unique tumors, multiple synchronic lesions have been described, and depending on their location, they can be a cause of significant complications or even death [1,5,6]. Despite all this, natural history of desmoids remains poorly understood, but they seem to be related to previous surgical aggression, trauma, and strogenic stimulation, along with genetic mutations in chromosome [5]. Desmoid tumor development has been associated with genetic predisposition in patients with familial adenomatous polyposis (FAP). In addition, sporadic cases of intra-abdominal desmoid tumors have been observed on sites of previous abdominal surgery. Therefore, a classification between two different types of desmoid tumors can be made: a sporadic variant and another associated with FAP [1-4,6-10]. FAP-associated cases usually occur in the abdomen, and can present with changes in bowel habits, pain, obstruction, ischemia, rectal bleeding, or a dysfunctional anastomosis, and are a significant cause of mortality for FAP patients. Sporadic cases present more frequently on shoulder, hips, and extremities, and have a better prognosis [1,4,5,6,9,11]. They can be multifocal on an extremity, but different anatomical regions rarely are affected in the same patient. Diagnosis of this kind of tumors can only be made through histological analysis of a biopsy or of the entire specimen after resection, with a sensitivity next to 90% [2,7]. Radiologic tests, such as CT scan and MRI are the most valuable tool prior to surgery, since they confirm the presence of the tumor and help to assess their resectability [1,4,6]. Surgical resection is still considered the first line of treatment when possible, and it is potentially curative if a complete R0 resection is achieved [3,6,7]. With satisfactory resection margins, recurrence rate ranges from 15 to 40%, while if they are compromised, recurrence might rise to 79%, usually within three years from diagnosis [1,2,5,6,7,9]. Unresectable or residual disease can be treated with radical radiotherapy. Systemic treatments with NSAIDs, anti - estrogens or androgens, chemotherapy (doxorubicin-based, methotrexate, vinblastine, vinorelbine), and lately imatinib have been used for unresectable or relapsed desmoids. The effectiveness of these systemic therapies remains unclear for unresectable disease, while results in recurrence are promising. In selected asymptomatic patients, a period of watchful observation could be recommended [4,6].
Case Report
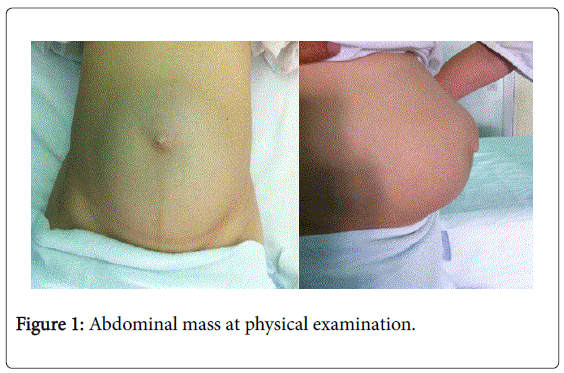
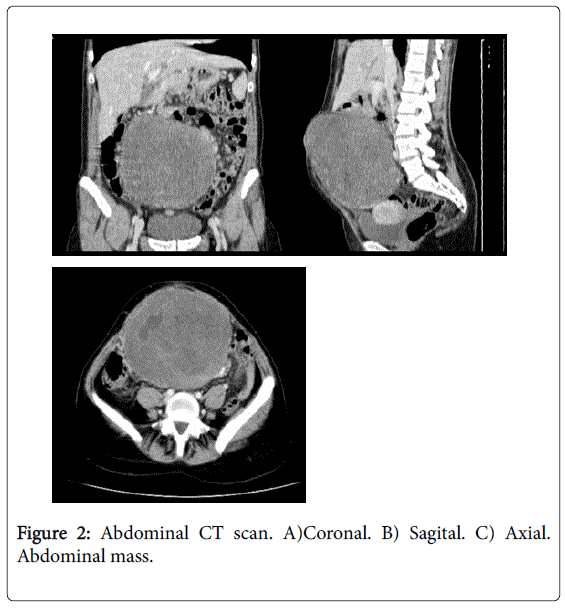
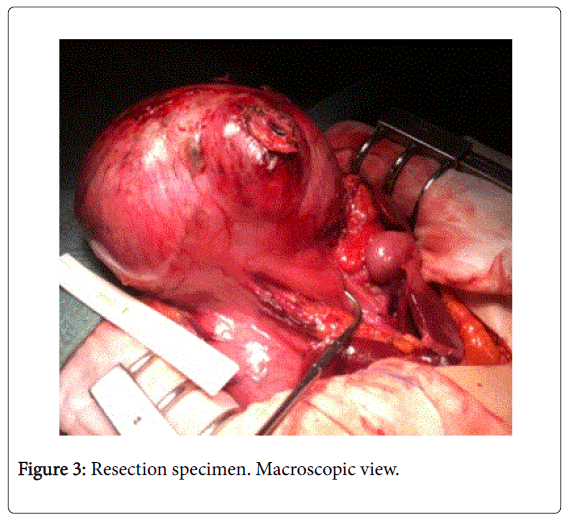
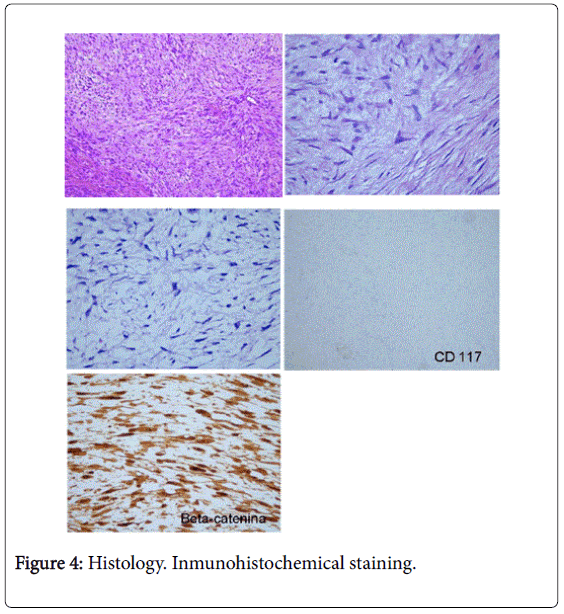
Our patient was a 37 years old healthy woman, with not known allergies and a normal delivery in the previous 9 months. The patient is admitted in the Emergency Room of our institution presenting an abdominal mass that has fast and progressively growed for the last 3 months. For two days before her consultation the patient refers dizziness, vomiting and diffuse abdominal pain. The pain is increased with movements, specially when standing up. Physical examination revels a soft and depressible abdomen, slightly painful during palpation. A big, round, hard and mobile mass is identified in the mesogastric region, extended to the pelvis (Figure 1). Blood tests are normal, except for a CRP of 15 U/l. Abdominal ultrasound shows a 15 cm mass. The mass is mainly solid, with some cystic regions inside it. An abdominal CT- Scan confirms the presence of a great tumor, with hypodense areas, correlated with necrostic areas. It is impossible to determine the existence of a free separation layer between the tumor and the gastric antrum. Due to these findings the lesion is considered to be dependant of the gastric submucose (Figure 2). The CT- Scan also reveals a significant peritumoral circulation, with tortuous blood vessels of considerable diameter. The subsequent gastroscopy showed a compression area in the gastric antrum, but preserved mucosa. With all these diagnostic tests and due to the lack of histological diagnosis, a surgical approach is decided for what was considered a Gastro- Intestinal Stromal Tumor (GIST) of gastric antrum. A regular laparotomy was performed to reach the abdominal cavity. Once the peritoneum is opened, a great tumor surrounded by great omentum is observed, with remarkable vascularization originated in the gastric antrum. The rest of the abdominal cavity does not present pathological findings. A distal gastrectomy with Billroth I (Pean variant) reconstruction is carried out (Figure 3). In the immediate postoperative period the patient refers cephalalgia associated with horizontal binocular diplopia, predominantly on the right eye. Having been evaluated by the Ophthalmology and Neurology Services she is diagnosed of cephalalgia due to hypotension of the cerebrospinal fluid with secondary damage of the VI cranial nerve due to distension. Evolution with medical treatment is satisfactory and the patient recovers from symptoms without sequela. From a surgical point of view the evolution was favorable and the patient was discharged after restablishment of oral tolerance, recovery of bowel function and control of all symptoms, on the eighth day. The histological macroscopic analysis reported a well defined mass, originated in muscular layer of the gastric antrum, with bright grey-yellow cut surface, and some cavitated hemorrhagic areas. It has 19 x 15 cm diameters, and weighs 2.900 kg. In the microscopic analysis, no defined architectural pattern was identified. Heterogeneous miofibroblastic proliferation was assessed. Nine regional lymph nodes were isolated, with no nodal metastases. 5-10 mitoses per HPF were identified. Free tumor margins were reported. Inmunohistochemical staining (IHC) reported was as follows: Negative expression for CD117, CD34, S100, DOG1, Actin, bcl-2. Positive expression for Betacatenin in both nucleus and cytoplasm (Figure 4). No mutations of ckit/ PDGFRA found. After 4-year follow-up, the patient runderwent a regular cholecystectomy for lithiasic disease, but remains without symptoms and no recurrence has been identified so far.
Conclusion
We present a case of a gastric desmoid tumor. Gastric location for desmoid tumors have never been described up to date. A remarkable aspect is the low experience surgeons have when facing this disease due to its low incidence. This point arises the importance of reminding the differential diagnosis when dealing with an abdominal oligosymptomatic mass, context in which the difference between desmoids and other entities such as GIST becomes crucial. It is also important to remind that because of their relation, all patients diagnosed of a desmoid tumor, must have their colon systematically explored in search of FAP; and on the other hand, any abdominal mass in a patient diagnosed of FAP should arise the suspicion of a desmoid tumor.
References
- Shields CJ, Winter DC, Kirwan WO, Redmond HP (2001) Desmoid tumours. Eur J SurgOncol 27: 701-706.
- Sutton RJ, Thomas JM (1999)Desmoid tumours of the anterior abdominal wall. Eur J SurgOncol 25:398-400.
- Lewis JJ, Boland PJ, Leung DH, Woodruff JM, Brennan MF (1999) The enigma of desmoidtumors. Ann Surg 229: 866-872.
- Kulaylat MN, Karakousis CP, Keaney CM, McCorvey D, Bem J, et al. (1999) Desmoid tumour: a pleomorphic lesion. Eur J SurgOncol 25: 487-497.
- Dalén BP, Bergh PM, Gunterberg BU (2003) Desmoidtumors: a clinical review of 30 patients with more than 20 years' follow-up. ActaOrthopScand 74: 455-459.
- Mendenhall WM, Zlotecki RA, Morris CG, Hochwald SN, Scarborough MT (2005) Aggressive fibromatosis. Am J ClinOncol 28: 211-215.
- Phillips SR, A'Hern R, Thomas JM (2004) Aggressive fibromatosis of the abdominal wall, limbs and limb girdles. Br J Surg 91: 1624-1629.
- Gurbuz AK, Giardiello FM, Petersen GM, Krush AJ, Offerhaus GJ, et al. (1994) Desmoid tumours in familial adenomatous polyposis. Gut 35: 377-381.
- Vasen HF, Möslein G, Alonso A, Bernstein I, Bertario L, et al. (2007) Guidelines for the clinical management of Lynch syndrome (hereditary non-polyposis cancer). J Med Genet 44: 353-362.
- Ishizuka M, Hatori M, Dohi O, Suzuki T, Miki Y, et al. (2006) Expression profiles of sex steroid receptors in desmoidtumors. Tohoku J Exp Med 210: 189-198.
- Okuno S (2006) The enigma of desmoidtumors. Curr Treat Options Oncol 7: 438-443.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 17579
- [From(publication date):
October-2015 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 13023
- PDF downloads : 4556