Gastric Band Slippage: A Bariatric Surgery Emergency A Case Report
Received: 24-Jun-2022 / Manuscript No. JOWT-22-67580 / Editor assigned: 25-Jun-2022 / PreQC No. JOWT-22-67580(PQ) / Reviewed: 09-Jul-2022 / QC No. JOWT-22-67580 / Revised: 14-Jul-2022 / Manuscript No. JOWT-22-67580(R) / Published Date: 21-Jul-2022 DOI: 10.4172/2165-7904.1000502
Abstract
A gastric band is a safe, dependable, and minimally invasive bariatric procedure that requires few tools and only minor dissection. In spite of this, complications can still occur. For instance, gastric band slippage, which occurs due to misplacement of the band, can lead to gastric obstruction. It is crucial to understand this complication before it develops into an unwanted adverse complication, which can be done through patients’ history, clinical examination, and imaging and managed immediately.
Keywords
Gastric band; Laparoscopic gastric band; Gastric obstruction; Gastric band slippage
Introduction
Obesity is becoming a worldwide pandemic [1] that is contributing to numerous medical comorbidities leading to death, such as diabetes mellitus, heart diseases, stroke, and cancer [2]. There are a wide range of methods for treating morbid obesity, including change of lifestyle and medications. However, surgery is the only robust option for managing morbid obesity [3]. A laparoscopic adjustable gastric band (LAGB) is a standard, minimally invasive bariatric procedure that leads to safe and effective weight loss of up to 40% of initial excess weight [4]. Gastric band slippage is a late complication of LAGB reported in 4–13% of cases [5]. Here we are reporting on a 51-year-old female who presented with a gastric band slip after two years of LAGB insertion.
Case Report
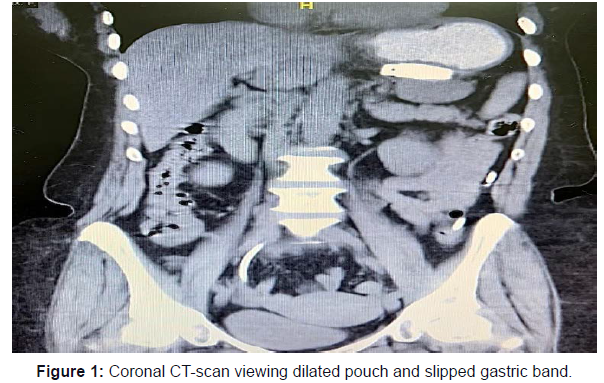
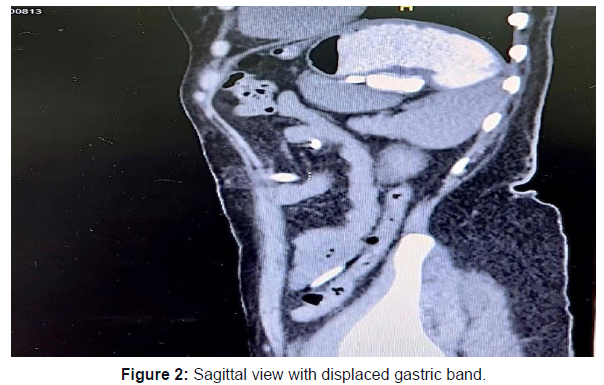
A 51-year-old female was admitted to the emergency department complaining of abdominal and chest pain associated with repeat vomiting, nausea, and loss of appetite for four days. The patient has a background history of laparoscopic gastric band insertion two years ago with considerable weight loss. The band was not inflated for one year and in her last visit – approximately three months ago – it was deflated. She was vitally stable with unremarkable physical and laboratory findings. The patient was transferred to the radiology department for a CT scan with oral and intravenous contrast, which showed complete gastric obstruction with a displacement of the gastric band to the mid-body and a markedly dilated stomach pouch with no contrast entering the distal body, a balloon within the band that is still dilated (Figures 1 and 2), and no evidence of ischemia. A trial of band aspiration was commenced; however, no change in patient status or relief of symptoms were recorded. The surgical team was consulted regarding the surgical removal of the band laparoscopically.
Intra-operative
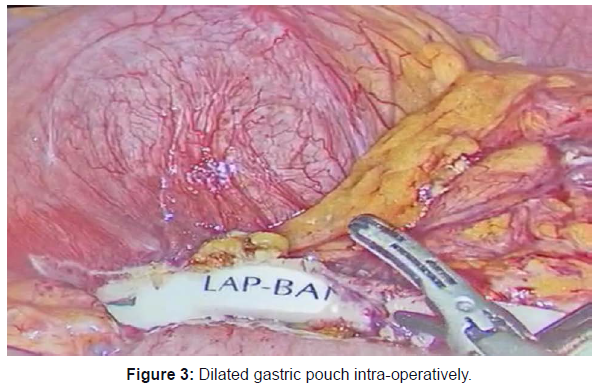
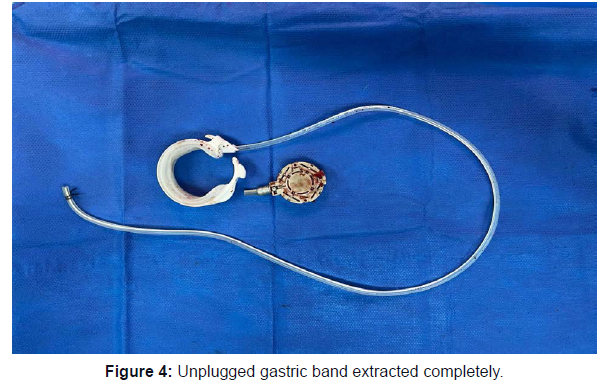
Four ports were used, and a markedly dilated gastric fundus was seen with the band at the mid-stomach with no sign of ischemia (Figure 3). The band was dissected from the capsule and adhesions via the ultrasonic device and mono-polar diathermy. It was successfully unplugged and retrieved fully outside the abdominal cavity (Figure 4). However, the capsule created severe adhesion obstructing the passage of the boogie. Thus, further dissection was performed in order to remove the capsule, which helped to clear the stomach’s pathway. Post-operative
The patient's post-operative recovery was uneventful. She was discharged after resuming a regular diet. Only three doses of antibiotics were required during her hospital course. The first outpatient visit took place after 14 days. The patient raised no complaints and her wounds were clean.
Discussion
Bariatric surgery is the acceptable, sustainable weight loss method used for obese patients worldwide [6]. It entails various procedures that can be restrictive, malabsorptive, or a combination of both, and which are performed according to the surgeon’s preferences and the patient’s condition. An LAGB has many advantages for the surgeon: it requires fewer tools, has low surgical morbidity, leads to rapid recovery, has high adjustability and reversibility, and produces acceptable outcomes [7]. According to the American Society for Metabolic and Bariatric Surgery (ASMBS), in 2011, LAGB accounted for 35.4% of all bariatric cases [8]. The first LAGB was described in 1993 by Belachew [9]. There are two LAGB techniques – the peri-gastric technique and the para flaccida technique – with many surgeons preferring the para flaccida technique [10].
Numerous complications of LAGB have been described in the literature. Some are minor such as pouch dilation (12%), gastrooesophageal reflux disease (7%), port prominence (2–6%), and port malfunction, while others are major, such as band erosions (<1%), slippage (5%), port infection, and gastric obstruction [11]. As mentioned earlier in this case, the patient experienced herniation of the band to the distal stomach, which is among the expected significant complications of LAGB. Common symptoms are abdominal pain, nausea, vomiting, food intolerance, regurgitation, nocturnal vomiting, and severe dyspepsia. Patients sometimes present with severe chest pain upon ingesting solid or liquid food [12]. Diagnosis (GBS) can be achieved via patient medical history, AP abdominal X-ray studies, or computer tomography scan (CTscan), which reveals dilatation of the pouch and improper position of the gastric band [13]. There are five types of gastric band slippage: anterior slip (type 1 prolapse), posterior slip (type 2 prolapse), pouch enlargement (type 3 prolapse), immediate post-operative prolapse (type 4 prolapse), and finally anterior and posterior slip with gastric perforation (type 5 prolapse) [14]. Recognition of GBS requires urgent intervention through deflation of the band for symptoms relief and subsequent laparoscopic band removal or adjustment to prevent adverse complications such as stomach ischemia, necrosis, and subsequent perforation, which, according to the literature, have a 5–11% chance of occurring [14-16].
Conclusion
Gastric band slippage is considered a significant complication in laparoscopic gastric band surgery. Although it is not particularly common, reporting it remains crucial as identifying presentations and image findings can help to prevent unwanted complications in the future.
References
- DeMaria EJ (2007) Bariatric surgery for morbid obesity. N Engl J Med. 356: 2176-83.
- Hales CM, Carroll MD, Fryar CD, Ogden CL (2017) Prevalence of Obesity Among Adults and Youth: United States, 2015-2016. NCHS Data Brief. 288: 1-8.
- Flum DR, Belle SH, King WC, Wahed AS, Berk P, et al. (2009) Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 361: 445-54.
- Himpens J, Cadière GB, Bazi M, Vouche M, Cadière B, et al. (2011) Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg. 146: 802-807.
- Mortelé KJ, Pattijn P, Mollet P, Berrevoet F, Hesse U, et al. (2001) The Swedish laparoscopic adjustable gastric banding for morbid obesity: radiologic findings in 218 patients. AJR Am J Roentgenol 177: 77-84.
- Fobi MAL (2004) Surgical treatment of obesity: a review. J Natl Med Assoc 96: 61-75.
- Hady HR, Dadan J, Sołdatow M, Ładny RJ, Gołaszewski P, et al. (2012) Complications after laparoscopic gastric banding in own material. Wideochir Inne Tech Maloinwazyjne. 7: 166-174.
- Herndon LK, Stead TG, Ganti L, Jasper T, Lebowitz D (2019) Laparoscopic Adjustable Gastric Band Slippage Presenting as Chest Pain. Cureus. 11: e5069.
- Banlı O, Altun H, Aslan E, Sipahi M, Börekçi H, et al. (2014) Laparoscopic adjustable gastric banding: technique and results. Laparoscopic Endoscopic Surgical Science (LESS). 23: 78-82.
- Coco D, Leanza S (2021) Slippage of Gastric Banding for Mobid Obesity: Case Report and Review of Literature: Slippage of Gastric Banding. BJOS. 1(1).
- Eid I, Birch DW, Sharma AM, Sherman V, Karmali S (2011) Complications associated with adjustable gastric banding for morbid obesity: a surgeon's guides. Can J Surg. 54: 61-66.
- Keidar A, Szold A, Carmon E, Blanc A, Abu-Abeid S (2005) Band slippage after laparoscopic adjustable gastric banding: etiology and treatment. Surg Endosc. 19: 262-267.
- Blachar A, Blank A, Gavert N, Metzer U, Fluser G, et al. (2007) Laparoscopic adjustable gastric banding surgery for morbid obesity: imaging of normal anatomic features and postoperative gastrointestinal complications. AJR Am J Roentgenol. 188: 472-479.
- Kang SH, Kim KC, Kim KH (2014) Endoscopic treatment of gastric band prolapse. Obes Surg. 24(6): 954-957.
- Snow JM, Severson PA (2011) Complications of adjustable gastric banding. Surg Clin North Am. 91(6): 1249-ix.
- Lee WK, Kim SM (2014) Three-year experience of pouch dilatation and slippage management after laparoscopic adjustable gastric banding. Yonsei Med J. 55(1): 149-156. doi:10.3349/ymj.2014.55.1.149
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Al-Mulla AE, Sultan AE, Imam ES, Al-Juwaihel HJ, Elnemr M (2022) Gastric Band Slippage: A Bariatric Surgery Emergency A Case Report. J Obes Weight Loss Ther 12: 502. DOI: 10.4172/2165-7904.1000502
Copyright: © 2022 Al-Mulla AE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2509
- [From(publication date): 0-2022 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 2073
- PDF downloads: 436