Case Report Open Access
Gall Bladder Perforation Leads to Liver Abscess Formation – Role of Ultrasonography
Rikki Singal1*, Samita Gupta3, Rajinder Pal Singal2, Amit Mittal3, Saurabh Sharma1 and Raviv Khurana1
1Department of Surgery, Maharishi Markandeshwer Institute of Medical Sciences and Research, Mullana (Dist-Ambala), Haryana, India
2Department of Orthopaedics, Adesh Institute of Medical Sciences and Research, Bathinda, India
3Department of Radiodiagnosis and Imaging, Maharishi Markandeshwer Institute of Medical Sciences and Research, Mullana (Dist-Ambala), Haryana, India
- *Corresponding Author:
- Rikki Singal
Department of Surgery
Maharishi Markandeshwer Institute of Medical Sciences and Research
Mullana (Dist-Ambala), Haryana, India
Tel: 09996184795
Fax: 01731304550
E-mail: singalsurgery@yahoo.com
Received date: March 01, 2015; Accepted date: March 30, 2015; Published date: April 15, 2015
Citation: Singal R, Gupta S, Singal RP, Mittal A, Sharma S, et al. (2015) Gall Bladder Perforation Leads to Liver Abscess Formation – Role of Ultrasonography . J Gastrointest Dig Syst 5:279. doi:10.4172/2161-069X.1000279
Copyright: © 2015 Singal R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Perforation of the gall bladder is a rare complication of cholecystitis leads to liver abscess. Hepatic abscess is reportedly associated with a 7% to 40% prevalence of biliary communication. Biliary communication may prevent an abscess from healing after percutaneous drainage and, if so, require additional surgical or other interventional treatment. We report a case of a 40 year – old female who was diagnosed as gallbladder perforation and intrahepatic abscess which was successfully treated by surgically.
Keywords
Ultrasonography; Acute cholecystitis; Perforation; Peritonitis; Surgery
Introduction
Perforation of the gallbladder with cholecystohepatic communication is a rarer cause of liver abscess [1,2]. In 1934, a classification was proposed by Neimeir of acute perforation of the gall bladder based on his findings and how to treat it [3,4]. He concluded that this rare condition requires early recognition and treatment to decrease the mortality.
There are no classical symptoms and signs associated with gall bladder perforations. Only a few adult cases have been reported in the English literature [5,6]. Ultrasonography (USG) can be useful in detecting gall bladder perforation preoperatively.
Case Report
A 40 year-old female presented with history of acute pain in the abdomen with episodes of vomiting since two days in emergency. Fever was also present. Pain was more in right hypochondrium region. Patients pulse rate was 120/min, blood pressure-120/70 mmHg and was febrile.
On abdominal examination, generalized tenderness was present but tenderness was more in the right upper quadrant region. On palpation, temperature was raised. Rigidity was present in right upper abdomen but no mass was felt. On laboratory findings, white cell counts were raised. Rest of blood tests was within normal limits including liver function tests. Chest X-ray revealed no gas under diaphragm.
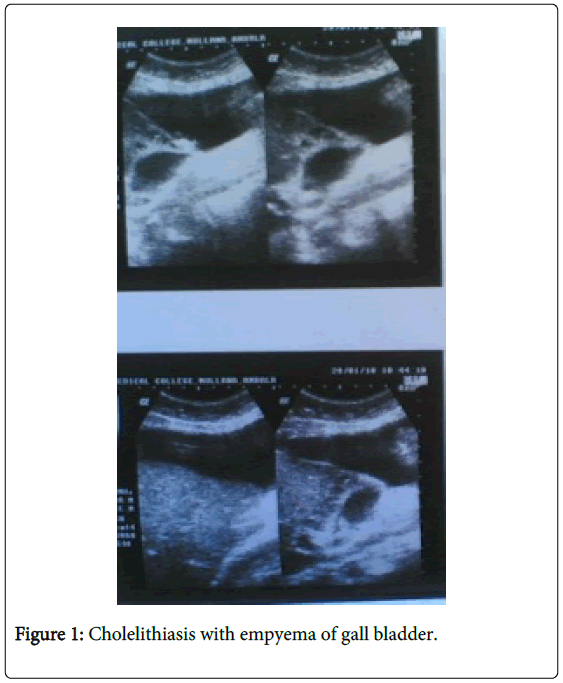
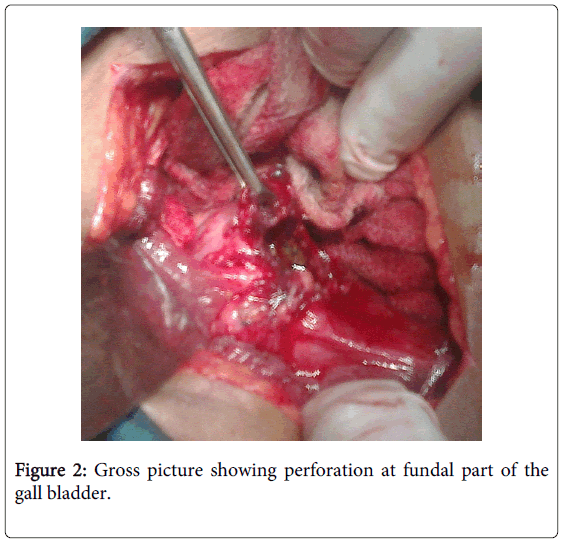
Ultrasonography of the abdomen revealed distended gall bladder with thickened wall (5 mm) and thick internal echoes with a large 1.2 cm calculus in the neck of gall bladder suggestive of cholelithiasis with empyema of gall bladder (Figures 1 and 2).
There was large 2 cm defect in the left anterior wall of gall bladder with formation of large abscess in adjacent liver. On USG diagnosis was made as perforation of gall bladder empyema with formation of liver abscess.
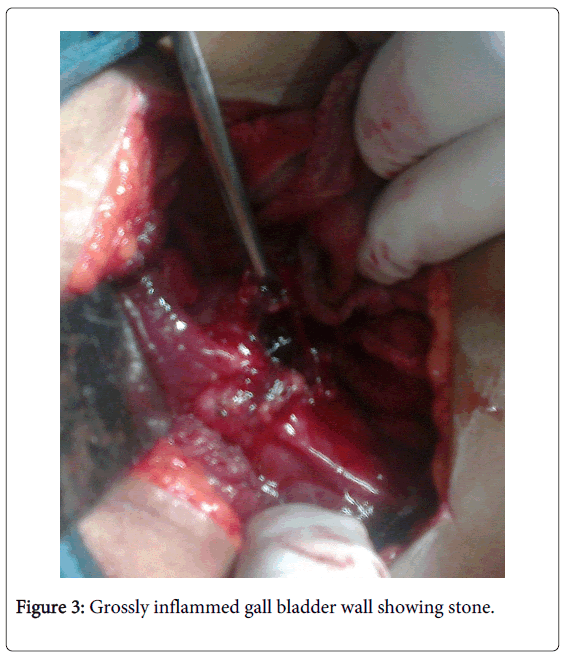
Patient was taken for surgery finding revealed gallbladder perforation at fundus part with formation of liver abscess (Figure 3). A single large stone of size approximately 1.5 cm in fundus part of the gall bladder neck and common bile duct was dilated. Adhesions were present to surrounding structures and bile was present in the peritoneal cavity. Cholecystectomy was done with thoroughly wash of the whole abdomen by normal saline. In follow up of 6 months, patient is doing well.
Discussion
Perforation of the gall bladder is an infrequent and serious complication of cholecystitis. The incidence of this complication has shown a decline over time since its first description by Duncan in 1884 [7]. Rates of gall bladder perforation are decreased due to an increase in the number of cholecystectomies performed as compared with the past. A recent case series found the rate of perforation to be 0.8% [8]. In 1934, Niemeier classified GBF into three types: type chronic perforation with the presence of a fistulous communication between the gall bladder and some other viscus; type subacute perforation where the perforated gall bladder is surrounded by an abscess walled off by adhesions from the general peritoneal cavity; and type 3, acute perforation of the gall bladder into the free peritoneal cavity without protective adhesions [9].
Gall bladder perforation can be due to cholelithiasis, infection, malignancy, trauma, corticosteroid therapy, diabetes mellitus, impaired vascular supply, old age and male sex. Patients may present with right upper quadrant pain, fever, palpable right upper quadrant mass and tenderness may herald an acute onset. But in malignancy, patients may present with weakness, malaise, anorexia and a palpable right upper quadrant mass [1]. Elevated liver enzymes, especially alkaline phosphatase levels are commonly observed [3]. A sudden decrease in pain intensity may occur due to perforation which causes relief of high intracholecystic pressure [3].
Somasekhar et al. [5] reported 31 patients with GBF. Nine patients (29%) had type I perforation, presented with complaints of generalized abdominal pain. Seven patients had history of pain, which was initially localized to the right hypochondrium before becoming generalized. Three of these were already diagnosed to have gallstone disease and were waiting for elective cholecystectomy. Seven (78%) patients had presented with shock. Features of generalized peritonitis were seen in six (67%) patients. Type II perforation was present in 14 patients (45%) who presented with complaints of right hypochondrial pain, which ranged in duration from 3 days to 15 days. All except for one patient described a history of such complaints even though they may have been milder. Type III perforation was present in eight patients (26%) and presented with acute cholecystitis. However, these patients had symptoms of longer duration and were recurrent. Fever was noted in 15 (48%) patients, all of whom had either type I or type II perforations. An abdominal mass was present in 11 patients (36%) while three (10%) patients have presented with jaundice. Zerman [10] reported 5 cases of hepatic abscess secondary to acute cholecystitis (4 males and 1 female), aged between 46 and 78 years. They presented with fever, abdominal pain and, one, with jaundice. Liver abscess were diagnosed by USG and CT scan. In acute phase, all the patients were treated with percutaneous drainage and subsequently, four of them had elective cholecystectomy. CT may have an important role in preoperative diagnosis of complicated acute cholecystitis and in the surgical management of patients with this condition, if ultrasound examination fails to establish the diagnosis or cannot be done for technical reasons [11].
In the past, clinical and radiological aids were insufficient to clinch the diagnosis, however advent of CT and MRI has made it easier [12]. Though ultrasound could not specifically identify type I perforations, it was helpful in determining the need for surgical intervention, as it could identify the presence of free fluid, the appearance of which, on guided tap, left no doubts about the pathology. The results of ultrasound in our patients are similar to those quoted in various studies comparing efficacy of ultrasound in detecting gall bladder perforation [13-15]. Ultrasonography (USG) and CECT are the most important tools in diagnosing this rare complication. USG is the initial investigation of choice in evaluating acute gallbladder pathology and is often sufficient for a correct diagnosis. CECT is particularly useful in situations where ultrasound findings are not confirmatory. CECT is also valuable in the assessment of emphysematous cholecystitis, and gallbladder perforation [16].
The treatment modality has not been fully established for gallbladder perforation with cholecystohepatic communication leads to liver abscesses which is rare [1-3]. USG may show gall bladder wall thickening >3 mm, gall bladder distention(largest diameter >3.5-4.0 cm),gallstones, coarse intracholecystic echogenic debris and bile duct dilatation including ‘halo sign’ which can help in diagnosis, as diagnosed in our case [17,18]. The earliest signs of impending gall bladder perforation detectable on sonography may be distended gallbladder and oedema of its walls alongwith liver abscess raise the suspicion of intrahepatic perforation [19]. Computed Tomography can demonstration of either calculi outside the gall bladder or a ruptured segment of the gall bladder wall which are the direct indicators of perforation according to Pedrosa et al. [11]. The demonstration of an abscess outside the gall bladder, presence of gallstones and thickening of gall bladder wall are the indirect indicators. As in our reported case we also diagnosed a ‘hole sign’ between the gall bladder and the liver abscess which matched to other reported studies [11]. Roslyn and Busutte [20] have reported mortality rate to be between 12 and 16%. They have suggested that spontaneous gall bladder perforation is caused by hypoperfusion of viscera, secondary to systemic disease and also reported that the fundus of the gall bladder is the most common site of perforation in gall bladder. However, other hypotheses include trauma, congenital abnormality, infection, pancreatic secretions, obstructions, calculi and abnormal bile [21]. Delay in surgical intervention is the major reason for increased morbidity and mortality associated with GBF. Emergency cholecystectomy should be considered in patients with acute cholecystitis at an early stage to prevent this complication [9].It is others opinion that an open approach or early conversion should, in these cases, as in other Niemeier’s perforation type I, still be the preferred surgical treatment [22].
Conclusion
We present a rare case of gall bladder perforation leads to formation of hepatic abscess with cholecystohepatic communication. Initially, such cases can be treated conservatively with percutaneous drainage with subsequent cholecystectomy. The intrahepatic nature of the gall bladder in such cases can lead to difficulty in laparoscopic cholecystectomy with a high rate of conversion to open cholecystectomy. Even if percutaneous drainage tried then again chances of remaining ruptured gall bladder can lead to septicaemia. So to prevent futher complications, laparoscopic or open surgery should be done unless patient unfit for surgery.
References
- Bakalakos EA, Melvin WS, Kirkpatrick R (1996) Liver abscess secondary to intrahepatic perforation of the gallbladder, presenting as a liver mass.Am J Gastroenterol 91: 1644-1646.
- Peer A, Witz E, Manor H, Strauss S (1995) Intrahepatic abscess due to gallbladder perforation.Abdom Imaging 20: 452-455.
- Morris BS, Balpande PR, Morani AC, Chaudhary RK, Maheshwari M, et al. (2007) The CT appearances of gallbladder perforation.Br J Radiol 80: 898-901.
- Huang CC, Lo HC, Tzeng YM, Huang HH, Chen JD, et al. (2007) Percutaneous transhepatic gall bladder drainage: a better initial therapeutic choice for patients with gall bladder perforation in the emergency department. Emerg Med J 24: 836-840.
- Menakuru SR, Kaman L, Behera A, Singh R, Katariya RN (2004) Current management of gall bladder perforations.ANZ J Surg 74: 843-846.
- Kochar K, Vallance K, Mathew G, Jadhav V (2008) Intrahepatic perforation of the gall bladder presenting as liver abscess: case report, review of literature and Niemeier's classification.Eur J GastroenterolHepatol 20: 240-244.
- Duncan J (1844-1845) Femoral hernia, Gangrene of the gallbladder: Extravasation of bile: Peritonitis: Death. North J Med 2: 151-153.
- Stefanidis D, Sirinek KR, Bingener J (2006) Gallbladder perforation: risk factors and outcome.J Surg Res 131: 204-208.
- Singal R, Mittal A, Gupta S, Singh B, Jain P (2011) Management of gall bladder perforation evaluation on ultrasonography: report of six rare cases with review of literature.J Med Life 4: 364-371.
- Aljiffry M, Walsh M, Peltekian K, Molinari M (2008) Type II gall bladder perforation with abdominal wall abscess in a cirrhotic patient: case report and review of the literature.J SurgEduc 65: 367-371.
- Pedrosa CS, Casanova R, Rodríguez R (1981) CT findings in subacute perforation of the gallbladder: report on 5 cases.Eur J Radiol 1: 137-142.
- Ji JS, Zhang SZ, Shao CX, Zhao ZW, Wang ZF, et al. (2007) Imaging diagnosis of two unusual forms of gallstone ileus.Chin Med J (Engl) 120: 938-940.
- Lobo DN, Jobling JC, Balfour TW (2000) Gallstone ileus: diagnostic pitfalls and therapeutic successes.J ClinGastroenterol 30: 72-76.
- Atli AO, Coşkun T, Ozenç A, Hersek E (1997) Biliary enteric fistulas.IntSurg 82: 280-283.
- Sood BP, Kalra N, Gupta S, Sidhu R, Gulati M, et al. (2002) Role of sonography in the diagnosis of gallbladder perforation.J Clin Ultrasound 30: 270-274.
- Narayanan S, Rammohan A, Sathyanesan J, Palaniappan R, Govindan M (2015) Gallbladder perforation presenting as a hepatic neoplasm. Arch ClinExpSurg 4.
- Goldberg BB (1977) Abdominal gray scale ultrasonography. John Wiley; New York.
- Chau WK, Na AT, Feng TT, Li YB (1988) Ultrasound diagnosis of perforation of the gallbladder: real-time application and the demonstration of a new sonographic sign.J Clin Ultrasound 16: 358-360.
- Madrazo BL, Francis I, Hricak H, Sandler MA, Hudak S, et al. (1982) Sonographic findings in perforation of the gallbladder.AJR Am J Roentgenol 139: 491-496.
- Roslyn J, Busuttil RW (1979) Perforation of the gallbladder: a frequently mismanaged condition.Am J Surg 137: 307-312.
- Croley GG 2nd1 (1992) Gangrenous cholecystitis: five patients with intestinal obstruction.Am Surg 58: 284-292.
- Donati M, Biondi A, Basile F, Gruttadauria S (2014) An atypical presentation of intrahepatic perforated cholecystitis: a modern indication to open cholecystectomy. Report of a case.BMC Surg 14: 6.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 19983
- [From(publication date):
June-2015 - Jul 06, 2025] - Breakdown by view type
- HTML page views : 15327
- PDF downloads : 4656