Full-Endoscopic Interlaminar Versus Microsurgical Operations in Lumbar Compressive Lesions Surgery: Prospective Randomized Trial of Overall 570 Patients
Received: 07-Oct-2017 / Accepted Date: 22-Nov-2017 / Published Date: 27-Nov-2017 DOI: 10.4172/2167-0846.1000304
Abstract
Introduction: Full-endoscopic operations of lumbar spine are truly minimally invasive surgical procedures and they have become the standard because of their intraoperative and postoperative advantages.
Aim: To compare clinical outcomes of full-endoscopic interlaminar technique to conventional microdiscectomy performed during 3 year period.
Materials and Methods: A series of 350 patients underwent full-endoscopic interlaminar lumbar discectomy, comparing 220 patients with microdiscectomy and spinal canal decompression, during a 3-year period, is analysed. Oswestry Disability Index (ODI), visual analogue scores (VAS) of back and leg pain were measured preoperatively and at 1, 6, 12, 24 months.
Results: All outcome measures improved significantly in both groups (p<0.001). In the full-endoscopic group 88% of the patients no longer had leg pain, and 7% had only occasional pain, postoperatively. In the microdiscectomy (MI) group 78.1% had significant improvement, 13.6% had improvement with occasional pain, and 8% had no improvement. The recurrence rate was 8%. Resection of the herniated disc and sufficient decompression was technically possible in all cases. The overall complication rate (16.4%), and recurrence-reoperation rate (11.8%) was significantly higher in the MI group.
Conclusion: The clinical results of the full-endoscopic technique are at least equal to those of the conventional microsurgical discectomy with advantages such as reduced traumatization, improved patient mobility, and lower complication and recurrence rate. With the possibility of selecting the most adequate approach, lumbar disc herniations inside and outside the spinal canal, can be sufficiently removed using the full-endoscopic technique, when taking the appropriate indication criteria into account.
Keywords: Full-endoscopic discectomy; Interlaminar decompression; Microdiscectomy; Monosegmental stenosis
Introduction
Mixter and Barr [1] reported an open hemilaminectomy with intraoperative discotomy for treatment of intervertebral disc rupture into the spinal canal. The results of intrathecal endoscopy of more than 400 myeloscopic procedures were presented in 1942 by Pool [2]. Ooi and colleagues [3] used an endoscope to examine the intrathecal space before surgery and they were able to describe pathologic features in nerve elements in spinal canal. Microendoscopic discectomy (MED) through tubular retraction was first reported by Foley and Smith [4]. MED combines standard microsurgical technique with endoscopy, enabling surgeons to access disc herniations. The first use of a laparoscopic approach to the lumbar spine for a discectomy was reported by Obenchain [5]. Good results have been associated with microdiscectomy, but postoperative complications like scarring of the epidural space and destabilization of the spinal column structures may occur [6-8]. The full-endoscopic (FE) technique provides minimal skin incision and much less tissue damage compared with standard open microdiscectomy with reduced hospital stays and costs. The most used approaches in the full-endoscopic lumbar surgery is transforaminal (TF) and interlaminar (IL) approach [8-11]. The FE IL access has been developed to enable the extirpation of pathologic entities not successfully achieved using the TF technique [11-13]. The goal of this prospective study was to compare the results of lumbar full-endoscopic interlaminar discectomy with those of the standard microsurgical technique, performed during 3 year period with representative clinical series of patients.
Materials And Methods
The presented study is a prospective, randomized study which was done on 570 patients with lumbar disc herniation operated from 2012 to 2014. Before participants enter the study, it was essential to complete the informed consent. Then the patients had neurosurgical examination, and after the MRI verification of disc herniation they have been introduced for surgery. Before surgery the permission was taken, and then the patients entered the study. The study was approved by Ethical committee of Clinical Hospital Center-Zemun.
Three hundred and fifty (350) patients underwent full-endoscopic interlaminar operation and 220 patients were operated by conventional microsurgical technique.
There were 337 male and 233 female patients. The mean age was about 40 years old. All patients presented with clinicaly symptomatic disc herniation with significant radicular symptoms (mean Lasegue sign in microdiscectomy (MI) group 42 degrees and in full-endoscopic (FE) group 40 degrees).
The indication for operation was defined through today’s standards based on existing radicular symptoms with or without neurological deficit. Twenty one operations were performed at the level of L3/4, 174 on L4/5 and 375 on L5/S1 disc level (Table 1). All patients were operated in general endotracheal anesthesia.
| Variable | Statistics | MI, n=220 | FE, n=350 | |
|---|---|---|---|---|
| Age | mean ± SD | 40.32 ± 10.54 | 40.55 ± 10.18 | |
| Gender | Male Female |
Freq; % | 118; 53.6 102; 46.4 |
219; 62.6 131; 37.4 |
| Type of DH | Protrusion Extrusion Sequestration |
Freq; % | 25; 11.4 156; 70.9 39; 17.7 |
27; 7.7 275; 78.6 48; 13.7 |
| Lesion level | L3-L4 L4-L5 L5-S1 |
Freq; % | 18; 8.2 110; 50.0 92; 41.8 |
3; 0.9 64; 19.1 283; 81.0 |
| Lazarevic/Lasegue (degrees) | mean ± SD | 42.34 ± 16.25 | 40.06 ± 15.76 | |
| GMS<4 | Freq; % | 32; 14.5 | 27; 7.7 | |
Table 1: Descriptive variables for MI and FE IL group.
In this prospective study we generated reproducible randomization schedule and after obtaining, to each subject we assigned random number generated using SAS.
The study entrance criteria: (1) Lumbar disc herniation within the spinal canal in L3/4, L4/5 and L5/S1 level (including the sequestration of disc migrated cranially or caudally), with lumbar spine plain radiographs, and magnetic resonance imaging (MRI) corresponding to the clinical symptoms; (2) Age between 20 and 70 years; (3) failure of at least two weeks of conservative treatment
The excluding criteria from the study were: (1) lateral recess stenosis, extraforaminal disc herniations, and spinal instability; (2) an inability to accurately complete the pre- and post-operative questionnaires.
Clinical assessment
Clinical and demographic data were prospectively recorded. The patients completed a questionnaire consisting of a 10-point visual analog scale (VAS) for low back pain and radicular pain preoperatively and postoperatively. The patients also completed the Oswestry Disability Index (ODI) questionnaire for their quality of life preoperatively and postoperatively.
Follow up examinations was conducted 1, 6, 12, 24 months after surgery. The operation time, blood loss, hospital stay, return-to-work time, complication rate, failure rate, and reherniation rate were evaluated to assess the outcomes of the procedures.
Radiological assessment
All patients underwent MRI preoperatively, and if clinically needed after surgery. Disc degeneration was graded on MRI T2 spinecho weighted images using a grading system proposed by Pfirrmann [14]. This classification is not used on routine spine reports, being more important for research purposes (Table 2).
| Grade I | Disc is homogeneous with bright hyperintense white signal intensity and normal disc height |
| Grade II | Disc is inhomogeneous, but keeping the hyperintense white signal; nucleus and annulus are clearly differentiated and a horizontal gray band could be present; disc height is normal |
| Grade III | Disc is inhomogeneous with an intermittent gray signal intensity; distinction between nucleus and annulus is unclear; disc height is normal or slightly decreased |
| Grade IV | Disc is inhomogeneous with a hypointense dark gray signal intensity; there is no more distinction between the nucleus and annulus; disc height is slightly or moderately decreased |
| Grade V | Disc is inhomogeneous with a hypointense black signal intensity; there is no more distinction between the nucleus and annulus; thedisc space is collapsed |
Table 2: Grading system for disc degeneration proposed by Pfirmann.
Surgical procedures
All operations were performed under general endotracheal anesthesia in the prone position. In MI group we used the standard technique using a microscope with paramedian access. The level of lesion was identified with guidance of radiography or fluoroscopy in both groups. The FE IL operations were performed with 205 mm endoscope with the 4.2 mm working channel via interlaminarspace. Optical 25° angle system with continuos saline solution irrigation enabled excellent visualization, also good mobilization by handling endoscope with “joystick technique” (due to anatomy of the spinal canal) provides big comfort and efficient surgical work. The outer diameter of instruments of 3-4 mm was quite adequate for discectomy and sufficient decompression. If the interlaminar space was narrow we have performed widening of the canal with a burr symple or drill, as well as with kerison punch.
Statistics
Statistical analyses were performed using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA). The data were summarized by means, range, CI 95% and percents measure of variability used is SD. A Paired t-test, Mann-Whitney, chi-square and Wilcoxon test were used to determine difference between or within groups and Pearson or Spearman coefficient to determine correlation depending on type of variable.
Results
Demographics
We reviewed 350 patients in FE IL group and 220 patients in the MI group who met the inclusion and exclusion criteria. Patient demographics including the follow-up period were not significantly different between the two groups.
Clinical Outcomes
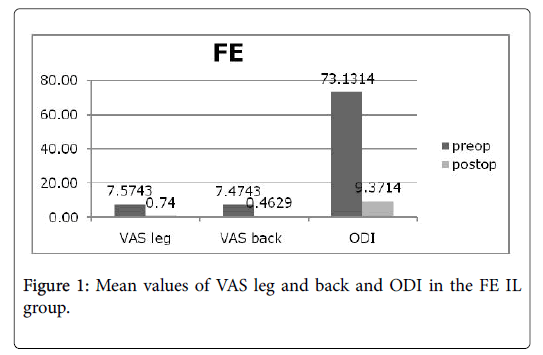
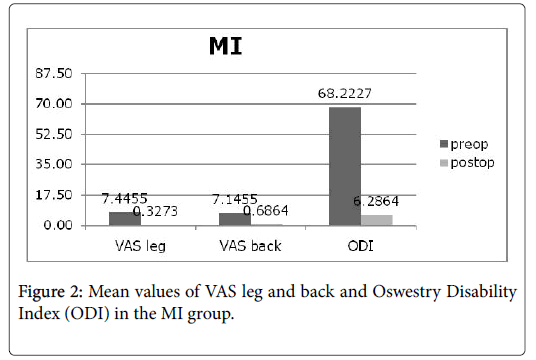
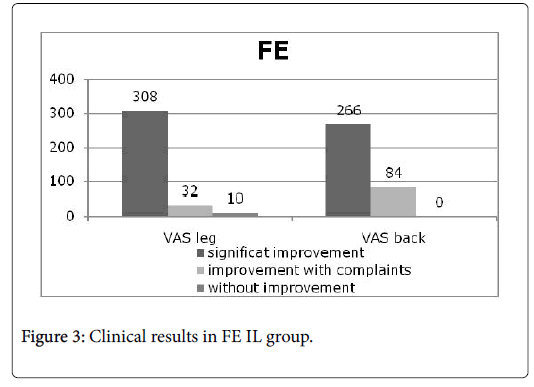
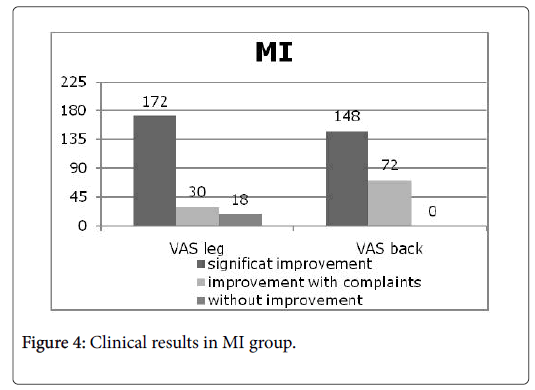
Preoperatively the back and leg VAS scores were 7.47 and 7.57 in FE IL group and 7.15 and 7.45 in MI group. These results revealed no significant differences. After surgery, the VAS scores for the back and leg decreased significantly in both groups. Postoperatively, the back and leg VAS scores were 0.46 and 0.74 respectively in FE IL group, and 0.69 and 0.33 in the MI group. However, there was no significant difference between the groups for VAS scores. The mean ODI scores significantly improved from baseline at the final follow-up in both groups (Figures 1 and 2). There were significant improvement in back and leg pain in all groups. After 3 years of follow up 308 patients (88%) in FE IL group, and 172 patients (78.1%) in MI group had significant improvement; 32 patients (7%) in FE IL group, and 30 (13.6%) patients in MI group had improvement with complaints (pain occasionally), and 18 patients (8%) in MI group and 10 patients (5%) in FE IL group had no improvement (Figures 3 and 4).
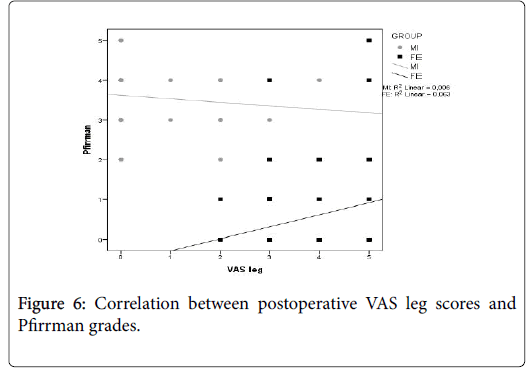
There is a significant difference noted among patients with different preoperative Pfirrman grades and postoperative VAS back and leg scores (p<0.001). Higher Pfirrmann degree was associated with higher postoperative VAS leg pain in MI and FE IL groups (p<0.001) and with postoperative VAS back pain in FE IL group (p<0.005) (Figures 5 and 6).
Postoperative complications
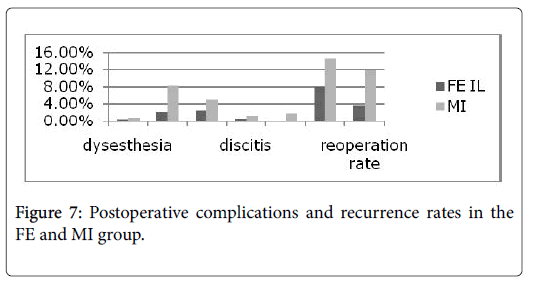
Four patients complained of dysesthesia on the posterolateral thigh, which spontaneously improved next month after surgery (two cases in group MI and two cases in group FE IL). A dural tear occurred in 8 patients (2.2%) in group FE IL (only one patient had reoperation for direct dural repair) andin 18 patients (8.2%) in group MI (of them 3 patients had reoperation). Nerve injury occurred in 9 (2.5%) patients in FE group, of them 7 patients had only parestesias and 2 patients had neurological deficit. In the MI group nerve injury occurred in 11 (5%), in 7 patients resulting in parestesias and 4 patients had neurological deficit. Discitis although rare complication was seen in 2 (0.6%) patients in FE group, and in 3 (1.4%) patients in MI group. There were no wound infection in the FE group, but in MI group was present in 4 (1.8%) patients. There were no serious complications like cauda equine syndrome or postoperative thrombosis in both groups (Figure 7). The overall complication rate was 6.5% in the FE IL group, and 16.4% in the MI group. The difference in overall complication rate between groups was significant (p<0.05).
Disc herniation recurrence rate
Recurrence rate up to 36 months of follow up period was 8% (28 patients) in FE IL group, and 14.5% (32 patients) in MI group. Only 13 (3.7%) patients in the FE group need reoperation, and 26 (11.8%) patients in the MI group with reherniation underwent reoperation. There was significant difference (p<0.05) in the recurrence rate between the groups.
Discussion
The main goal of surgical treatment of lumbar disc herniations is sufficient decompression with minimization of operation-induced trauma and its sequelae, which could be achieved with full-endoscopic operations.
The results of the FE IL procedure in our study is similar to those of the microsurgical (MI) procedure in a sense of VAS leg and back and ODI score improvement. These results are similar to previous reports [15-18] Clinical improvement also is similar in both groups but is better in FE IL group and is nearly 90% of excellent clinical outcome, which exceeds the good results of the microscopic-assisted procedures reported between 75 and 100% of the cases. These results are also corresponding to the other studies [15,18], but with less resection of spinal canal structures [18-25]. Operation time, tissue traumatization and complications are low compared to conventional procedures [26-34]. In our study, every single complication like dural tear with liquorea (2.2% FE/8.2% MI), nerve injury (2.5% FE/5% MI), discitis (0.6% FE/1.4% MI), and infection (0 FE/1.8% MI) were rare and less frequent in patients operated with full- endoscopic interlaminar technique. However, the overall complication rate was significantly lower in the patients operated with full-endoscopic technique.
It is our opinion, like in several other authors [35-37], that there is no operation-related worsening of existing symptoms in the FE group of patients, which is consistent with the minimally invasive epidural and intervertebral procedures. Also, concomitant diseases do not lead to increased morbidity [31,32,38,39].
In our study all 10 (5%) patients in the FE group without improvement had additional back pain and duration of symptoms more than 6 months, but the great majority of them (76%) had significant improvement in back pain despite the fact that radicular symptoms were predominant prior to surgery. Similar results in a sense of back pain improvement were present in the MI group (67.3%), and are in accordance with the several other reports from literature [27-45].
The rate of disc herniation recurrence was significantly lower in the FE group (8% vs. 14.5% in MI group), especially in the aspect of clinical need for reoperation (3.7% vs. 11.8%), in contrast to other studies [18,46,47]. The recurrence rate of 8% is slightly above some other reports of conventional techniques but still below selective sequestrotomies [40,41]. The rate of recurrence is reported variously in the literature and depending on anulus defect and fragment type ranges from 5% to over 20% [40-45]. On the other hand, our attempt was as complete resection as possible of available nucleus material in the intervertebral space, all in the purpose of lowering reherniation rate. In the several other studies [18,46,47] there was no difference in the recurrence rate between FE and MI group of patients but in our study significantly lower recurrence rate in the patients operated by FE IL technique is probably due to minimization of the operation-related anulus defect which was strict concept in our operative FE technique, what is already proposed as a protective biomechanical factor [45,48].
In the group of patients operated by FE IL technique in our study, postoperative MRI examinations (done if clinically needed) showed no scarring in the access area or in the epidural space. In repeated endoscopic operations this MRI finding is easily confirmed which, unlike following conventional techniques, were neither made more difficult nor required longer operation time as it is reported by several other authors [11,49]. However, epidural scarring which may become clinically symptomatic in up to 10% of cases, could be expected in conventional MI techniques [50-52]. Minimal traumatisation of the ligamentumflavum appears to bring advantages [53,54], because opening of the ligament to insert the endoscope into the spinal canal can be limited to a few mm (up to 5 mm). The combination of a lack of clinical symptoms, MRI and intraoperative revision findings obviously demonstrate reduced scarring due to minimal tissue traumatisation in the full-endoscopic procedures. In operation of lumbar disc recurrences, the risk of dural and nerve injury may increase owing to existing epidural scarring [55,56]. Increased epidural scarring may become clinically symptomatic [57,58], make revisions more difficult, and lead to “tethering” of the Cauda equine by postoperative connection between the epidural space and paravertebral musculature [59-61]. Also the route of access in the innervation area of the dorsal branch of the spinal nerves can have a negative influence on the stabilizing and coordination system [62,63]. For this reason, attempts are made even in the primary operation, and also in revisions, to work with tissue-sparing techniques [64,65] Furthermore, technical advances have been made in the primary operation of disc herniations which enable a full-endoscopic technique and provides the advantages of a truly minimally invasive procedure [64,66-68].
Pfirrmann developed a classification system for lumbar disc degeneration based on routine T2-weight MRI images and five grades of progressive degeneration. Briseno et al. [69] found that the degree of preoperative adjacent level degeneration does not significantly affect functional or pain relief outcomes following lumbar discectomy. Hong et al. [70] showed that adjacent segment degeneration and Pfirrmann grading for disk degeneration were significant risk factors for reoperation after primary microendoscopic diskectomy. Adjacent segment degeneration and Pfirrmann grading for disk degeneration were identified as risk factors for reoperation after microendoscopic discectomy to treat lumbar disk herniation. Corniola et al. [71] showed that patients with high Pfirrmann degrees of disc degeneration had more VAS back pain and a more reduced quality of life.
In our FE IL and MI group of patients, postoperative VAS leg pain was associated with higher Pfirrmann grades. Higher Pfirrmann grade was associated also with postoperative VAS back pain in the FE IL group. Our results suggest that higher Pfirrman grades seems potential indicators for unsatisfactory outcome (higher VAS scores), potential instability and need for dynamic stabilization procedures.
In the cases of relatively narrow interlaminar space (5-6 mm) we performed bony resection of the mediodorsal edge of processus articularis inferior by a few mm which was easily achieved using burr, so size of the interlaminar window between cranial and caudal lamina and midline and mediosagital border of the processus articularis inferior was not limitation factor. Occasional problems in mobility may arise because of the divergent level between the interlaminar window and intravertebral space in the higher intervertebral levels (L3/L4 or above).
Considering many aspects in the indication and selection process for the full-endoscopic operations, we applied following criteria as guidelines: radicular symptoms with or without motor deficit due to disc herniation within the spinal canal, level of lesion not above L3/L4, lumbar spine without degenerative deformities such as spondylolistesis or scoliosis, osteochondrosis and relative spinal canal stenosis were not contraindications.
Conclusions
The clinical results are similar but slightly better in the fullendoscopic technique compared to microsurgical operations with lower overall complication and recurrence-reoperation rate.
With the surgical devices and instruments all forms of lumbar disc herniations can be sufficiently removed using the full-endoscopic technique.
Full-endoscopic interlaminar technique is a reliable, safe and slightly superior alternative to microsurgical procedures when taking the appropriate indications criteria into account.
Open microsurgical and invasive procedures are necessary in spinal surgery and must be familiar and known by surgeons to overcome problems and complications when performing full-endoscopic procedures.
References
- Mixter WJ, Barr JS (1934) Rupture of intervertebral disc with involvement of spinal cord. N Engl J Med 211: 210-215.
- Ooi Y, Sato Y, Morisaki N (1973) Myeloscopy: the possibility of observing the lumbar intrathecal space by use of an endoscope. Endoscopy 5: 901-906.
- Foley KT, Smith MM (1997) Microendoscopic discectomy. Tech Neurosurg 3:301-307.
- Obenchain TG (1991) Laparoscopic lumbar discectomy: Case report. J Laparoendosc Surg 1: 145-149.
- Angevine PD, McCormick PC (2002) Outcomes research and lumbar discectomy. Neurosurg Focus 13: E8.
- Markovic M, Zivkovic N, Spaic M, Gavrilovic A, Stojanovic D, et al. (2016) Full-endoscopic interlaminar operations in lumbar compressive lesions surgery: Prospective study of 350 patients. "Endos" study. J Neurosurg Sci.
- Casal-Moro R, Castro-Menendez M, Hernandez-Blanco M, Bravo-Ricoy JA, Jorge-Barreiro FJ (2011) Long-termoutcome after microendoscopic diskectomy for lumbar disk herniation: A prospective clinical study with a 5-year follow-up. Neurosurgery 68: 1568-1575.
- Dewing CB, Provencher MT, Riffenburgh RH, Kerr S, Manos RE (2008) The outcomes of lumbar microdiscectomy in a young, active population: Correlation by herniation type and level. Spine 33: 33-38.
- Gempt J, Jonek M, Ringel F, Preuss A, Wolf P, et al. (2013) Long-term follow-up of standard microdiscectomy versus minimal access surgery for lumbar disc herniations. Acta Neurochir (Wien) 155: 2333-2338.
- Ruetten S, Komp M, Godolias G (2006) A new full-endoscopic technique for the interlaminar operation of lumbar disc herniations using 6 mm endoscopes: prospective 2-year results of 331 patients. Minim Invas Neurosurg 49: 80-87.
- Ruetten S, Komp M, Godolias G (2005) Full-endoscopic interlaminar operation of lumbar disc herniations using new endoscopes and instruments. Orthop Praxis 10: 527-532.
- Ruetten S (2005) The full-endoscopic interlaminar approach for lumbar disc herniations. In: Mayer HM, editors. Minimally Invasive Spine Surgery. Berlin Heidelberg New York: Springer; pp: 346-55.
- Griffith JF, Wang YX, Antonio GE, Choi KC, Yu A, et al. (2007) Modified Pfirrmann grading system for lumbar intervertebral disc degeneration. Spine 32: E708-712.
- Lee DY, Ahn Y, Lee SH (2006) Percutaneous endoscopic lumbar discectomy for adolescent lumbar disc herniation: Surgical outcomes in 46 consecutive patients. Mt Sinai J Med 73: 864-870.
- Lee SH, Chung SE, Ahn Y, Kim TH, Park JY, et al. (2006) Comparative radiologic evaluation of percutaneous endoscopic lumbar discectomy and open microdiscectomy: A matched cohort analysis. Mt Sinai J Med 73: 795-801.
- Mayer HM, Brock M (1993) Percutaneous endoscopic discectomy: Surgical technique and preliminary results compared to microsurgical discectomy. J Neurosurg 78: 216-225.
- Ruetten S, Komp M, Merk H, Godolias G (2008) Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine 33: 931-939.
- Kotilainen E, Valtonen S (1993) Clinical instability of the lumbar spine after microdiscectomy. Acta Neurochir 125: 120-126.
- Ebara S, Harada T, Hosono N, Inoue M, Tanaka M, et al. (1992) Intraoperative measurement of lumbar spine instability. Spine 17: 44-50.
- Faulhauer K, Manicke C (1995) Fragment excision versus conventional disc removal in the microsurgical treatment of herniated lumbar disc. Acta Neurochir 133: 107-111.
- Goel VK, Nishiyama K, Weinstein JN, Liu YK (1986) Mechanical properties of lumbar spinal motion segments as affected by partial disc removal. Spine 11: 1008-1012.
- Lida Y, Kataoka O, Sho T, Sumi M, Hirose T (1990) Postoperative lumbar spinal instability occuring or progressing secondary to laminectomy. Spine 15: 1186-1189.
- Kambin P, Cohen L, Brooks ML, Schaffer JL (1994) Development of degenerative spondylosis of the lumbar spine after partial discectomy: comparison of laminotomy, discectomy and posterolateral discectomy. Spine 20: 599-607.
- Mochida J, Toh E, Nomura T, Nishimura K (2001) The risks and benefits of percutaneous nucleotomy for lumbar disc herniation. A 10-year longitudinal study. J Bone Joint Surg Br 83: 501-505.
- Weber BR, Grob D, Dvorak J, Müntener M (1997) Posterior surgical approach to the lumbar spine and its effect on the multifidus muscle. Spine 22: 1765-1772.
- Caspar W, Campbell B, Barbier DD, Kretschmmer R, Gotfried Y (1991) The Caspar microsurgical discectomy and comparison with a conventional standard lumbar disc procedure. Neurosurgery 28: 78-87.
- Mayer HM (2000) The microsurgical interlaminar, paramedian approach. In: Mayer HM, editor. Minimally Invasive Spine Surgery. Berlin, Heidelberg, New York: Springer; pp: 79-91.
- Ramirez LF, Thisted R (1989) Complications and demographic characteristics of patients undergoing lumbar discectomy in community hospitals. Neurosurgery 25: 226-231.
- Rantanen J, Hurme M, Falck B, Alaranta H, Nykvist F, et al. (1993) The lumbar multifidus muscle five year after surgery for a lumbar intervertebral disc herniation. Spine 18: 568-574.
- Rompe JD, Eysel P, Zollner J, Heine J (1999) Intra- and postoperative risk analysis after lumbar intervertebral disk operation. Z Orthop 137: 201-205.
- Stolke D, Sollmann WP, Seifert V (1989) Intra- and postoperative complications in lumbar disc surgery. Spine 14: 56-59.
- Wildfoerster U (1991) Intraoperative complications in lumbar intervertebral disc operations, cooperative study of the spinal study group of the German Society of Neurosurgery. Neurochirurgica 34: 53-56.
- Wilson DH, Harbaugh R (1992) Lumbar discectomy: A comparative study of microsurgical and standard technique. In: Hardy RW, editor. Lumbar disc disease. New York: Raven Press; pp: 147-156.
- Mochida J, Nishimura K, Nomura T, Toh E, Chiba M (1996) The importance of preserving disc structure in surgical approaches to lumbar disc herniation. Spine 21: 1556-1563.
- Ross JS, Robertson JT, Frederickson RC, Petrie JL, Obuchowski N, et al. (1996) Association between peridural scar and recurrent radicular pain after lumbar discectomy: Magnetic resonance evaluation. Neurosurgery 38: 861-863.
- Balderston RA, Gilyard GG, Jones AA, Wiesel SW, Spengler DM, et al. (1991) The treatment of lumbar disc herniation: Simple fragment excision versus disc space curettage. J Spinal Disord 4: 22-25.
- Knight MTN, Goswami A, Patko JT, Buxton N (2001) Endoscopic foraminoplasty: A prospective study on 250 consecutive patients with independent evaluation. J Clin Laser Med Surg 19: 73-81.
- Saberski LR, Kitahata LM (1996) Persistent radiculopathy diagnosed and treated with epidural endoscopy. J Anesth 10: 1-4.
- Boyer P, Srour R, Buchheit F, Krause D, Albuquerque M (1994) Lumbar disc hernia. Excision of hernia with or without complementary discectomy? Neurochirurgie 40: 259-262.
- Wenger M, Mariani I, Kalbarczyk A, Gröger U (2001) Long-term outcome of 104 patients after lumbar sequestrectomy according to Williams. Neurosurgery 49: 329-335.
- Hirabayashi S, KumanoK, Ogawa Y, Aota Y, Maehiro S (1993) Microdiscectomy and second operation for lumbar disc herniation. Spine 18: 2206-2211.
- Stambough JL (1997) Lumbar disk herniation: An analysis of 175 surgically treated cases. J Spinal Disord. 10: 488-492.
- Carragee EJ, Spinnikie AO, Alamin TF, Paragioudakis S (2006) A prospective controlled study of limited versus subtotal posterior discectomy: Short-term outcomes in patients with herniated lumbar intervertebral discs and large posterior anular defect. Spine 31: 653-657.
- Caragee EJ, Han MY, Suen PW, Kim D (2003) Clinical outcomes after discectomy for Sciatica: The effects of fragment type and anular competence. J Bone J Surg Am 85:102-108.
- Ruetten S, Komp M, Merk H, Godolias G (2009) Recurrent lumbar disc herniation after conventional discectomy: A prospective, randomized study comparing full-endoscopic interlaminar and transforaminal versus microsurgical revision. J Spinal Disord Tech 22: 122-128.
- Ahn SS, Kim SH, Kim DW, Lee BH (2016) Comparison of outcomes of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for young adults: A retrospective matched cohort study, World Neurosur 86: 250-258.
- Zollner J, Rosendahl T, Herbsthofer B (1999) The effect of various nucleotomy techniques on biomechanical properties of the intervertebral disc. Z Orthop 137: 206-210.
- Suk KS, Lee HM, Moon SH, Kim NH (2001) Recurrent lumbar disc herniation: Results of operative management. Spine 26: 672-676.
- Annerzt M, Jonsson B, Stromqvist B, Holtas S (1995) No relationship between epidural fibrosis and sciatica in the lumbar postdiscectomy syndrome. A study with contrast-enhanced magnetic resonance imaging in symptomatic and asymptomatic patients. Spine 20: 449-453.
- Schoeggl A, Maier H, Saringer W, Reddy M, Matula C (2002) Outcome after chronic sciatica as the only reason for lumbar microdiscectomy. J Spinal Disord Tech 15: 415-419.
- Ruetten S, Meyer O, Godolias G (2002) Epiduroscopic diagnosis and treatment of epidural adhesions in chronic back pain syndrome of patients with previous surgical treatment: First results of 31 interventions. Z Orthop 140: 171-175.
- Aydin Y, Ziyal IM, Durnam H, Turkmen CS, Basak M, et al. (2002) Clinical and radiological results of lumbar microdiscectomy technique with preserving of ligamentum flavum comparing to the standard microdiscectomy technique. Surg Neurol 57: 5-13.
- De Devitiis E, Cappabianca P (2002) Lumbar discectomy with preservation of the ligamentum flavum. Surg Neurol 58: 68-69.
- Law JD, Lehman RAW, Kirsch WM (1978) Reoperation after lumbar intervertebral disc surgery. J Neurosurg 94: 259-263.
- Kim SS, Michelsen CB (1992) Revision surgery for failed back surgery syndrome. Spine 17: 957-960.
- Fritsch EW, Heisel J, Rupp S (1996) The failed back surgery syndrome: Reasons, intraoperative findings and long term results: A report of 182 operative treatments. Spine 21: 626-633.
- Katz JN, Lipson SJ, Larson MG, McInnes JM, Fossel AH, et al. (1991) The outcome of decompressive laminectomy for degenerative lumbar stenosis. J Bone J Surg Am 73: 809-816.
- Markwalder TM (1993) Surgical management of neurogenic claudication in 100 patients with lumbar spinal stenosis due to degenerative spondylolisthesis. Acta Neurochir 120: 136-142.
- Ragab AA, Fye MA, Bohlmann HH (2003) Surgery of the lumbar spine for spinal stenosis in 118 patients 70 years of age or older. Spine 28: 348-353.
- Lewis PJ, Weir BKA, Broad RW, Grace MG (1987) Long-term prospective study of lumbosacral discectomy. J Neurosurg 1987; 67: 49-54.
- Cooper R, Mitchell W, Illimgworth KJ, Forbes WS, Gillespie JE, et al. (1991) The role of epidural fibrosis and defective fibrinolysis in the persistence of postlaminectomy back pain. Spine 16: 1044-1048.
- Ruetten S, Komp M, Merk H, Godolias G (2007) Use of newly developed instruments and endoscopes: Full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J Neurosurg Spine 6: 521-530.
- Le H, Sandhu FA, Fessler RG (2003) Clinical outcomes after minimal-access surgery for recurrent lumbar disc herniation. Neurosurg Focus 15: E12.
- Ruetten S, Komp M, Merk H, Godolias G (2007) A new full-endoscopic technique for cervical posterior foraminotomy in the treatment of lateral disc herniations using 6.9 mm endoscopes: Prospective 2-year results of 87 patients. Minim Invasive Neurosurg 50: 219-226.
- Ruetten S, Meyer O, Godolias G (2003) Endoscopic surgery of the lumbar epidural space (epiduroscopy): Results of therapeutic intervention in 93 patients. Minim Invasive Neurosurg 46: 1-4.
- Ruetten S, Meyer O, Godolias G (2002) Application of holmium: YAG laser in epiduroscopy: Extended practicabilities in the treatment of chronic back pain syndrome. J Clin Laser Med Surg 20: 203-206.
- Briseno MR, Phukan RD, Leonard DA, Herzog TL, Cho CH, et al. (2015) The influence of adjacent level disc disease on discectomy outcomes. Eur Spine J 25: 230-234.
- Hong X, Liu L, Bao J, Shi R, Fan Y, et al. (2015) Characterization and risk factor analysis for reoperation after microendoscopic diskectomy. Orthopedics 38: e490-496.
- Corniola MV, Stienen MN, Joswig H, Chau I, Hildebrandt G, et al. (2015) Correlation of pain, functional disability, and health-related quality of life with radiological grading scales for lumbar degenerative disc disease. J Neurol Surg A Cent Eur Neurosurg.
Citation: Markovic M, Zivkovic N, Ruetten S, Ozdemir S, Goethel D (2017) Full-Endoscopic Interlaminar Versus Microsurgical Operations in Lumbar Compressive Lesions Surgery: Prospective Randomized Trial of Overall 570 Patients. J Pain Relief 6: 304. DOI: 10.4172/2167-0846.1000304
Copyright: © 2017 Markovic M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4998
- [From(publication date): 0-2017 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 4157
- PDF downloads: 841