Frequency and Severity of Low Back Pain among Healthcare Providers and Associated Factors in a Tertiary Care, Public Hospital in Karachi
Received: 25-Jan-2019 / Accepted Date: 04-Mar-2019 / Published Date: 11-Mar-2019 DOI: 10.4172/2329-6879.1000285
Abstract
Introduction: Health care workers are known to have relatively higher burden of musculoskeletal problems including low back pain as compared to other occupational groups due to their specific ergonomics exposures at work. This study aims to determine the frequency of low back pain, its associated factors and level of functional disability due to low back pain among health care providers working in a tertiary care public hospital in Karachi.
Methodology: A cross-sectional survey was conducted among healthcare providers (doctors, nurses and paramedics) working in a tertiary care public hospital in Karachi, Pakistan. All 300 study participants were enquired about complain of low back pain in past 12 months and participants who had low back pain were assessed for low back pain associated functional disability using modified Oswestry Disability Index (ODI). Data was analyzed using SPSS version 19.
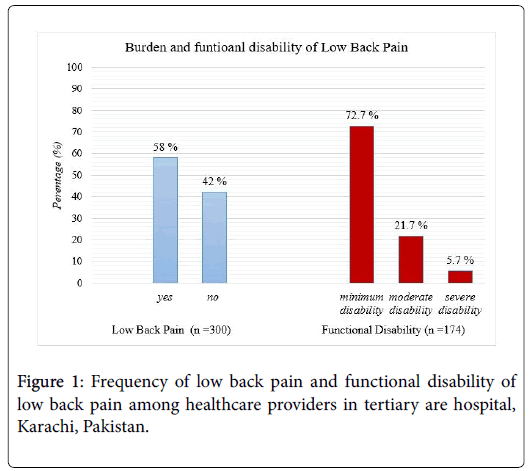
Results: 58% of all healthcare providers included in the survey reported to experience low back pain in last 12 months. 72.6% of all the healthcare providers with low back pain had minimum disability. While 27.4% of all healthcare providers with low back pain were found to have moderate to severe functional disability affecting their social and work related life. The study found positive association of low back pain with functional disability with an OR: 1.82 (95% CI: 1.56, 2.13). Worker experience >5 years OR: 2.70 (95% CI: 1.21, 6.03), lifting heavy objects / patients OR 2.14 (95% CI: 1.28, 3.55), family history OR: 1.98 (95%CI: 1.17, 3.36) (p-value <0.05).
Conclusion: Healthcare providers have considerably high prevalence of low back pain. A substantial proportion of healthcare providers are suffering from functional disability associated with low back pain; affecting their social and work life. There is need of multilevel interventions for prevention and control of low back pain in this highly vulnerable occupational group.
Keywords: Low back pain; Disability; Occupational health; Healthcare providers
Introduction
Low back pain (LBP) is a common health problem caused by physical stress and strain. Globally 37% of all LBP cases are caused by work related ergonomic exposures resulting in an annual loss of 818,000 disability-adjusted life years [1]. Healthcare provider is a term which represents a particular occupational group with a variety of skilled cadre including doctor, nurses, nursing assistants and paramedics involved in direct patient care and provision of healthcare services. This particular occupational group is known to have relatively higher burden of musculoskeletal problems including LBP as compared to other occupational groups due to their specific ergonomics exposures at work [2].
A systematic review of musculoskeletal disorders among healthcare providers estimated that 12 months prevalence of LBP among healthcare providers was 25% irrespective of their work category [2]. Burdford and colleagues conducted a literature review of 35 studies to assess the association of back disorders and work related risk factors and concluded that lifting or carrying loads, whole-body vibration, and frequent bending and twisting were consistently associated with workrelated back disorders. However, age, smoking habits, and education were identified as important confounders [3]. Another systematic review of 89 studies supporting high burden of LBP among nurses found that work related activities among nurses were associated with back disorders regardless of nursing technique, personal characteristics, and non-work-related factors [4]. Patient handling appeared to confer the highest risk, but other nursing duties were found to be associated with elevated risk and identified as important confounder [4].
A survey conducted by the Korea Occupational Safety and Health Agency (KOSHA) in 2014 to identify ergonomic risk factors associated with work-related LBP. The study found that fatigue-inducing and painful posture (aOR:5.0), lifting or moving people (aOR:1.98); dragging or pushing, or moving heavy objects (aOR:2.09); standing posture(aOR:1.79) repetitive hand or arm movements (aOR:2.04) were major ergonomic factors associated with complain of LBP [5].
Pakistan is a developing country with limited awareness and trainings regarding occupational health and safety. There is dearth of research on occupational diseases among healthcare providers. Hence, there is a dire need to assess the frequency of LBP and level of functional disability in this vulnerable occupational group. However, determining the factors associated with LBP among healthcare providers would help in developing relevant and effective interventions for prevention of this occupational health problem. This study aims to determine the frequency of LBP, its associated factors and level of functional disability due to LBP among healthcare providers working in a tertiary care public hospital in Karachi.
Methods
Study design and setting
A cross-sectional survey was conducted among health care providers working in a tertiary care public hospital in Karachi from November, 2015 to March, 2016. The study was conducted in Jinnah Post Graduate Center (JPMC). JPMC is one of the biggest tertiary care public hospital and clinical training institute in Karachi. The institute shares major burden of public sector and offers quality care through qualified and multidisciplinary health team.
Participant recruitment: Healthcare providers including doctors, nurses and paramedical staff who were working in the same job for at least 12 months were invited to participate in this study. Study participants were selected using convenient sampling technique. However, healthcare providers with history of congenital musculoskeletal any deformity, acquired bone deformity or history of spinal injury or epidural procedures were excluded from the study.
The sample size for this study was calculated using Open Epi Software with 21% anticipated proportion of LBP among health care providers in the reference population and Odds Ratio of 1.98 for ergonomic risk factors such as lifting and dragging people or moving heavy objects [5,6]. At 95% level of confidence, precision of 5% and power of 80% a final sample size of 300 participants was obtained.
Data collection: The information regarding socio-demographic and occupational details of study participants was collected using a structured, self-administered questionnaire. Each study participant was enquired about complain of LBP in past 12 months period. The definition of LBP was adapted from work of Hoy and colleagues describing back pain as pain on the posterior aspect of the body from the twelfth ribs to the lower gluteal folds which may or may not be referred to lower limb(s) [7].
Assessment of functional disability: The level of functional disability due to LBP was assessed using Oswestry Disability Index (ODI). ODI has been widely recognized by researchers for its good internal consistency and test-retest reliability (kappa=0.9) for measurement of functional disability [8-10].
The ODI tool is consist of 10 items addressing different motor functions such as walking, sitting, standing, lifting, sleeping and traveling. Each item is scored from 0 to 5, with higher values representing greater disability. The total score is multiplied by 2 and expressed as a percentage. The disability level is classified into five categories on the basis of scores ranging from minimal disability to bed bound disability on the basis of pre-designed scoring system (Appendix-I). This study used ODI to assess the level of disability among healthcare providers who had complain of LBP at the time of survey. The study used a modified version of ODI in which an item related to sex life is replaced by questions on pain intensity. The internal consistency and reliability of this modified version of ODI is well supported by previous researchers [11].
Statistical analysis
Data was double entered using EPI Data version 3.1 and data was analyzed using SPSS version 19. Descriptive statistics were run to determine the frequency and proportions of LBP and distribution of socio-demographic and job related characteristics. Proportions for various levels of functional disability due to LBP were calculated. Chi square test of significance was applied to assess statistically significant difference in frequency of LBP among healthcare providers with different socio-demographic characteristics. Linear regression was applied to determine possible association between LBP with various factors including age, work hours, gender, education and nature of job.
Ethical considerations
The written informed consent was taken from each participant before the data collection. The purpose and procedure of data collection was explained in details to each participant. The study participants who were found to have moderate to severe functional disability were advised and referred for further work-up and management. Ethical approval for this study was obtained from Institutional Review Board (IRB) of Jinnah Sindh Medical University, Karachi.
Results
The mean age of the study participants was 29.7 years ± 7 SD. 65% of the study participants were female while 35% were males. Detailed socio-demographic and work related information is given in Table 1.
| Characteristics | Frequency (n) | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 105 | 35 |
| Female | 195 | 65 |
| Ethnicity | ||
| Urdu | 137 | 45.7 |
| Punjabi | 67 | 22.3 |
| Sindhi | 47 | 15.7 |
| Others1 | 49 | 16.3 |
| Education status | ||
| Undergraduate | 72 | 24 |
| Graduation | 155 | 51.7 |
| Post-Graduation | 73 | 24.3 |
| Monthly household income (PKR) | ||
| ≤ 10 thousand | 40 | 13.3 |
| 10-25 thousand | 87 | 29 |
| >25 thousand | 173 | 57.7 |
| Type of health worker | ||
| Doctor | 141 | 47 |
| Nurse | 123 | 41 |
| Others2 | 36 | 12 |
| Work experience | ||
| ≤ 5 years | 177 | 59 |
| >5 years | 123 | 41 |
| Working hours per day | ||
| ≤ 8 hours | 205 | 68.3 |
| >8 hours | 95 | 31.7 |
| BMI (kg/m2) | ||
| Normal | 178 | 59.3 |
| Malnourished | 39 | 13 |
| Overweight | 68 | 22.7 |
| Obese | 15 | 5 |
| Past Medical History | ||
| No Disease | 260 | 86.7 |
| Hypertension | 20 | 6.7 |
| Diabetes | 4 | 1.3 |
| Vitamin D Deficiency | 2 | 0.7 |
| Injury | 8 | 2.7 |
| Other | 6 | 2 |
| Smoking history | ||
| Yes | 24 | 8 |
| No | 276 | 92 |
Table 1: Frequency distribution of socio-demographic and job related characteristics among health care providers in tertiary are hospital, Karachi Pakistan. (n=300).
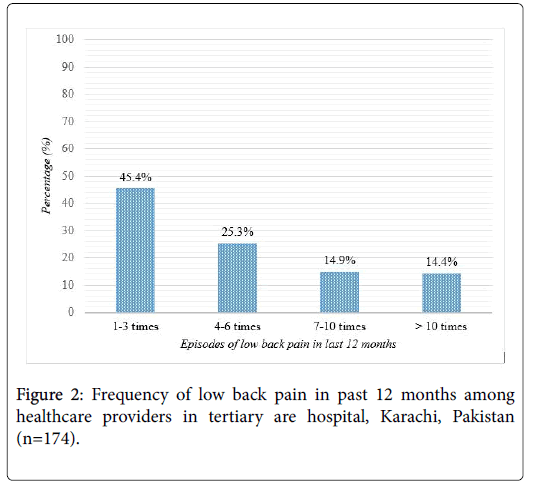
58% of all healthcare providers included in the survey reported to experience LBP in last 12 months irrespective of the frequency of pain. Assessment of functional disability was conducted using “Oswestry Low Back Pain Scale” among healthcare providers who reported LBP. 27.4% of all the healthcare providers with LBP found to have moderate to severe functional disability (Figure 1). However, among all the study participants who experienced LBP in last 12 months most of them experienced LBP with a frequency ranging from one to three times only (Figure 2).
The comparison for frequency of LBP among health care providers found significant difference with socio-demographic and job related characteristics. The proportion of LBP was more among healthcare providers of age >30 years, those having a monthly income of ≤ 25 thousand, having job shift of more than eight hours (>8 hours), among those involved in lifting or moving heavy objects, and having a positive family history of LBP (p<0.05) (Table 2).
| Low back pain n (%) | |||
|---|---|---|---|
| Characteristics | No | Yes | p-value |
| Gender | |||
| Female | 79 (40.5) | 116 (59.5) | 0.477 |
| Male | 47 (44.8) | 58 (55.2) | |
| Age | |||
| ≤ 30 years | 100 (48.8) | 105 (51.2) | 0.000* |
| >30 years | 26 (27.4) | 69 (72.6) | |
| Ethnicity | |||
| Urdu | 56 (40.9) | 81 (59.1) | 0.625 |
| Sindhi | 17 (36.2) | 30 (63.8) | |
| Punjabi | 29 (43.3) | 38 (56.7) | |
| Others | 24 (49) | 25 (51) | |
| Education status | |||
| Under graduation | 36 (50) | 36 (50) | 0.115 |
| Graduation and above | 90 (39.5) | 138 (60.5) | |
| Monthly income (PKR) | |||
| ≤ 25 thousand | 60 (34.7) | 113 (65.3) | 0.003* |
| >25 thousand | 66 (52) | 61 (48) | |
Table 2: Comparison for frequency of low back pain among health care providers with socio-demographic and job related characteristics in tertiary care hospital in Karachi. (n=300).
Multiple logistic regression model found the positive association of LBP with work experience. Healthcare providers who had more than 5 years of experience were more likely to develop LBP OR: 2.89 (95% CI: 1.58, 5.27). The healthcare providers involved in lifting and moving heavy objects at work were more likely to develop LBP OR 2.21 (95% CI: 1.33, 3.70). Similarly, LBP was more likely to occur among healthcare providers with family history of LBP OR: 1.76 (95%CI: 1.15, 2.95) (p<0.05) (Table 3).
| Characteristics | unadjusted odds ratio (95% CI) | adjusted odds ratio (95% CI) | p-value |
|---|---|---|---|
| Age | |||
| ≤ 30 years | ref | ref | <0.05 |
| >30 years | 2.52 (1.49, 4.28)* | 2.05 (1.11,3.78)* | |
| Healthcare providers’ type | |||
| Doctor | ref | ref | |
| Nurse | 1.10 (0.67,1.80) | 1.37 (0.69, 2.71) | 0.35 |
| Others | 1.38 (0.65,2.96) | 1.97 (0.83,4.06) | 0.12 |
| Work experience | |||
| ≤ 5 years | ref | ref | <0.05 |
| >5 years | 3.01 (1.83, 4.95)* | 2.89 (1.58, 5.27)* | |
| Working hours per day | |||
| ≤ 8 hours | ref | ref | <0.05 |
| >8 hours | 2.04 (1.22, 3.42)* | 2.30 (1.28, 4.14)* | |
| Manually lift heavy objects | |||
| No | ref | ref | <0.05 |
| Yes | 2.03 (1.27, 3.23)* | 2.21 (1.33, 3.70)* | |
| Physical exercise | |||
| Yes | ref | ref | 0.07 |
| No | 1.66 (0.99, 2.79) | 1.65 (0.95, 2.86) | |
| Family history of low back pain | |||
| No | ref | ref | <0.05 |
| Yes | 1.82 (1.10, 2.99)* | 1.76 (1.15, 2.95)* | |
| Co-morbidity | |||
| No | ref | ref | 0.53 |
| Yes | 1.59 (0.78, 3.23) | 1.09 (0.40,2.93) | |
| Adjusted for age, sex, education, monthly income, ethnicity, BMI and smoking history. *p<0.05 significant | |||
Table 3: Logistic regression showing the association of low back pain with functional disability and other factors among health care workers in tertiary care hospital, Karachi (n=300).
Discussion
This study is a unique effort in the context of Pakistan, while focusing a common but neglected occupational health problem among healthcare providers in a developing country. This study found that 58% of all healthcare providers included in the study had suffered from LBP in last 12 months. This finding indicates considerably high frequency of LBP among healthcare providers working in one of the biggest tertiary care hospital in mega city of Karachi, Pakistan. This finding is in line with the findings from previously conducted studies in other developing countries including India, Malaysia and Iran. This can be explained by similar social context, as well as health management systems. A systematic review of 11 studies was conducted to estimate the prevalence of LBP among healthcare providers in Iran. The systematic review found that 58% of all healthcare providers in Iran had LBP in last 12 months. The review also concluded that healthcare providers in Iran had highest frequency of LBP in last 12 months as compared to various other occupational groups [2]. Similarly, another study conducted among healthcare providers working in a tertiary care hospital in Turkey found comparable prevalence of LBP among healthcare providers during last 12 months i.e. 59.7% [12]. Another study conducted in 2010 in district hospital Sibu, Malaysia found 56.9% prevalence of LBP in last 12 months [13]. However another study conducted among doctors working in a hospital in Selangor, Malaysia in 2009 reported a 12 month prevalence of 65% for LBP [14]. A multi-center study conducted among nurses working in selected hospitals in rural Maharashtra, India found 12 months prevalence of 48% for LBP [15]. Another multicenter study conducted in six hospitals in Turkey estimated 12 months LBP prevalence of 61.3% among hospital workers including nurses, physicians, physical therapists, technicians, and hospital aides [16]. The slight differences in frequency of LBP frequency in our study and studies conducted in other developing countries can be explained by differences in categories of healthcare providers or job description, differences in workload as well as possible differences in work environment of hospitals included in each study.
In our study the LBP was significantly more prevalent among healthcare providers of age above 30 years, work experience of more than five years, more than eight work hours in a day, lifting of heavy objects and family history of LBP. This study determined statistically significant association between LBP among healthcare providers and all the above mentioned factors (p-value <0.05). The association of LBP among healthcare workers with age and heavy lifting is previously established by studies conducted in Turkey, Korea [5,16,17]. A quantitative assessment of previously conducted studies investigated effect of manually lifting patients on LBP occurrence and impact of introducing lifting devices on frequency of LBP. The study concluded that elimination of manual lifting of patient by nurses and use of patient lifting devices can bring considerable reduction in frequency of LBP among nurses [18] Nevertheless, musculoskeletal problems including LBP resulting from repositioning and pulling patients up in bed, or catching falling patients cannot be prevented by the use of patient lifting devices and may require additional multilevel interventions [19]. However, this study found no association between healthcare providers` category, physical activity and known comorbidities such as hypertension, diabetes and vitamin D deficiency. Due to heavy workload and limited human resource the overlapping of patient care related tasks is a common problem in public hospitals developing countries like Pakistan. This may have resulted in failure to establish any possible association in this particular group of healthcare providers. Moreover, lack of association of comorbidities and physical activity with LBP can be explained by limited validity of study methods used to gather information about above mentioned variables. Furthermore, majority of all healthcare providers who reported to experience LBP in last 12 months had minimum functional disability and were able to perform their routine activities as required. However, 27.4% of all healthcare providers were suffering from moderate to severe functional disability which was affecting their day to day activities including social as well as work related activities. This highlights the actual burden of physical and social suffering among healthcare providers in the biggest and one of the busiest tertiary care hospitals in Karachi. The LBP related functional disability might be affecting the service delivery quality and healthcare providers` motivation towards work.
Despite limited scope this study has highlighted the frequency of LBP and associated functional disability among healthcare providers. The study simultaneously assessed multiple risk factors such as work hours, lifting heavy objects or lifting patients, work experience, age and family history of LBP
Limitations
This study has few limitations. First, this was a cross-sectional survey which cannot establish temporality hence results should be interpreted with caution. Secondly, the information regarding complain of LBP and work related ergonomic exposures were selfreported and might be affected by the recall bias as well as volunteer bias. Similarly, use of self-reports to evaluate ergonomic risk factors and self-reported history of co-morbidity including vitamin D deficiency have certain inherent shortcomings and lack validity [20]. Moreover, this study might have underestimated the actual frequency of functional disability due to LBP as those who had crippling disability and could not continue their job were naturally excluded from the survey. Furthermore, this study did not adjust for the possible confounding effect of psychosocial factors, knowledge and training regarding occupational safety and use of personal protective measures as well as patient lifting equipment or devices.
Conclusion
This study suggests need of interventions to prevent and control occupational risk factors of LBP among healthcare providers such as work hours and lifting heavy objects or patients. However, multilevel interventions are required to control the effect of age, work experience and comorbidity. Multi-center study with enhanced methodology is required to understand the actual burden of LBP and its related disability to identify possible strategies and interventions for its prevention and control in the particular context of this highly vulnerable occupational group in local as well as national level.
References
- Punnett L, Prüss-Utun A, Nelson DI, Fingerhut MA, Leigh J, et al. (2005) Estimating the global burden of low back pain attributable to combined occupational exposures. Am J Ind Med 48: 459-469.
- Mehrdad R, Shams-Hosseini NS, Aghdaei S, Yousefian M (2016) Prevalence of low back pain in health care workers and comparison with other occupational categories in Iran: A systematic review. Iran J Med Sci 41: 467-478.
- Burdorf A, Sorock G (1997) Positive and negative evidence of risk factors for back disorders. Scand J Work Environ Health 23: 243-256.
- Yassi A, Lockhart K (2013) Work-relatedness of low back pain in nursing personnel: A systematic review. Int J Occup Environ Health 19: 223-244.
- Kim JY, Shin JS, Lim MS, Choi HG, Kim SK, et al. (2018) Relationship between simultaneous exposure to ergonomic risk factors and work-related lower back pain: A cross-sectional study based on the fourth Korean working conditions survey. Ann Occup Environ Med 30: 58.
- Landry MD, Raman SR, Sulway C, Golightly YM, Hamdan E (2008) Prevalence and risk factors associated with low back pain among health care providers in a Kuwait hospital. Spine (Phila Pa 1976) 33: 539-545.
- Hoy D, March L, Brooks P, Woolf A, Blyth F, et al. (2010) Measuring the global burden of low back pain. Best Pract Res Clin Rheumatol 24: 155-165.
- Fairbank JC, Couper J, Davies JB, O’brien JP (1980) The oswestry low back pain disability questionnaire. Physiotherapy 66: 271-273.
- a name="_ENREF_9">Fritz JM, Irrgang JJ (2001) A comparison of a modified oswestry low back pain disability questionnaire and the quebec back pain disability scale. Phys Ther 81: 776-788.
- Changulani M, Shaju A (2009) Evaluation of responsiveness of oswestry low back pain disability index. Arch Orthop Trauma Surg 129: 691-694.
- Hudson-Cook N (1989) Revised Oswestry disability questionnaire. Back pain: New approaches to rehabilitation and education.
- Terzi R, Altın F (2015) The prevalence of low back pain in hospital staff and its relationship with chronic fatigue syndrome and occupational factors. Agri 27: 149-154.
- Wong TS, Teo N, Kyaw MO (2010) Prevalence and risk factors associated with low back pain among health care providers in a district hospital. Malays Orthop J 4: 23-28.
- Lee KY, Farhanah BN, Rifaaie MH, Chang CY, Hassan STS, et al. (2014) Prevalence of low back pain and its associated factors among doctors in a hospital in Selangor. Int J Res Med Sci 1: 189-197.
- Anap DB, Iyer C, Rao K (2017) Work related musculoskeletal disorders among hospital nurses in rural Maharashtra, India: A multi centre survey. International Journal of Research in Medical Sciences 1: 101-107.
- Karahan A, Kav S, Abbasoglu A, Dogan N (2009) Low back pain: Prevalence and associated risk factors among hospital staff. J Adv Nurs 65: 516-524.
- Rezaee M, Ghasemi M (2014) Prevalence of low back pain among nurses: Predisposing factors and role of work place violence. Trauma Mon 19: e17926.
- Burdorf A, Koppelaar E, Evanoff B (2013) Assessment of the impact of lifting device use on low back pain and musculoskeletal injury claims among nurses. Occup Environ Med 70: 491-497.
- Pompeii LA, Lipscomb HJ, Schoenfisch AL, Dement JM (2009) Musculoskeletal injuries resulting from patient handling tasks among hospital workers. Am J Ind Med 52: 571-578.
- David GC (2005) Ergonomic methods for assessing exposure to risk factors for work-related musculoskeletal disorders. Occup Med (Lond) 55: 190-199.
Citation: Tanzil S, Jamali T, Inam SNB, Abbas A (2019) Frequency and Severity of Low Back Pain among Healthcare Providers and Associated Factors in a Tertiary Care, Public Hospital in Karachi. Occup Med Health Aff 7:285. DOI: 10.4172/2329-6879.1000285
Copyright: © 2019 Tanzil S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3276
- [From(publication date): 0-2019 - Apr 16, 2025]
- Breakdown by view type
- HTML page views: 2456
- PDF downloads: 820