Fractures in Children: Practical Approach to Reduce Missed Diagnosis
Received: 21-Dec-2022 / Manuscript No. roa-22-84333 / Editor assigned: 23-Dec-2022 / PreQC No. roa-22-84333 (PQ) / Reviewed: 06-Jan-2023 / QC No. roa-22-84333 / Revised: 23-Jan-2023 / Manuscript No. roa-22-84333 (R) / Published Date: 30-Jan-2023 DOI: 10.4172/2167-7964.1000419
Abstract
Fractures in children are common due to increased physical activity and their regular engagement in sports. Pediatric fractures can be subtle and easily missed on plain radiographs. This can be caused by many factors including those related to patients, technical, clinical, and radiological. The immature skeleton has a few unique features that can add to increased incidence of missed non-displaced fractures, however, some of these structural characteristics play a positive favourable role in the healing process of these fractures. Missed fractures in pediatrics can lead to long-term deformities or physical disabilities. In this mini-review article, we go through some of the factors contributing to missed diagnosis, go through few examples of subtle fractures in upper limb and the best technique to decrease the incidence of missed diagnosis.
Keywords
Fracture; Pediatric; Buckling; Greenstick; Radiology; X-ray
Introduction
The incidence of acute injury is up to 90% of orthopaedic emergency patients. It forms almost 85% of skeletal injuries in pediatrics [1-3]. In daily practice in the emergency department, it is common to miss the diagnosis of a subtle fracture in children, which can cause delayed treatment, and depending on the fracture’s location, malfunction or serious disabilities can occur [4,5]. Up to 24% of harm-causing missed diagnosis in emergency departments are caused by misinterpretation of fractures [6,7]. Diagnosing a fracture in children has some challenges related to the presence of the growth or physeal plate, anatomical skeletal variation and the variation in bones, ligaments, and tendons structural anatomy in children. Hereby we will discuss these anatomical variations, technical factors and the radiological reasons for missing fractures in children.
Bones and tendons anatomical structural variations
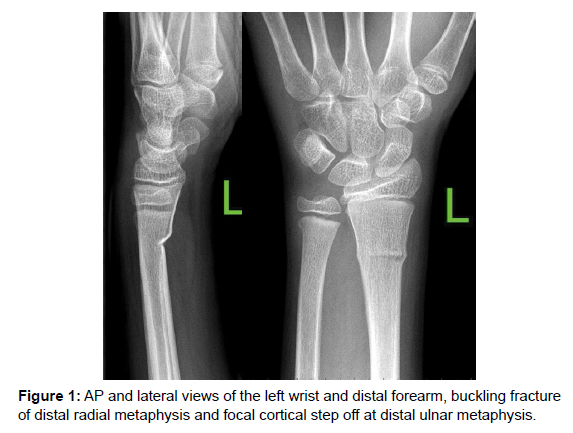
Immature skeletons in children have specific anatomical variations from adults that predispose children to specific fracture types [8]. These unique features include the more porous cortical bones, the thickened strong periosteum, the strong tendons attachment to apophyses, and the open cartilaginous physeal plates. The cortical bones are more porous than adults’ bones due to wider Haversian canals in the compact bones in children [9], which results in increased elasticity of pediatric bones and predispose to plastic fractures in children. The periosteum’s increased strength adds to the elasticity of bones. The thick strong periosteum prevents the cortical break in torus, buckling, fractures and green stick fractures, (Figure 1). Therefore, prevents the bony fragments displacement that can obscure the non-displaced fracture on a plain x-ray. However, both features of increased porosity and thick periosteum help in stabilizing the fracture by reducing fragments’ displacement, thus, promote a faster healing process and better re-modelling in children’s fractures [10]. Tendons in growing skeleton attach strongly to the periosteum, which results in frequent avulsion fractures in sports injuries. The apophyseal injury prevalence is higher in the immature bones of children playing sports due to the anatomically weaker apophysis compared to the attached tendon of muscles [11]. Lastly, the characteristic cartilaginous physeal plates are considered a weak point in immature long bones, if injured, can lead to growth deformity or to a premature growth plates’ closure. However, they enhance the bone re-modelling during the healing process. Salter- Harris classification categorizes fractures around the physeal plate as per the adjacent bony parts or physis involvement [10,12].
Technical clinical and radiographic factors
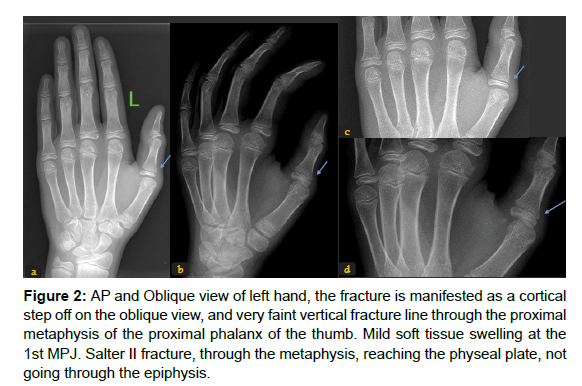
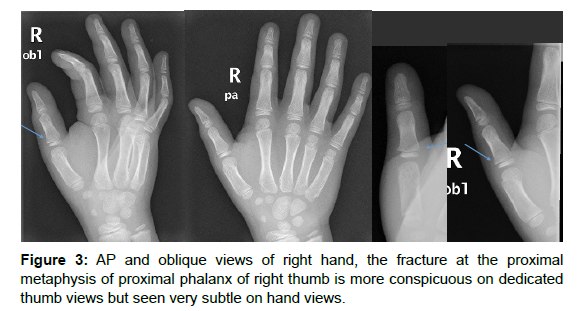
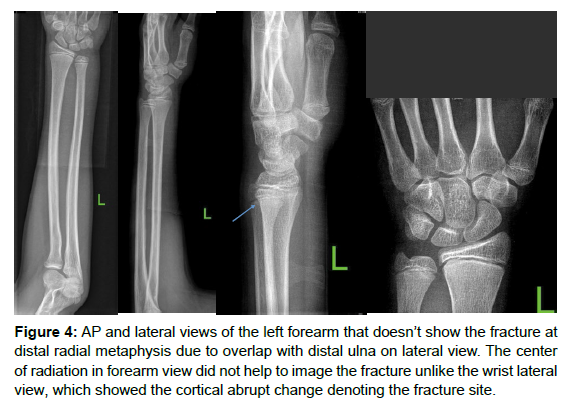
The injured child can present to the emergency department with no obvious limb deformity or localized swelling. The pain may radiate to areas other than the injured bone. This can affect the radiographs requested by the emergency physicians. As a result, if the thumb is injured, it is common to miss the thumb fracture on a hand anterioposterior, AP, and oblique views without dedicated thumb views, (Figures 2 and 3). Similarly, the distal radial subtle fracture can be missed on the two views forearm x-ray because it is not in the focus of the radiation beam (Figure 4).
Figure 2: AP and Oblique view of left hand, the fracture is manifested as a cortical step off on the oblique view, and very faint vertical fracture line through the proximal metaphysis of the proximal phalanx of the thumb. Mild soft tissue swelling at the 1st MPJ. Salter II fracture, through the metaphysis, reaching the physeal plate, not going through the epiphysis.
Figure 4: AP and lateral views of the left forearm that doesn’t show the fracture at distal radial metaphysis due to overlap with distal ulna on lateral view. The center of radiation in forearm view did not help to image the fracture unlike the wrist lateral view, which showed the cortical abrupt change denoting the fracture site.
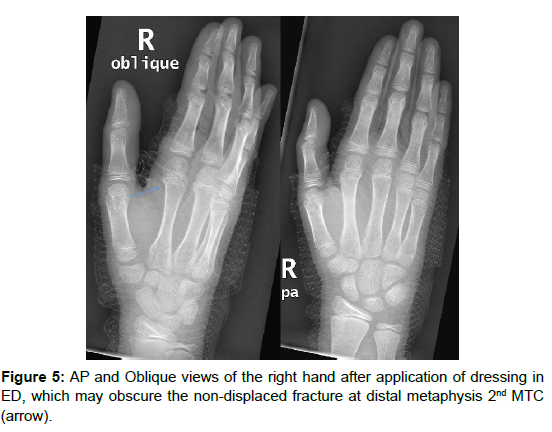
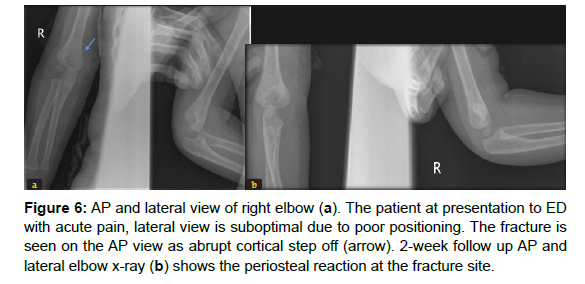
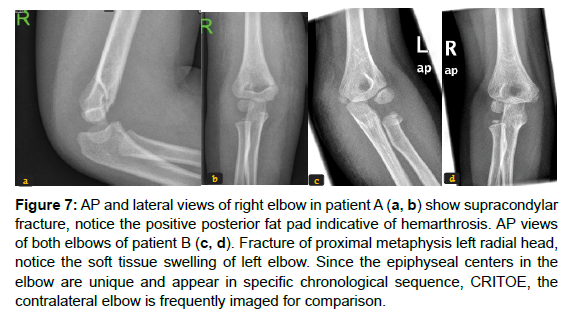
Some of the factors to obscure the fracture is the initial treatment at the emergency department, including dressing or a splint application as they reduce the fine details visibility of small bones in hands and feet, leading to missing fractures in the inherently small and osteopenic bones (Figure 5). Proper positioning of the imaged part of the body helps to align bones in an orthogonal position, which is crucial to diagnose a fracture. Therefore, when the injured children are in pain and cannot position their extremities properly, the radiological assessment can miss an occult fracture. The lateral view of elbows is a common example, it shows the displacement of fat planes that suggests joint effusion or hemarthrosis in a trauma setting, and the drawn lines through the intact distal humerus should normally align with the intact proximal radius and ulna. When the position in a lateral view of elbow is sub-optimal, the radiologist cannot assess the elevated anterior fat pad or positive posterior fat pad, the indirect signs of an occult fracture of an elbow bone (Figures 6 and 7).
Figure 6: AP and lateral view of right elbow (a). The patient at presentation to ED with acute pain, lateral view is suboptimal due to poor positioning. The fracture is seen on the AP view as abrupt cortical step off (arrow). 2-week follow up AP and lateral elbow x-ray (b) shows the periosteal reaction at the fracture site.
Figure 7: AP and lateral views of right elbow in patient A (a, b) show supracondylar fracture, notice the positive posterior fat pad indicative of hemarthrosis. AP views of both elbows of patient B (c, d). Fracture of proximal metaphysis left radial head, notice the soft tissue swelling of left elbow. Since the epiphyseal centers in the elbow are unique and appear in specific chronological sequence, CRITOE, the contralateral elbow is frequently imaged for comparison.
One of the essential orthopedic assessment rules is to image each body part or limb in two perpendicular-orthogonal views, and to include the proximal and distal joints. Occasionally, the images of the contralateral limb provide a good comparative image, especially in elbows, (Figure 7c, d). If clinical suspicion is high despite negative radiologic reports, doing a follow-up imaging can increase fracture visibility due to disuse-osteopenia and hyperemia following a fracture [8,13].
Radiological reporting factors
Reporting fractures in pediatrics can be confusing for the nonradiologists physicians or residents in the emergency department, the junior radiologists or the radiologists in training due to the unique different morphology of the immature skeleton including the presence of physis, the anatomical variations related to epiphyseal centers, and the radiologic features of some specific unique fractures in children. Radiologists experienced in pediatric imaging are familiar with pediatric orthopedic images. However, many factors can affect the inter-observership variations including the workload, time or shift of radiologic reporting, and distraction while reporting [15]. Therefore, following a thorough systematic assessment of the extremity radiograph in children can decrease incidence of missed fractures in children. Here are some of the practical tips:
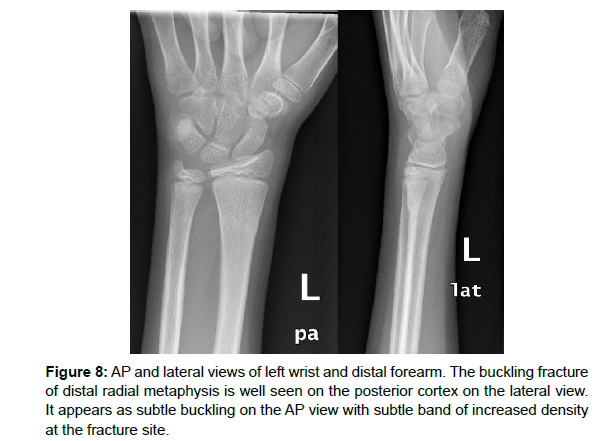
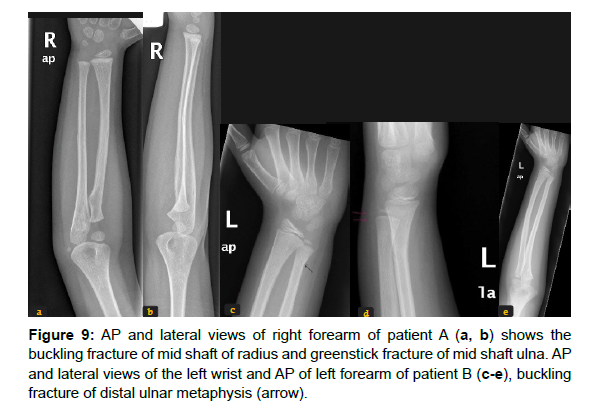
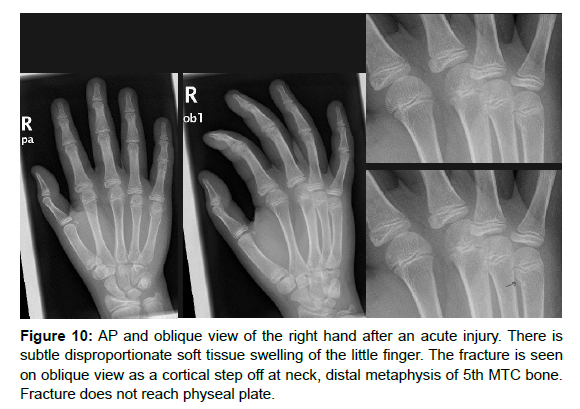
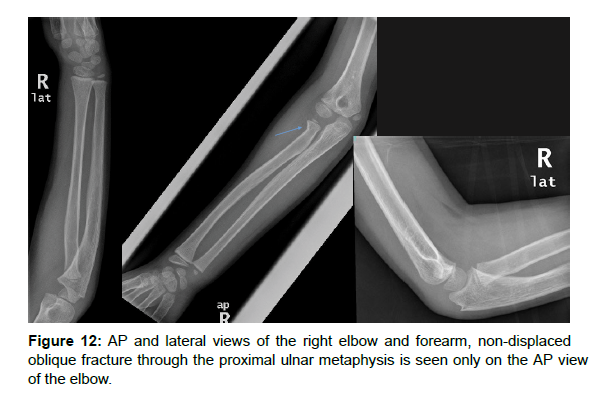
1. Following each bone individually is helpful when assessing hand or foot x-rays including passing the eye and even a finger on each part of the bones. This meticulous systematic assessment can help detect the focal buckling (Figure 1, 8), or a greenstick fracture, (Figure 9) or subtle cortical step-off injury, (Figures 10-12).
Figure 11: AP and oblique view of the left hand, the fracture is very subtle as horizontal radiolucent line through the proximal metaphysis of the proximal phalanx of the middle finger. Notice the helping signs of the soft tissue swelling at the base of left ring finger which is disproportionate to other digits. Fracture is not reaching the physeal plate.
2. Comparing, when possible, side to side and finger or toe of suspected fracture to others. The soft tissue assessment is a helpful tool to detect the site of injury. The injured digit or toe has generally associated soft tissue swelling, (Figure 11) [16]. Injury-associated soft tissue swelling manifest by displaced fat planes in the X-rays (Figure 9d).
3. Careful examination of the edges of the film, some of the foot fractures can be detected from an ankle X-ray, or a wrist bone fracture from a forearm X-ray.
4. Direct communication with the clinician can help solve the dilemma of an occult fracture and helps to request further radiographic views if the region of suspicion is masked or not imaged properly.
Conclusion
Occult fractures are frequently missed in adults and children. However, the unique immature skeletal structural anatomy and the normal variations contribute to the increased incidence of missing pediatric fractures. Cortical bone and periosteum characteristics may result in undisplaced and occult fractures, however, promote remodelling and healing process. Following a systematic radiologic assessment of bones combined with thorough knowledge of the unique fracture types in the pediatric population can decrease the incidence of missed fractures and prevents deformities or long-term malfunction.
References
- Gufler H, Schulze CG, Wagner S, Baumbach L (2013) MRI for occult physeal fracture detection in children and adolescents. Acta Radiol 54: 467-472.
- Kan JH, Estrada C, Hasan U, Bracikowski A, Shyr Y, et al. (2009) Management of occult fractures in the skeletally immature patient: cost analysis of implementing a limited trauma magnetic resonance imaging protocol. Pediatr Emerg Care 25: 226-230.
- Q Ma, Q Jiao, S Wang, L Dong, Y Wang, et al. (2020) Prevalence and Clinical Significance of Occult Fractures in the Extremities in Children. Front Pediatr 8: 393.
- Guly HR (2001) Diagnostic errors in an accident and emergency department. Emerg Med J 18: 263-269.
- Hallas P, Ellingsen T (2006) Errors in fracture diagnoses in the emergency department--characteristics of patients and diurnal variation. BMC Emerg Med 6: 4.
- Guermazi A, Tannoury C, Kompel AJ, Murakami AM, Ducarouge A, et al. (2022) Improving Radiographic Fracture Recognition Performance and Efficiency Using Artificial Intelligence. Radiology 302: 627-636.
- Fernholm R, Pukk Härenstam K, Wachtler C, Nilsson GH, Holzmann MJ, et al. (2019) Diagnostic errors reported in primary healthcare and emergency departments: A retrospective and descriptive cohort study of 4830 reported cases of preventable harm in Sweden. Eur J Gen Pract25: 128-135.
- Segal LS, Shrader MW (2013) Missed fractures in paediatric trauma patients. Acta Orthop Belg 79: 608-615.
- Schnitzler CM, Mesquita JM (2013) Cortical porosity in children is determined by age-dependent osteonal morphology. Bone 55: 476-486.
- Jacobsen FS (1997) Periosteum: its relation to pediatric fractures. J Pediatr Orthop B 6: 84-90.
- Choi C, Lee SJ, Choo HJ, Lee IS, Kim SK (2021) Avulsion injuries: an update on radiologic findings. Yeungnam Univ J Med 38: 289-307.
- Wahba G, Cheung K (2018) Pediatric hand injuries: Practical approach for primary care physicians. Can Fam Physician 64: 803-810.
- Swischuk LE, Hernandez JA (2004) Frequently missed fractures in children (value of comparative views). Emerg Radiol 11: 22-28.
- Zeng FTA, Fall M, Mbaye PA, Gueye D, Bisseyou AK, et al. (2022) Fractures of limbs specific to children: the experience of a Senegalese tertiary hospital. Egyptian Pediatric Association Gazette 70: 1-6.
- Mattijssen-Horstink L, Langeraar JJ, Mauritz GJ, Stappen Wvd, Baggelaar M, et al. (2020) Radiologic discrepancies in diagnosis of fractures in a Dutch teaching emergency department: a retrospective analysis. Scand J Trauma Resusc Emerg Med 28: 38.
- Minor M, Bui-Mansfield LT, Carra BJ (2015) Systematic Checklist Approach to the Radiographic Interpretation of the Injured Wrist to Avoid Common Diagnostic Errors. Contemp Diagn Radiol 38: 1-7.
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Citation: Tabban HA, Gani AHM, Ezeldin AM, El-Said E (2023) Fractures inChildren: Practical Approach to Reduce Missed Diagnosis. OMICS J Radiol 12:419. DOI: 10.4172/2167-7964.1000419
Copyright: © 2023 Tabban HA, et al. This is an open-access article distributedunder the terms of the Creative Commons Attribution License, which permitsunrestricted use, distribution, and reproduction in any medium, provided theoriginal author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2749
- [From(publication date): 0-2023 - Mar 29, 2025]
- Breakdown by view type
- HTML page views: 2356
- PDF downloads: 393