Case Report Open Access
Forefoot Osteolysis Revealing a Charcot Osteoarthropathy
Clara Bouche, Lucille Ratheau and Jean-François Gautier*Department of Endocrinology and Diabetes, Lariboisière Hospital, Assistance Publique des Hopitaux de Paris, France
- Corresponding Author:
- Jean-François Gautier
Department of Endocrinology and Diabetes
Lariboisière Hospital, Assistance Publique des Hopitaux de Paris, France
Tel: +330149959020
E-mail: jean-francois.gautier@aphp.fr
Received Date: April 13, 2016; Accepted Date: June 03, 2016; Published Date: June 10, 2016
Citation: Bouche C, Ratheau L, Gautier JF (2016) Forefoot Osteolysis Revealing a Charcot Osteoarthropathy. J Clin Diabetes Pract 1: 108.
Copyright: © 2016 Bouche C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at
Keywords
Osteoarthropathy; Antibiotherapy; Midfoot; Distal extremities
Introduction
Charcot osteoarthropathy, also known as Charcot foot or neuroarthropathy, has been recognised for over 130 years. Yet it remains a major cause of morbidity for patients with diabetes mellitus and a continuing challenge for physicians, as well as for public health because of the massive economic consequences of foot ulcers. Acute Charcot osteoarthropathy is a skeletal breakdown associated with inflammatory swelling of a foot in patients with pain insensitivity. Charcot osteoarthropathy can be classified into five different types, depending on the anatomical site involved: forefoot, tarsometatarsal joints, Chopart joint, ankle or calcaneus [1]. Midfoot Charcot osteoarthropathy is the most common form (more than 80%), and is in general easily recognized with the classic rocker-bottom subluxation of the midfoot [1]. On the opposite, forefoot Charcot osteoarthropathy is less well known and is probably underdiagnosed as the external deformities are minimal.
Case Report
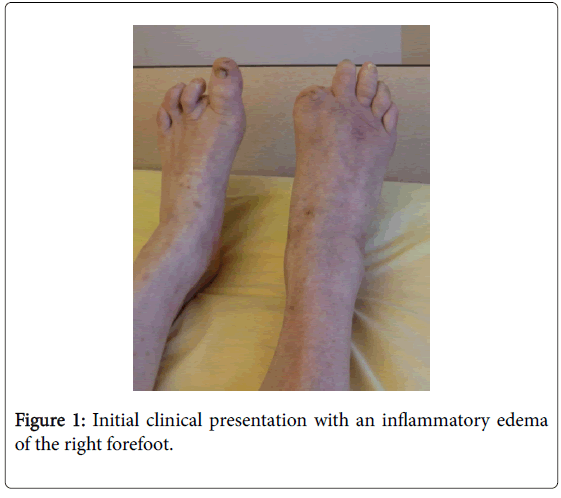
We report the case of a 58 year-old woman with a 23-year history of type 1 diabetes. She presented to our clinic with an inflammatory edema of the right forefoot (Figure 1), occurring three months after a partial first ray amputation for osteomyelitis.
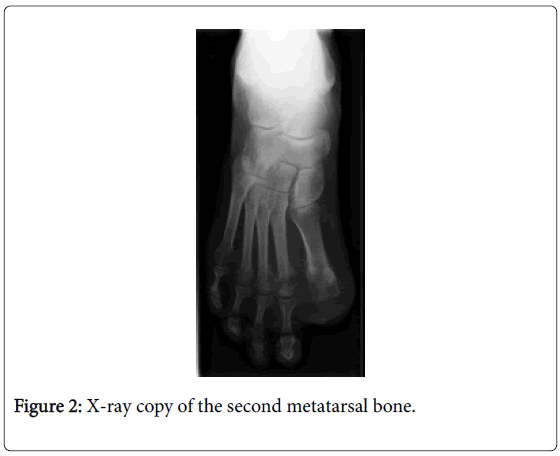
Diabetes was already complicated by a laser-treated proliferative retinopathy and a second ray amputation of the left foot due to osteomyelitis secondary to a skin ulcer. X-rays showed a destruction of the two first metatarsal heads of the right foot (Figure 2).
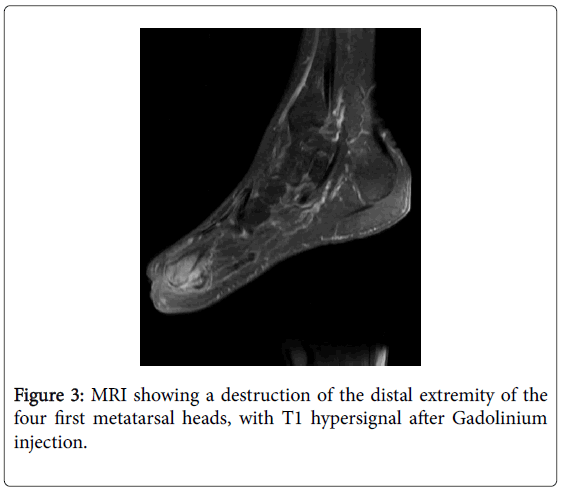
MRI showed a destruction of the distal extremity of the first four metatarsal heads, associated with a T1 hyposignal, T2 hypersignal and T1 hypersignal after Gadolinium injection without cellulitis or abscess (Figure 3).
All radiological exams were compatible with the diagnosis of osteomyelitis of the forefoot, especially in the context of a recent osteomyelitis of the first toe. However, we were surprised by the good healing of the amputation wound, the absence of a clinical infectious syndrome and the lack of biochemical inflammation markers. We put forward the hypothesis of a Charcot neuropathic osteoarthropathy, and prescribed the classical treatment by immobilization, without antibiotics. As an alternative to the total contact cast, we used an offloading device called the prefabricated pneumatic walking brace. After 2 months, clinical and standard radiographs reflected consolidation. The immobilization device was abandoned and footwear was prescribed.
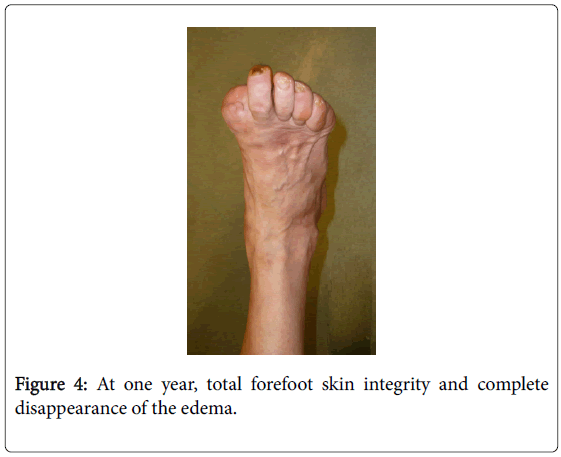
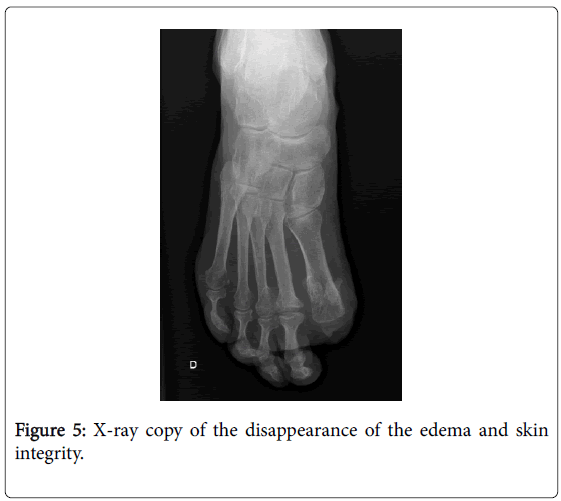
At one year, the diagnosis of Charcot neuropathic osteoarthropathy was confirmed since we observed skin integrity with a complete disappearance of the edema (Figure 4), and X-Ray consolidation (Figure 5).
Discussion
Charcot osteoarthropathy directly leads to foot deformity with subsequently lower extremity complications such as ulcers and infections and may ultimately lead to lower extremity amputation if not identified and managed appropriately. Forefoot Charcot osteoarthropathy can be easily misdiagnosed due to the minimal deformity of the foot. Moreover this entity is less frequent than the classical midfoot form, frequently ignored by physicians.
Distinguishing osteomyelitis from Charcot osteoarthropathy can be challenging. 50 percent of the patients remember a precipitating minor traumatic event, such as an ankle sprain or a previous foot procedure. In the present case report, the patient had a partial first ray amputation. As in our case, Charcot osteoarthropathy can be suspected because of the absence of infectious sign. MRI may be useful and usually finds, as in this case, an isolated T2 hypersignal and postcontrast T1 bone marrow enhancement, without contiguous foci of skin disruption, cellulitis, abscess or sinus tract [2,3]. Treatment of Charcot osteoarthropathy implies to reduce weigh bearing in order to reduce the risk of complex cortical bone fractures and subsequent disability [1,3]. Different devices are allowed, and a prefabricated pneumatic walking brace can be used in patient without severe foot deformity [3]. Charcot osteoarthropathy localized to the forefoot may heal faster than other forms, and the average time of healing was reported to be 55 ± 17 (SD) days [4] in one publication, similarly to the presented case.
In the present case report, the diagnosis was confirmed by the healing after appropriate immobilization, without use of antibiotics. Charcot osteoarthropathy is commonly located at the midfoot. Physicians should be aware that it may also affect the forefoot in order to avoid unnecessary hospitalizations, antibiotherapy and amputation.
References
- Hartemann-Heurtier A, Van GH, Grimaldi A (2002) The Charcot foot. Lancet 360: 1776-1779.
- Ergen FB, Sanverdi SE, Oznur A (2013) Charcot foot in diabetes and an update on imaging. Diabet Foot Ankle 4: 21884.
- Sommer TC, Lee TH (2001) Charcot foot: the diagnostic dilemma. Am Fam Physician 64: 1591-1598.
- Sinacore DR (1998) Acute Charcot arthropathy in patients with diabetes mellitus: healing times by foot location. J Diabetes Complications 12: 287-293.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 17137
- [From(publication date):
September-2016 - Jul 06, 2025] - Breakdown by view type
- HTML page views : 16387
- PDF downloads : 750