Review Article Open Access
Flutter Device Review: Effects on Secretion and Pulmonary Function
Ada Clarice Gastaldi*
Physiotherapy Course, Ribeirão Preto Medical School, University of São Paulo, Brazil
- *Corresponding Author:
- Ada Clarice Gastaldi
Professor of the Physiotherapy Course
Ribeirão Preto Medical School, University of São Paulo, Brazil
Tel: 14049- 900
E-mail: ada@fmrp.usp.br
Received date: March 14, 2016; Accepted date: May 16, 2016; Published date: May 25, 2016
Citation: Gastaldi AC (2016) Flutter Device Review: Effects on Secretion and Pulmonary Function. J Nov Physiother 6:292. doi:10.4172/2165-7025.1000292
Copyright: © 2016 Gastaldi AC. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
The flutter is a respiratory device that produces an oscillatory positive expiratory pressure that can be used as an alternative for removal of secretions. The effects of flutter have been studied in patients with different diseases, using different protocols and outcomes, and its effects on secretions and pulmonary function are not well established. In this review, we present the results from studies that have used flutter as a physical therapy intervention compared with a control or sham group or compared to other physical therapy techniques. The device has demonstrated its beneficial effect on removal of secretions increasing the volume of expectoration and a decrease in the viscosity of secretions, increasing in vitro transport of secretions from cystic fibrosis and bronchiectasis patients. The effects of flutter on pulmonary function are controversial with no changes or improvement in some studies, and some possible negative effects that could be associated with the flow dependent mechanism. The airways resistance or respiratory resistance were not changed in some studies and the only one that showed a decrease in the respiratory system resistance studied patients with large amounts of secretions. In conclusion, the flutter can decrease the viscoelasticity of respiratory secretions favouring the secretions transport and elimination, which can be used for stable patients or during exacerbation. The effects in the pulmonary function / mechanics needs to be better investigated.
Keywords
Flutter device; Physical therapy modalities; Intrathoracic oscillation; Chest physical therapy; Pulmonary function
Abreviations
COPD: Chronic Obstructive Pulmonary Disease; PEP: Positive Expiratory Pressure; CF: Cystic Fibrosis; Log G*: Mucus Impedance; MCI: Mucociliary Clearance Index; CCI: Cough Clearance Index; PDPV: Postural Drainage, Percussion, and Vibration; IPV: Intrapulmonary Percussive Ventilation; ACBT: Active Cycle Breathing Technique; HFCWC: High Frequency Chest Wall Compression; ELTGOL: Slow Expiration With Glottis Opened in Infralateral Decubitus Position; VC: Vital Capacity; FEV1: Forced Expiratory Volume in 1 Second; PEF: Peak Expiratory Flow; FVC: Forced Vital Capacity; RV: Residual Volume; FEF: Forced Expiratory Flow; TLC: Total Lung Capacity; FET: Forced Expiration Technique; HAT: Hydro Acoustic Therapy; AD: Autogenic Drainage; PDP: Postural Drainage And Percussion; Raw: Airway Resistance; R5: Respiratory System Resistance at 5 Hz; X5: Respiratory System Reactance at 5 Hz; Fres: Resonant Frequency
Introduction
The physical therapy can contribute to prevent or treat complications arising from the retention of secretion in patients with hipersecretory chronic diseases or during exacerbations. Different physical therapy techniques can help patients patients that are not able to produce enough expiratory flow or because they have too much secretions or because their secretions are too thick [1-3].
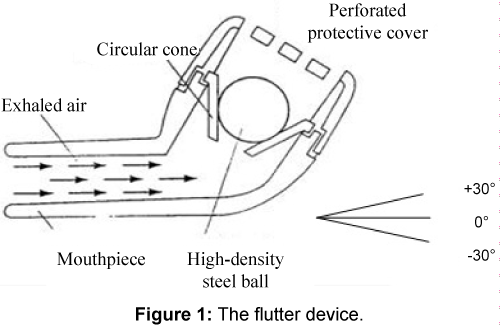
The flutter is a respiratory device that can be used as an alternative for removal of secretions proposed by Lindeman [4]. It is a simple and small plastic device shaped like a pipe, with a mouthpiece at one end and a perforated cover at the other end and with a stainless steel ball resting in a plastic cone inside (Figure 1). During the expiration through the flutter, the expiratory flow causes the steel ball up and down movement, creating an oscillatory positive expiratory pressure (PEP) with a back transmission to the patient. This device is a combination of two different techniques: PEP and oscillations [4-6].
The PEP helps the removal of secretions by increasing the alveolar pressure due to expiration against resistance producing a positive pressure which helps hold airways open and may reducing peripheral airway resistance. The oscillations produce a thixotropic effect, which is a decrease in the viscoelasticity of secretions when subjected to a constant vibration [4-7].
The effects of flutter have been studied in patients with cystic fibrosis, chronic obstructive pulmonary disease (COPD), bronchiectasis, and others, using different protocols and outcomes, in children and adult patients, and its effects on secretions and pulmonary function are not well established. The objective of this paper was to review the effects on respiratory secretions and pulmonary function.
Methods
Electronic literature searches for articles published between 1992 and 2015 were conducting using PubMed, ScienceDirect, PEDro (Physiotherapy Evidence Database), and Scielo databases. The search terms used were flutter VRP1, flutter valve, flutter desitin, intrathoracic oscillation, oscillating positive pressure, and oscillating positive expiratory pressure.
The search included articles in English or with English abstract that have investigated the flutter device. There were no exclusions on the basis of age, gender or physiological status. All reviews and study protocols were excluded.
Mechanical principles
The generation of oscillation and pressure are dependent on the expiratory flow and gravity forces. The neutral position (or zero degrees) is considered the one which the device has an angle of 90 degrees with the head position, i.e., parallel to the ground. In general, with the device turned upward (positive degrees) there is an increase in the pressure and oscillation, and with the device turned downward (negative degrees), pressure and oscillation decrease 4 (Figure 1).
The flutter was studied by Lindemann [4] using the angles of -30, 0, and + 30° and flows ranging from 1.6 to 5.5 L/s, which produced 8 to 75 cm H2O of pressure range, and oscillation frequency of 2 to 32 Hz. These angles were later used by other authors who reproduced similar results for comparable flows [4,8-12].
For low flow rates (30-65 L/min), the sphere moves in the horizontal and vertical directions, touching the conical wall and vibrating. For airflow rates higher than 100 L/min, the sphere movement is basically vertical, suggesting the use of the flutter device during normal (not forced) expiration [9,10].
Brooks et al. [13] increased the number of angles and studied the device at -40, -30, -20, 0, +20, +30 e +40°, while Volsko et al. [14] partially reproduced positive angles of 0, 20 and 40°. The results of Brooks et al. [13] also show a similar behavior to that was described by Lindemann [4], which means a decrease in PEP and oscillation frequency with negative angles and increased with positive angles. They recommended special attention to PEP values above 20 cm H2O that could be obtained at angles of zero and positive, which can be detrimental in susceptible patients.
Among the clinical trials, the pressure and oscillation variation were registered during the breathing exercises by some authors. They described a pressure varying from 6 to 25 cm H2O [15-23], whereas oscillation variation has been mentioned only in McIlwaine’s study [19], ranging 8-26 Hz.
Effects on removal of secretions
The effect of breathing exercises with flutter on the volume of expectorated secretions was evaluated in 19 studies, in stable patients with cystic fibrosis (CF), chronic obstructive pulmonary disease (COPD), bronchiectasis and panbronchiolitis, and in hospitalized patients with CF and chronic bronchitis. These studies are in Table 1 and their results suggest that the device is effective for removal of secretions.
| Compared with a control group | |
|---|---|
| ↑ With flutter | [24-28] |
| Compared with other physiotherapy techniques | |
| Both ↑ | Newhouse et al. [17] ; Lindeman et al.[24]; [29-31] |
| Greaterwith flutter | Orlik et al. [18]; Konstan et al.[15]; [32-35] |
| Greaterwithother techniques | [36-38] |
Table 1: Effects of flutter on the volume of sputum.
In five of these studies the flutter was compared with a control or sham group and their results showed a higher volume of expectorated secretion after flutter [24-31].
Other studies compared flutter with other (s) technique (s) of physical therapy. In six of these studies, the volume of sputum secretion after flutter was greater after flutter than with other techniques [14,15,18,32-35]; in four studies the volume were similar [4,17,29,30]; and in three, the sputum volume was higher with the other physical therapy technique [36-38] (Table 1).
However, the effects on secretions can also be related to the effect of the oscillations on the physical properties, i.e., the tixothropic effect that means a decrease in the viscosity when the mucus is submitted to an oscillation and/or flow.
The use of oscillations was based on the mechanism that was first demonstrated in dogs that were submitted to oral and thoracic vibration, showing that the best transport of their respiratory secretion was obtained at frequencies of oscillation between 13 and 15 Hz [39,40].
The acute effect of flutter oscillations on viscoelastic properties of respiratory mucus was demonstrated in secretions from patients with cystic fibrosis and bronchiectasis, in studies without a control group and after one single session. After 30 minutes of oscillation there was a decrease in the log G* that is a measure of the total impedance of mucus samples [41] and a decrease in the mucus viscosity [22], besides no change in the ciliary and cough transport [42].
Another studies have evaluated the flutter effects after four weeks of treatment, using one or two 30 minutes sessions per day. App et al. [30] demonstrated an increase in the mucociliary and cough clearance indexes in cystic fibrosis patients, while Tambascio et al. [43] demonstrated an increase in the cough transport and contact angle measurements that can be related with a change in the rheological and surface properties in patients with bronchiectasis. These studies are detailed in the Table 2.
| Acute effects | ||||
|---|---|---|---|---|
| Dasgupta et al. [41] | CF secretions | n=19 | 30 min | ↓ log G* |
| Valente et al. [42] | bronchiectasis | n=8 | 20 and 40 min | transport not changed |
| Ramos et al. [22] | bronchiectasis | n=15 | 20 min | ↓ viscosity |
| Effects after 4 weeks of using | ||||
| App et al. [30] | CF | n=14 | 2 x 30 min/day | ↑ MCI and CCI |
| Tambascio et al.[43] | bronchiectasis | n=18 | 30 min/day | ↑ cough transport ↓ contact angle |
CF: Cystic Fibrosis; Log G*: Mucus Impedance; MCI: Mucociliary Clearance Index; CCI: Cough Clearance Index
Table 2: Effects of flutter on the physical properties of sputum.
Effects on pulmonary function
The beneficial effects of flutter exercises on pulmonary function have been studies in clinical trial and crossover studies, in adults and children, and their results are controversial and not well established yet. Fourteen studies, comparing flutter with a control or sham group, or other techniques have presented positive effects on pulmonary function, with an increase in the slow and forced vital capacity and pulmonary flows and a decrease in the residual volume, functional residual capacity and total lung capacity, in patients with cystic fibrosis, COPD and others. In two studies flutter was used with a medication improving the bronchodilator response [16-18,20,24,27,33,44-50] (Table 3).
| Author | Disease | n | age (years) |
Comparison group | Protocol | Results |
|---|---|---|---|---|---|---|
| Cegla et al.[24] | COPD | 51 | 53 | control | 2 weeks 3x, 5min |
↑ VC, ↑ FEV1,↑ PEF |
| Girard et al.[44] | asthma | 18 | 43 | - | 45 days 3x, 5min |
↑ FVC, ↑ FEV1,↑ PEF |
| Weiner et al.[45] | COPD | 20 | sham | 3 months | ↑ VC | |
| Jones et al.[16] | thoracic restriction | 30 | 18-24 | breathing exercises | 1 session 15min |
restore FVC |
| Homnik et al.[46] | CF hospitalized | 16 | 16,1 | PDPV | 9 days 15min/30min |
↑ FVC, ↑ FEV1, ↓ RV |
| Burioka et al.[33] | panbronchiolitis | 8 | 56,1 | cough | 1 week 4x/day, 5min |
↑ PEF |
| Newhouse et al.[17] | CF | 8 | 17 | IPV | 1 session 20min |
↑ FVC |
| Gondor et al. [47] | CF hospitalized | 8 | 11,9 | PDPV | 2 weeks | ↑ FVC, ↑ FEV1, ↑FEF25-75 |
| Orlik and Sands,[18] | CF | 80 | 11,44 | PDP x PDPV x ACBT | 7 months 3x/day |
↑ FVC, ↑ FEV1 |
| Wolkove et al.[20] | severe COPD | 23 | 71,7 | sham | 1 session 10min |
↑ FEV1 (>effect of bronchodilator) |
| Wolkove et al.[48] | COPD | 15 | 71±10 | sham | 1 week | ↑ FVC, ↑ FEV1 (>effect of bronchodilator) |
| Wang et al.[49] | >85 years | 60 | 87,2 | control | 28 days | ↑ FVC, ↑ FEV1 |
| Sontag et al.[50] | CF | 16 | 14,6 | PDP x HFCWO | 3 years 2x/day 20-40min |
<decline rate FEF25-75 |
| Guimarães et al.[27] | bronchiectasis | 10 | 55,9 | control x ELTGOL | 1 session 15min |
↓ RV, ↓ FRC, ↓ TLC |
COPD: Chronic Obstructive Pulmonary Disease; CF: Cystic Fibrosis; PDPV: Postural Drainage, Percussion, and Vibration; IPV: Intrapulmonary Percussive Ventilation; ACBT: Active Cycle Breathing Technique; HFCWC: High Frequency Chest Wall Compression; ELTGOL: Slow Expiration with Glottis Opened in Infralateral Decubitus Position; VC: Vital Capacity; FEV1: Forced Expiratory Volume in 1 Second; PEF: Peak Expiratory Flow; FVC: Forced Vital Capacity; RV: Residual Volume; FEF: Forced Expiratory Flow; TLC: Total Lung Capacity.
Table 3: Positive effects of flutter on pulmonary function.
However, other 15 studies with similar designs, have showed no change in the pulmonary function [15,18,21,25,29-32,34-36,51-53] (Table 4).
| Author | Disease | n | age (years) | Comparison group | Protocol | Results |
|---|---|---|---|---|---|---|
| Swiftet al.[51] | asthma | 20 | control | 2 week | PEF | |
| Pryoret al.[36] | CF | 20 | 16-36 | ACBT | 1 session 20min |
FVC, FEV1 |
| Konstanet al.[15] | CF | 18 | 22 | cough | 2 sessions 15min |
FVC |
| Ambrosinoet al.[32] | COPD and bronchiectasis | 14 | 65±16 | PDP | 2 sessions 30min |
FVC, FEV1, PEF |
| Nakamuraet al.[25] | hypersecretive | 17 | control | 3 days 15min |
PEF | |
| Ceglaet al.[52] | COPD | 90 | 57 | control | 1 week | FVC, FEV1, RV |
| van Windenet al.[29] | CF | 22 | 7-17 | PEP + FET | 2 weeks 2x/day 5x15br |
FVC, FEV1 |
| Appet al.[30] | CF | 14 | 19,6 | AD | 4 weeks 2x/day 30min |
FVC, FEV1 |
| Padmanet al.[53] | CF | 15 | 5-17 | PDP | 1 month 3x/day 15min |
FVC, FEV1, FEF25-75 |
| Belloneet al.[34] | chronic bronchitis hospitalized | 10 | 57,5 | ELTGOL x DP | 1 session 30min |
FVC, FEV1 |
| Orlik and Sands[18] | CF hospitalized | 21 | 5-18 | PDP x PDPV x ACBT | - | PEF |
| Oermanet al. [54] | CF | 24 | 23±9,4 | HFCWO | 4 weeks 2-3x/day 20min |
FVC, FEV1 |
| Thompsonet al. [35] | bronchiectasis | 17 | 59 | ACBT | 4 weeks | FVC, FEV1 |
| Lagerkvistet al. [21] | CF | 15 | 12,5±5,1 | PEP | 8 weeks 3x/day 2min |
FVC, FEV1 |
| Gastaldiet al. [28] | COPD | 15 | 67.3±9.1 | sham | 1 session | FVC, FEV1 |
CF: Cystic Fibrosis; COPD: Chronic Obstructive Pulmonary Disease; ACBT: Active Cycle Breathing Technique; PDPV: Postural Drainage, Percussion, and Vibration; PEP: Positive Expiratory Pressure; Forced Expiration Technique; AD: Autogenic Drainage; ELTGOL: Slow Expiration With Glottis Opened in Infralateral Decubitus Position; HFCWC: High Frequency Chest Wall Compression; Br: Breath; PEF: Peak Expiratory Flow; FVC: Forced Vital Capacity; FEV1: Forced Expiratory Volume in 1 Second; RV: Residual Volume; FEF: Forced Expiratory Flow.
Table 4: Studies with no change in pulmonary function results with flutter.
And two other studies in cystic fibrosis patients showed a decrease in pulmonary function. Both have used the flutter exercises twice a day, one for one week and another one with year of follow-up [19,26].
Some studies have been used airway or respiratory system resistance to evaluate the effects produced by the flutter exercises. In three of them there were no changes in the airways resistance by body plethismograph in patients with cystic fibrosis and COPD [29,52-54]. It needs to be noted that one of these studies have included 90 patients to a flutter or control group [52].
Three studies using the impulse oscillometry system (IOS) showed different results. In the study of Veiga et al. [55] there was no change in the resistance at 5 Hz (R5) after 15 minutes of flutter. On the other hand, two crossover studies comparing flutter with a control group have improved the respiratory system resistance. Figueiredo et al. [56] have demonstrated a decrease in the R5 after 15 minutes of flutter in bronchiectasis patients with a large amount of secretions while Gastaldi et al. [28] have obtained a decrease in the resistance, reactance and resonant frequency after 30 minutes of flutter in COPD patients with small amount of secretions (Table 5).
| Author, year | Disease | n | Comparison group | Duration | Results |
|---|---|---|---|---|---|
| Ceglaet al.[52] | COPD | 90 | control | 1 week | Raw (no change) |
| van Windenet al.[29] | CF | 22 | PEP + FET | 2 weeks | Raw (no change) |
| Padmanet al.[53] | CF | 15 | PDP | 1 month | Raw (no change) |
| Veigaet al.[55] | COPD, asthma and bronchiectasis | 39 | - | 1 session | R5 (no change) |
| Figueiredoet al.[56] | bronchiectasis | 8 | sham | 1 session | ↓ R5 |
| Gastaldiet al.[28] | COPD | 15 | sham | 1 session | ↓ R5, ↓ X5, ↓ Fres |
COPD: Chronic Obstructive Pulmonary Disease; CF: Cystic Fibrosis; PEP: Positive Expiratory Pressure; FET: Forced Expiration Technique; PDP: Postural Drainage and Percussion, Raw: Airway Resistance; R5: Respiratory System Resistance At 5 Hz; X5: Respiratory System Reactance At 5 Hz; Fres: Ressonat Frequency.
Table 5: Effects of flutter on airway and respiratory system resistance.
Discussion
The flutter device produces pressure and oscillation that can help the removal of secretions. This oscillatory pressure is dependent on the patient’s expiratory flow as well as the position of the device. According to the mechanical studies, the patient can, using normal (not forced) expiration, produce pressures up to 25 cm H2O and oscillation range between 10 and 20 Hz [4,8-12], but there is not enough information in the papers included in this review about instructions to the patients or patient’s performance.
The flutter device has been studied in clinical trials and crossover studies, ranging from one single session to 3 years of follow-up. It is interesting to note that, among the selected studies in this review, only 11 have compared the flutter with a control or sham group [20,24-28,40,45,48,51,52], and only four have studied hospitalized patients [18,34,46,47].
The device has demonstrated its beneficial effect on removal of secretions increasing the volume of expectoration when compared with a control group or with another physical therapy technique or device for removal of secretions [4,15,17,18,24-35]. Some studies have used the flutter time ranging from five to 30 minutes or five times of 15 breaths, suggesting that the effect on the volume of secretions was not related with the therapy time.
However, it is important to discuss if the volume of expectoration is a good outcome to express the secretion clearance. Besides the flutter device objective is to favour the clearance of secretions, there are some studies that did not evaluate the volume of expectoration probably because the volume may not be a precise or reliable measurement. Some patients can move the secretions from the lungs and swallow, and some others can expectorate pulmonary secretions with saliva, which can increase the expectoration volume. It is possible to minimize this confounding factor using the dry weight, or dry/wet ratio, but, with dry secretions, it is possible to become similar secretions with different densities.
Another effect on secretions is the thixotropic effect that was speculated by some authors and was demonstrated for secretions from cystic fibrosis and bronchiectasis patients. This effect is related with the produced oscillations but the mechanisms remain unclear [39,40].
Dasgupta [41] and Ramos [22] have demonstrated the acute effects of the flutter device decreasing the rigidity and viscosity of secretions, while Valente [42] observed no change in the in vitro secretion transport. App [30] and Tambascio [43] have demonstrated beneficial effects after four weeks of treatment in patients with cystic fibrosis and bronchiectasis. There was a decrease in the rigidity and an increase in the calculated ciliary and cough transport index and the measured in vitro cough transport. These effects were studied in adult patients and the changes in the physical properties of secretions were obtained only with 30 minutes of flutter exercises.
The effects of flutter on pulmonary function are controversial and the differences among the results could be related with different flows and positions that were not controlled during the studies. It is important to note that the device has a flow dependent resistance, which means a decrease in the resistance as the flow decreases.
Some studies have demonstrated an acute improvement in the pulmonary function but it is necessary to question some important points. Among the 14 studies with positive results [16-18,20,27,33,44-50], there are four studies that have used the flutter in one single session [16,17,20,27] and the improvement in pulmonary function after one single session can be related to the removal of secretions or to the airways opening effect.
In fact, we do not know what changes in pulmonary function would be expected when you move secretions from the peripheral to central airways. When the patients can move and expectorate secretions the pulmonary function can increase, but if the patient moves the secretions inside the airways with a late expectoration, he/she can experience a transitory decrease in the pulmonary function.
The long-term effects needs to be better defined. It needs to be noted that there was a higher decrease in the FVC, FEV [1], and FEF [25-55] after one year [19] but there was a smaller decline rate FEF [25-55] after three years of follow up [50].
Nevertheless, it is possible to use more sensitive methods to evaluate the pulmonary function. The airways resistance was not changed in some studies [29,52,53,55] and there are two studies that showed a decrease in the respiratory system resistance in bronchiectasis and COPD patients, one with large amounts of secretions (50 mL/day) [56] and the other with a small amount of secretions [28]. Additionally, among the studies that presented beneficial effects on respiratory secretions, some of them have showed no changes in pulmonary function [15,18,25,29,30,32,34]. For future protocols, it is important to know if the effects can be related to the amount of secretions, to the protocols of use, or to the sensitivity of the outcomes.
Conclusion
The flutter can decrease the viscoelasticity of respiratory secretions favouring the secretions transport and elimination, which can be used for stable patients or during exacerbation, in children and adults. Because it can be as good as other physiotherapy techniques for removal of secretions, the clinicians can be guided by the better ratio preference and effectiveness.
It is important to know the mechanisms that are involved in the decrease of secretions viscosity and the effects in the pulmonary function / mechanics needs to be better investigated, as well as whose patients can have beneficial effects using the flutter device for short and long term.
Competing Interests
There are not funding in the paper. The author declares no relevant conflicts of interest.
References
- Mackenzie D, Frith PA, Burdon JGW, Town GI, Australian Lung Foundation, et al. (2003) The COPDX Plan: Australian and New Zealand Guidelines for the management of Chronic Obstructive Pulmonary Disease. Med J Aust 178: S7-S39.
- Main E, Prasad A, Schans C (2005) Conventional chest physiotherapy compared to other airway clearance techniques for cystic fibrosis. Cochrane Database Syst Rev 25: CD002011.
- Langer D, Hendriks E, Burtin C, Probst V, van der Schans C, et al. (2009) A clinical practice guideline for physiotherapists treating patients with chronic obstructive pulmonary disease based on a systematic review of available evidence. Clin Rehabil 23: 445-462.
- Lindemann H (1992) [The value of physical therapy with VRP 1-Desitin ("Flutter")]. Pneumologie 46: 626-630.
- Chatburn RL (2007) High-frequency assisted airway clearance. Respir Care 52: 1224-1235.
- Bhowmik A, Chahal K, Austin G, Chakravorty I (2009) Improving mucociliary clearance in chronic obstructive pulmonary disease. Respir Med 103: 496-502.
- Zayas G, Dimitry J, Zayas A, O'Brien D, King M (2005) A new paradigm in respiratory hygiene: increasing the cohesivity of airway secretions to improve cough interaction and reduce aerosol dispersion. BMC Pulm Med 5: 1-12.
- Cegla UH (2000) Physiotherapy with oscillating PEP systems (RC-Cornet, VRP1) in COPD. Pneumologie 54: 440-446.
- Lepore Neto FP, Lima LC, Gastaldi AC (2000) Dynamic evaluation of a new device for respiratory physiotherapy. Rev Cenciae Engenharia 9: 62-68.
- de Lima LC, Duarte JB, Lépore Neto FP, Abe PT, Gastaldi AC (2005) Mechanical evaluation of a respiratory device. Med Eng Phys 27: 181-187.
- Alves LA, Pitta F, Brunetto AF (2008) Performance analysis of the Flutter VRP1 under different flows and angles. Respir Care 53: 316-323.
- dos Santos AP, Guimarães RC, de Carvalho EM, Gastaldi AC (2013) Mechanical behaviors of Flutter VRP1, Shaker, and Acapella devices. Respir Care 58: 298-304.
- Brooks D, Newbold E, Kozar LF, Rivera M (2002) The flutter device and expiratory pressures. J Cardiopulm Rehabil 22: 53-57.
- Volsko TA, DiFiore J, Chatburn RL (2003) Performance comparison of two oscillating positive expiratory pressure devices: Acapella versus Flutter. Respir Care 48: 124-130.
- Konstan MW, Stern RC, Doershuk CF (1994) Efficacy of the Flutter device for airway mucus clearance in patients with cystic fibrosis. J Pediatr 124: 689-693.
- Jones A, Tse E, Cheung L, To C, Lo C (1997) Restoration of lung volume using the Flutter VRP1 or breathing exercise. Aust J Physiother 43: 183-189.
- Newhouse PA, White F, Marks JH, Homnick DN (1998) The intrapulmonary percussive ventilator and flutter device compared to standard chest physiotherapy in patients with cystic fibrosis. Clin Pediatr (Phila) 37: 427-432.
- Orlik T, Sands D (2001) Long-term evaluation of effectiveness for selected chest physiotherapy methods used in the treatment of cystic fibrosis. Med Wieku Rozwoj 5: 245-257.
- McIlwaine PM, Wong LT, Peacock D, Davidson AG (2001) Long-term comparative trial of positive expiratory pressure versus oscillating positive expiratory pressure (flutter) physiotherapy in the treatment of cystic fibrosis. J Pediatr 138: 845-850.
- Wolkove N, Kamel H, Rotaple M, Baltzan MA Jr (2002) Use of a mucus clearance device enhances the bronchodilator response in patients with stable COPD. Chest 121: 702-707.
- Lagerkvist AL, Sten GM, Redfors SB, Lindblad AG, Hjalmarson O (2006) Immediate changes in blood-gas tensions during chest physiotherapy with positive expiratory pressure and oscillating positive expiratory pressure in patients with cystic fibrosis. Respir Care 51: 1154-1161.
- Ramos EM, Ramos D, Iyomasa DM, Moreira GL, Melegati KC, et al. (2009) Influence that oscillating positive expiratory pressure using predetermined expiratory pressures has on the viscosity and transportability of sputum in patients with bronchiectasis. J Bras Pneumol 35: 1190-1197.
- Chicayban LM, Zin WA, Guimaraes FS (2011) Can the Flutter Valve improve respiratory mechanics and sputum production in mechanically ventilated patients? A randomized crossover trial. Heart Lung 40: 545-553.
- Cegla UH, Retzow A (1993) Physical therapy with VRP1 in chronic obstructive respiratory tract diseases-results of a multicenter comparative study. Pneumologie 47: 636-639.
- Nakamura S, Kawakami M (1996) Acute effect of use of the Flutter on expectoration of sputum in patients with chronic respiratory diseases. Nihon Kyobu Shikkan Gakkai Zasshi 34: 180-185.
- Jarad NA, Powell T, Smith E (2010) Evaluation of a novel sputum clearance technique--hydro-acoustic therapy (HAT) in adult patients with cystic fibrosis: a feasibility study. Chron Respir Dis 7: 217-227.
- Guimaraes FS, Moco VJ, Menezes SL, Dias CM, Salles RE, et al. (2012) Effects of ELTGOL and Flutter VRP1® on the dynamic and static pulmonary volumes and on the secretion clearance of patients with bronchiectasis. Rev Bras Fisioter 16: 108-113.
- Gastaldi AC, Paredi P, Talwar A, Meah S, Barnes PJ, et al. (2015) Oscillating Positive Expiratory Pressure on Respiratory Resistance in Chronic Obstructive Pulmonary Disease with a small amount of secretion: A Randomized Clinical Trial. Medicine (Baltimore) 94: e1845.
- van Winden CM, Visser A, Hop W, Sterk PJ, Beckers S, et al. (1998) Effects of flutter and PEP mask physiotherapy on symptoms and lung function in children with cystic fibrosis. Eur Respir J 12: 143-147.
- App EM, Kieselmann R, Reinhardt D, Lindemann H, Dasgupta B, et al. (1998) Sputum rheology changes in cystic fibrosis lung disease following two different types of physiotherapy: flutter vs autogenic drainage. Chest 114: 171-177.
- Orlik T (2000) Evaluation of the efficiency of selected thoracic physiotherapy methods used in the treatment of patients with cystic fibrosis. Med Wieku Rozwoj 4: 233-246.
- Ambrosino N, Callegari G, Galloni C, Brega S, Pinna G (1995) Clinical evaluation of oscillating positive expiratory pressure for enhancing expectoration in diseases other than cystic fibrosis. Monaldi Arch Chest Dis 50: 269-275.
- Burioka N, Sugimoto Y, Suyama H, Hori S, Chikumi H, et al. (1998) Clinical efficacy of the FLUTTER device for airway mucus clearance in patients with diffuse panbronchiolitis. Respirology 3: 183-186.
- Bellone A, Lascioli R, Raschi S, Guzzi L, Adone R (2000) Chest physical therapy in patients with acute exacerbation of chronic bronchitis: effectiveness of three methods. Arch Phys Med Rehabil 81: 558-560.
- Thompson CS, Harrison S, Ashley J, Day K, Smith DL (2002) Randomized crossover study of the flutter duvice and the active cycle of breathing technique in non-cystic fibrosis bronchiectasis. Thorax 57: 446-448.
- Pryor JA, Webber BA, Hodson ME, Warner JO (1994) The Flutter VRP1 as an adjunct to chest physiotherapy in cystic fibrosis. Respir Med 88: 677-681.
- Eaton T, Young P, Zeng I, Kolbe J (2007) A randomized evaluation of the acute efficacy, acceptability and tolerability of flutter and active cycle of breathing with and without postural drainage in non-cystic fibrosis bronchiectasis. Chron Respir Dis 4: 23-30.
- Borka P, Gyurkovits K, Bódis J (2012) Comparative study of PEP mask and Flutter on expectoration in cystic fibrosis patients. Acta Physiol Hung 99: 324-331.
- King M, Phillips DM, Gross D, Vartian V, Chang HK, et al. (1983) Enhanced tracheal mucus clearance with high frequency chest wall compression. Am Rev Respir Dis. 128: 511-515.
- King M, Phillips DM, Zidulka A, Chang HK (1984) Tracheal mucus clearance in high-frequency oscillation. II: Chest wall versus mouth oscillation. Am Rev Respir Dis 130: 703-706.
- Dasgupta B, Brown NE, King M (1998) Effects of sputum oscillations and rhDNase in vitro: a combined approach to treat cystic fibrosis lung disease. Pediatr Pulmonol 26: 250-255.
- Valente AM, Gastaldi AC, Cravo SL, Afonso JL, Sologuren MJJ, et al. (2004) The effect of two techniques on the characteristics and transport of sputum in patients with bronchiectasis. A pilot study. Physiotherapy 90: 158-164.
- Tambascio J, de Souza LT, Lisboa RM, Passarelli RC, de Souza HC, et al. (2011)The influence of Flutter®VRP1 components on mucus transport of patients with bronchiectasis. Respir Med 105: 1316-1321.
- Girard JP, Terki N (1994) The Flutter VRP1: a new personal pocket therapeutic device used as an adjunct to drug therapy in the management of bronchial asthma. J Investig Allergol Clin Immunol 4: 23-27.
- Weiner P, Zamir D, Waizman J, Weiner M (1996) Physiotherapy in chronic obstructive pulmonary disease: oscillatory breathing with flutter VRP1. Harefuah. 131: 14-17.
- Homnick DN, Anderson K, Marks JH (1998) Comparison of the flutter device to standard chest physiotherapy in hospitalized patients with cystic fibrosis: a pilot study. Chest 114: 993-997.
- Gondor M, Nixon PA, Mutich R, Rebovich P, Orenstein DM (1999) Comparison of Flutter device and chest physical therapy in the treatment of cystic fibrosis pulmonary exacerbation. Pediatr Pulmonol 28: 255-260.
- Wolkove N, Baltzan MA Jr, Kamel H, Rotaple M (2004) A randomized trial to evaluate the sustained efficacy of a mucus clearance device in ambulatory patients with chronic obstructive pulmonary disease. Can Respir J 11: 567-572.
- Wang Q, Zhang X, Li Q (2010) Effects of a Flutter Mucus-Clearance Device on Pulmonary Function Test Results in Healthy People 85 Years and Older in China. Respir Care 2010 55: 1449-1452.
- Sontag MK, Quittner AL, Modi AC, Koenig JM, Giles D, et al. (2010) Lessons learned from a randomized trial of airway secretion clearance techniques in cystic fibrosis. Pediatr Pulmonol 45: 291-300.
- Swift GL, Rainer T, Saran R, Campbell IA, Prescott RJ (1994) Use of flutter VRP1 in the management of patients with steroid-dependent asthma. Respiration 61: 126-129.
- Cegla UH, Bautz M, Frode G, Werner T (1997) Physical therapy in patients with COPD and tracheobronchial instability-comparison of 2 oscillating PEP systems (RC-Cornet, VRP1 Desitin). Results of a randommized prospective study of 90 patients. Pneumologie 51: 129-136.
- Padman R, Geouque DM, Engelhardt MT (1999) Effects of the flutter device on pulmonary function studies among pediatric cystic fibrosis patients. Del Med J 71: 13-18.
- Oermann CM, Sockrider MM, Giles D, Sontag MK, Accurso FJ, et al. (2001) Comparison of high-frequency chest wall oscillation and oscillating positive expiratory pressure in the home management of cystic fibrosis: a pilot study. Pediatr Pulmonol 32: 372-377.
- Veiga J, Miranda IA, Dames KK, Jansen JM, Melo PL (2008) Respiratory mechanics effects of Flutter VRP1 in healthy subjects and COPD, asthma and bronchiectasis patients. Pulmno RJ 17: 18-21.
- Figueiredo PH, Zin WA, Guimaraes FS (2012) Flutter valve improves respiratory mechanics and sputum production in patients with bronchiectasis. Physiother Res Int. 17: 12-20.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 21767
- [From(publication date):
June-2016 - Mar 31, 2025] - Breakdown by view type
- HTML page views : 20538
- PDF downloads : 1229