Fluoroscopy CT versus Cone-Beam CT for Imaging-Guided Percutaneous Transthoracic Needle Biopsy of Lung Base Nodules
Received: 01-Apr-2023 / Manuscript No. ccoa-23-95858 / Editor assigned: 03-Apr-2023 / PreQC No. PQ- ccoa-23-95858; / Reviewed: 17-Apr-2023 / Revised: 22-Apr-2023 / Manuscript No. ccoa-23-95858(R) / Published Date: 29-Apr-2023
Abstract
Cone biopsy, also known as conisation, is a surgical procedure that involves the removal of a cone-shaped piece of tissue from the cervix. This procedure is often used to diagnose or treat cervical abnormalities, such as precancerous or cancerous cells.
Imaging-guided cone biopsy involves the use of imaging techniques, such as ultrasound or MRI, to guide the placement of instruments during the procedure. This allows for more precise removal of the targeted tissue and can help minimize damage to surrounding healthy tissue.
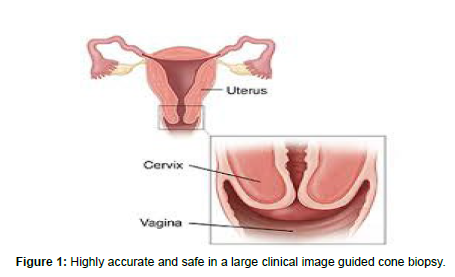
The use of imaging-guided cone biopsy has been shown to improve the accuracy and safety of the procedure, particularly in cases where the abnormalities are located deep within the cervix or close to critical structures such as blood vessels or the urinary bladder.
Keywords
Biopsy; Cancer; Ultrasound; Cervix; Cone
Introduction
Cone biopsy is a surgical procedure used to remove a cone-shaped piece of tissue from the cervix for diagnostic or therapeutic purposes. This procedure is often performed to investigate abnormalities detected during a Pap test, colposcopy, or other imaging studies [1].
Imaging-guided cone biopsy involves the use of various imaging techniques, such as ultrasound, magnetic resonance imaging (MRI), or computed tomography (CT), to guide the biopsy needle or surgical instruments to the precise location of the abnormal tissue [2].
The use of imaging guidance has several advantages, including increased accuracy, reduced risk of complications, and the ability to target smaller lesions that may be missed by traditional biopsy methods. Moreover, imaging guidance can help ensure that the biopsy sample is representative of the abnormal tissue, which can improve the accuracy of the diagnosis and guide further treatment decisions.
Image Guidance
Cone biopsy is a surgical procedure in which a cone-shaped piece of tissue is removed from the cervix for examination. Image guidance may be used during cone biopsy to help the surgeon accurately target the biopsy site and avoid damage to surrounding tissue.
The most commonly used imaging modalities for cone biopsy are colposcopy and ultrasound. Colposcopy involves using a special instrument called a colposcopy to magnify and illuminate the cervix, allowing the surgeon to visualize the biopsy site and surrounding tissue. Ultrasound, on the other hand, uses high-frequency sound waves to create images of the cervix, which can be used to guide the biopsy needle to the correct location (Figure 1).
In some cases, other imaging modalities such as MRI or CT may also be used to guide cone biopsy, particularly if there is concern about the extent or location of the abnormal tissue. However, these modalities are less commonly used due to their higher cost and complexity [3].
Overall, image guidance can be a valuable tool for ensuring the accuracy and safety of cone biopsy, particularly in cases where the abnormal tissue is located deep within the cervix or near important structures such as the bladder or rectum. Your doctor can help determine whether image guidance is necessary or appropriate for your specific case.
Fluoroscopy CT versus cone-beam CT
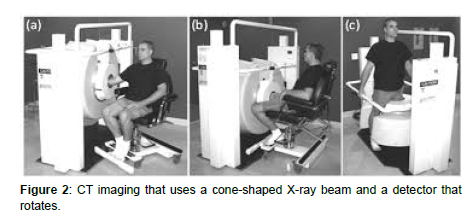
Fluoroscopy CT and cone-beam CT are both imaging techniques used in medical imaging. They have some similarities, but also some important differences (Figure 2).
Fluoroscopy CT, also known as dynamic CT or cine CT, is a type of CT imaging that allows for the visualization of moving structures in real time. It uses a continuous X-ray beam and a rotating detector to produce 3D images of the body. This technique is commonly used in interventional radiology procedures such as angiography and biopsies, where real-time imaging is necessary [4, 5].
Cone-beam CT, on the other hand, is a type of CT imaging that uses a cone-shaped X-ray beam and a detector that rotates around the patient to produce 3D images. Unlike fluoroscopy CT, cone-beam CT produces a single 3D image rather than a series of images over time. This technique is commonly used in dental and maxillofacial imaging, as well as in orthopedic and spine surgery planning.
In terms of image quality, cone-beam CT tends to produce higher resolution images than fluoroscopy CT, but it also exposes the patient to a higher dose of radiation. Fluoroscopy CT, on the other hand, produces lower resolution images but exposes the patient to a lower dose of radiation.
Overall, the choice of imaging technique will depend on the specific clinical scenario and the preferences of the radiologist or surgeon. Both techniques have their own advantages and disadvantages and should be used judiciously to balance the benefits and risks to the patient.
Discussion
Fluoroscopy CT (computed tomography) and cone-beam CT are both medical imaging techniques used to generate cross-sectional images of the body. However, there are some differences between the two techniques.
Fluoroscopy CT uses X-ray technology to produce detailed images of the body. It involves the use of a rotating X-ray source and a detector that is moved along the body. The images produced by fluoroscopy CT are 2D and can be reconstructed into 3D images. It is commonly used for diagnostic purposes, such as detecting bone fractures, Tumors, and other abnormalities.
On the other hand, cone-beam CT is a newer imaging technique that also uses X-rays but is more similar to traditional CT scans. It uses a cone-shaped X-ray beam and a detector that rotates around the patient to produce 3D images of the body. Cone-beam CT is commonly used in dentistry, Orthopedics, and radiation therapy planning.
One advantage of cone-beam CT is that it delivers a lower radiation dose to the patient compared to fluoroscopy CT. Cone-beam CT also provides higher resolution images with less distortion compared to fluoroscopy CT. However, cone-beam CT has a limited field of view and is not suitable for imaging larger parts of the body, while fluoroscopy CT can image larger areas.
Conclusion
Cone biopsy is a surgical procedure used to remove a cone-shaped piece of tissue from the cervix for diagnostic or therapeutic purposes. The procedure is typically performed to diagnose or treat cervical cancer, as well as to investigate abnormal Pap smear results.
The conclusion of a cone biopsy procedure depends on the reason for the biopsy and the findings of the biopsy. If the procedure was performed to diagnose cervical cancer, the conclusion would involve analysing the tissue sample to determine the presence and extent of cancerous cells. If the procedure was performed to treat cervical cancer, the conclusion would involve ensuring that all cancerous cells were removed and monitoring the patient for any signs of recurrence.
In general, the recovery from a cone biopsy is relatively quick, and patients are typically able to return to normal activities within a few days. However, as with any surgical procedure, there are risks and potential complications associated with cone biopsy, such as bleeding, infection, and scarring. Patients should be aware of these risks and discuss any concerns with their healthcare provider before undergoing the procedure.
References
- Chuang L, Kanis MJ, Miller B, Wright J, Small W, et al. (2016) Treating locally advanced cervical cancer with concurrent chemo radiation without brachytherapy in low-resource countries. Am J Clin Oncol 39: 92-97.
- Chuang LT, Randall TC, Denny L (2017) Sister society meeting on global education development and collaboration: Meeting report Int J Gynecol Cancer 26: 1186-1188.
- Chuang LT, Randall TC Karlan BY (2017) Efforts towards erasing borders in gynaecologic cancer? Gynecol Oncol Reports 21: 5-6.
- Gage JC, Ferreccio C, Gonzales M, Arroyo R, Huivin M, et al. (2003) Robles Follow-up care of women with an abnormal cytology in a low-resource setting. Cancer Detect Prev 27: 466-471.
- Madzima TR, Madzima M, Vahabi A (2017) Lofters Emerging role of HPV self-sampling in cervical cancer screening for hard-to-reach women: Focused literature review. Can Fam Phys 63: 597-601.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Mendalev D (2023) Fluoroscopy CT versus Cone-Beam CT for Imaging- Guided Percutaneous Transthoracic Needle Biopsy of Lung Base Nodules. Cervical Cancer, 8: 152.
Copyright: © 2023 Mendalev D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 978
- [From(publication date): 0-2023 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 746
- PDF downloads: 232