Fibrodysplasia Ossificans Progressiva: A Case Report
Received: 08-Nov-2018 / Accepted Date: 03-Dec-2018 / Published Date: 10-Dec-2018 DOI: 10.4172/2167-7964.1000301
Abstract
Background: Fibrodysplasia Ossificans Progressiva (FOP) is an extremely rare autosomal dominant genetic disease characterized by attacks of muscle inflammation followed by development of intramuscular calcifications.
Case report: A 4 month-old female patient presented to the Children’s Cancer Hospital (CCH) with a history of scalp lesions excised outside CCH. Pathology suggested juvenile fibromatosis throughout follow up, development of new lesions and consequent intra-muscular calcifications raised doubt over the diagnosis, FOP was suspected and confirmed by foot X-ray
Conclusion: Fibrodysplasia Ossificans Progressiva is a rare disease that should be considered in young patients presenting with muscular inflammatory mass lesions and/or intramuscular calcification. Early diagnosis and management of the disease has important implications on the quality of life of the patients
Keywords: Fibrodysplasia ossificans progressive; Myositis ossificans progressive; Intramuscular calcifications
Introduction
Fibrodysplasia Ossificans Progressiva (FOP) is an extremely rare disease, caused by an autosomal dominant genetic mutation in activin receptor IA/activin-like kinase 2 (ACVR1/ALK2) receptor genes [1]. Most cases occur by spontaneous genetic mutation [2].
The natural history classically involves flare ups of muscle inflammation which is followed by healing ossification. Consequent attacks result in formation of bony bridges throughout the muscles, causing limitation of movement and progressive disability. However, progressive ossification without inflammatory flare ups has been reported in a considerable number of patients [3].
Case Report
A 4 month-old female patient was referred to the Children’s Cancer Hospital (CCH) with a left sided scalp lesions excised outside CCH. Referred slide and block pathology revision report at CCH revealed a “Spindle Myxoid Fibroblastic Lesion”, suggested diagnoses were “Low Grade Myxofibrosarcoma” vs “Cranial Fasciitis”. Post-operative MRI revealed an extra-cranial fluid collection at the operative site. Patient was put under follow up.
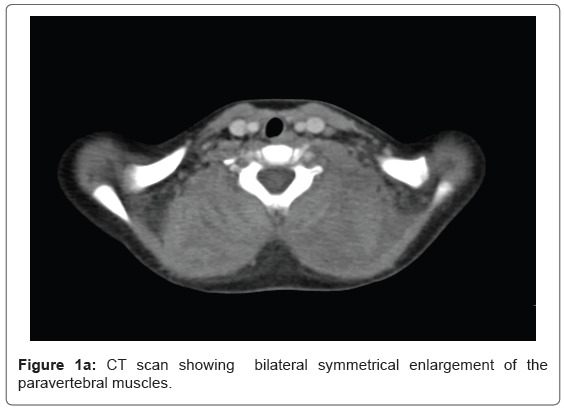
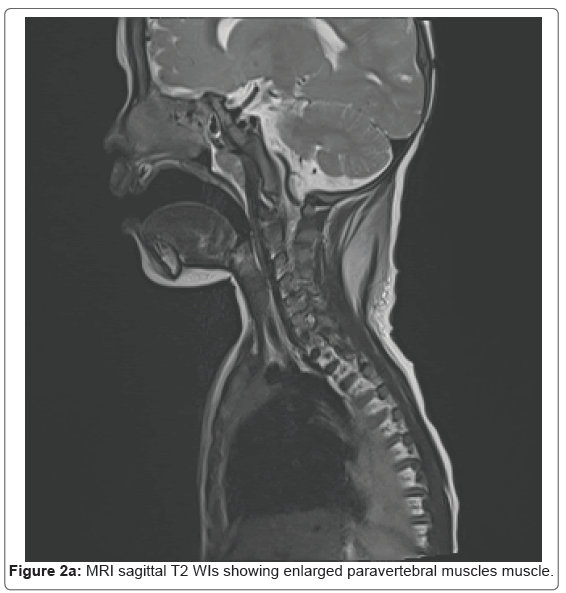
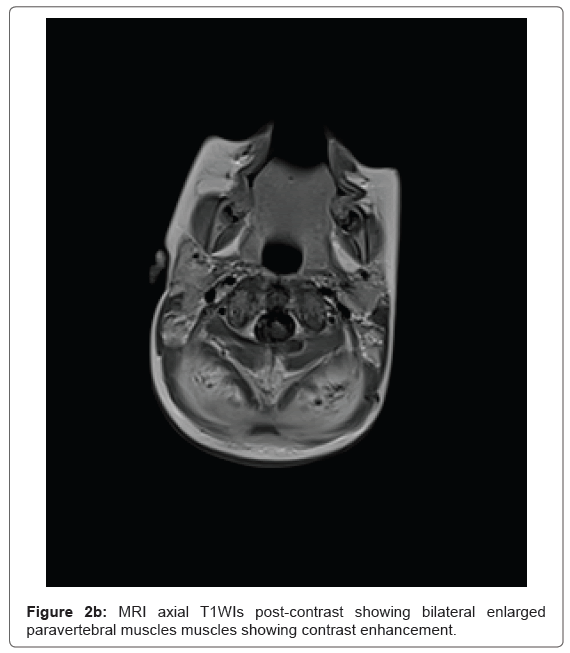
One year later, patient appeared with newly developed bilateral cervical swellings, CT and MRI revealed diffuse bilateral paravertebral and neck extensor muscles’ swelling with diffuse high T2 signal intensity on MRI (Figures 1a, 2a and 2b). Biopsy was performed and pathology favored juvenile fibromatosis. Patient was placed on the relevant chemotherapy protocol.
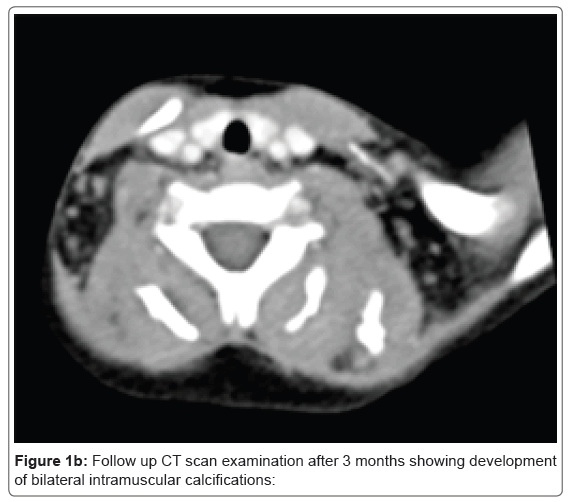
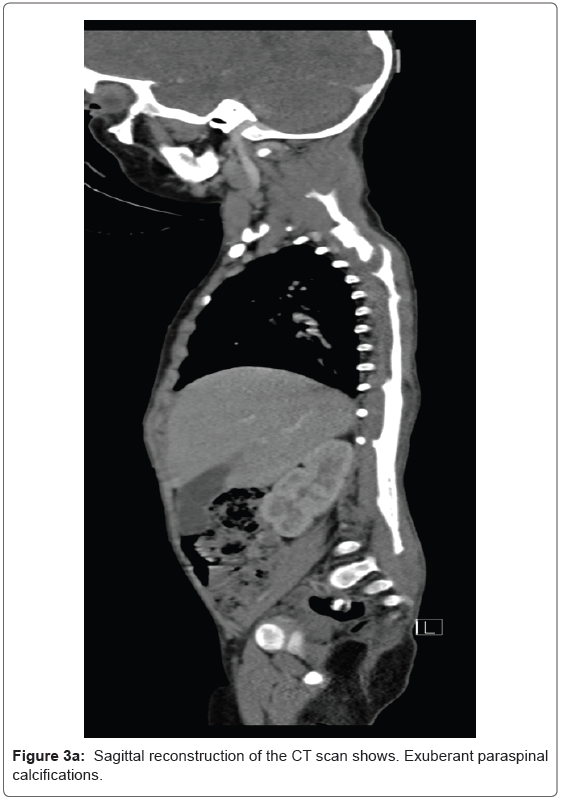
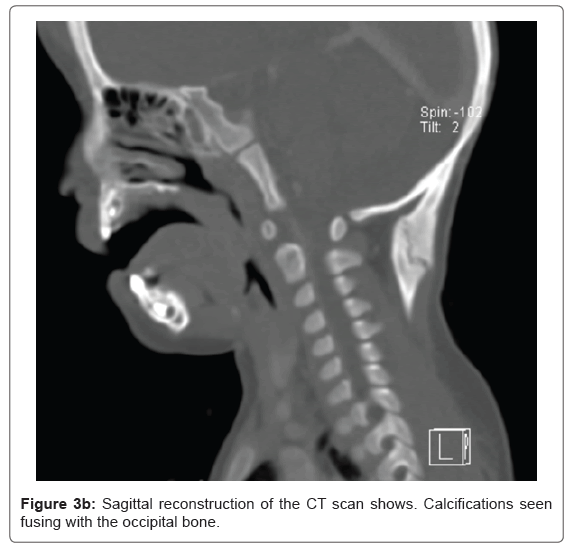
Throughout the follow up, further lesions began to develop in the neck, the chest wall and the back. After 3 months later of follow up, CT revealed a decrease in the size of the swellings in the paravertebral and neck extensor muscles, yet with newly-developed extensive intramuscular calcifications (Figure 1b). These calcifications extended along with the paravertebral muscles, latissimus dorsi and the pyriformis muscles and appeared more mature cranially, with thick bone formation seen at the sub-occipital region, seen merging with the occipital bone (Figure 3a, 3b).
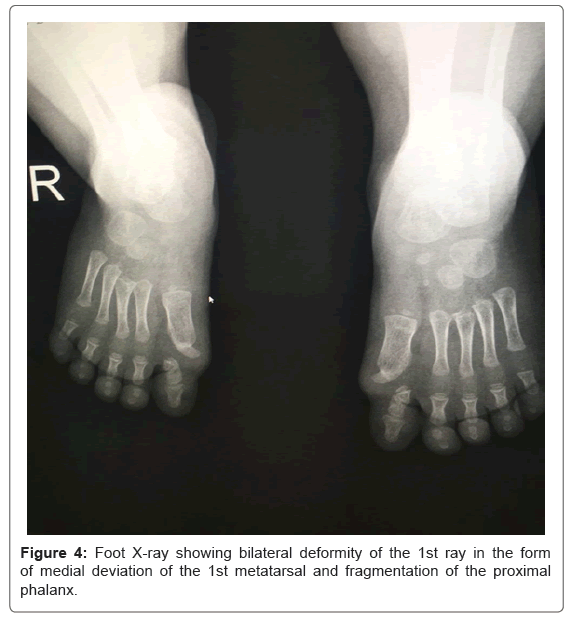
At this point, the diagnosis of FOP was suspected and foot X-rays were performed which revealed deformities of the 1st ray bilaterally in the form of medial deviation of the 1st metatarsal and fragmentation of the proximal phalanx (Figure 4). Diagnosis was confirmed and chemotherapy was stopped.
Discussion
FOP is an extremely rare disease, with an incidence of about 1/2000000 people [4]. Recent survey study conducted in cooperation with the International Fibrodysplasia Ossificans Progressiva Association (IFOPA) on 500 FOP patients revealed a slight female predominance (55.8%), with the United States of America being the country of the largest representation of the disease, followed by China [3].
FOP lies within the spectrum of congenital neuromuscular disorders, a group of diseases in which different imaging techniques play an important role in diagnosis and assessing the degree of severity of the disease [5]. Whilst detection of muscular inflammatory changes is difficult using CT due to poor contrasts of soft tissues [6], MRI shows high sensitivity to muscle inflammation and oedema in the form of diffuse high signal intensity on T2 and STIR weighted images[5,6].
Usually muscle oedema and inflammation are the first sign of muscular dystrophies and they precede degenerative changes and could serve as an alert sign for the radiologist [5,7].
Scalp nodules are a common presentation of FOP and often present as the first manifestation [8], differential diagnosis of soft tissue nodules includes cranial fasciitis, juvenile fibrosarcoma and aggressive fibromatosis, yet some characteristics can help a radiologist differentiate those entities from FOP; cranial fasciitis usually presents with an underlying osteolytic skull lesion [5,6] while juvenile fibrosarcoma usually occurs immediately post-natal or during the first year of life and its common site is in the extremities [7], finally aggressive fibromatosis commonly occurs in the abdominal wall, abdomen and proximal musculature of the extremities (including shoulders and buttocks) and it does not metastasize [8].
Differential diagnosis of intra-muscular ossification includes other forms of myositis ossificans. Myositis ossificans is classified into 3 subtypes: Traumatic Myositis Ossificans Circumscripta, representing the majority of cases (60%-75%), which occurs following blunt trauma, mainly in large appendicular muscles. This lesion occurs mainly in young men and in case of pediatric population it should raise the suspicion of child abuse [9].
Atraumatic Myositis Ossificans Circumscripta is characterized by ossification in which no specific cause could be found, yet the presence of a trauma that went unnoticed at the time has been suggested by some authors [10]. Again this is a localised form of muscular ossification.
Finally, as in our case, Myositis Ossificans Progressiva, another name for Fibrodysplasia Ossificans Progressive, the bilateral symmetrical inflammatory changes of the paravertebral muscles was typical of FOP, as it has a characteristic course which starts at the cervical para-vertebral muscles and spreads caudally [11].
Other radiological differential diagnoses include hereditary diseases showing ectopic calcifications, mainly Progressive Osseous Heteroplasia and Albright Hereditary Osteodystrophy, yet these diseases show mainly cutaneous and subcutaneous rather than intramuscular calcifications [12,13].
In our case, diagnosis was confirmed by performing foot X-ray, which revealed anomalies of the 1st ray bilaterally, the presence of shortened great toe with a single or deformed phalanx is diagnostic [2]. Treatment of FOP is generally symptomatic, consisting of anti-inflammatories including steroids and NSAIDs during flare ups to decreased myositis and consequent healing by fibrosis and ossification. Other drugs have been tried with limited effect including Leukotriene inhibitors and Biphosphonates [4]. It is important to note that biopsy and surgical treatment -done mainly to disrupt bony bridges which limit the movement are discouraged, as surgical manipulation of muscular tissue heals by fibrosis and further ossification [14-18].
Conclusion
FOP is a rare disease, yet a diagnosis that should be kept in mind with patients presenting with muscular inflammatory mass lesions in young age. Some key findings could alert a radiologist of the diagnosis, including bilateral and symmetrical muscular inflammation in the cervical para-spinal region followed by calcifications that develop from cranial to caudal on follow up. Foot X-ray should be performed upon suspicion. Early diagnosis and treatment of flare ups results in delayed development of ossification and hence disability.
References
- Shore EM, Xu M, Feldman GJ, George JF, David AC, et al. (2006) A recurrent mutation in the BMP type I receptor ACVR1 causes inherited and sporadic fibrodysplasia ossificans progressiva. Nat Genet 38: 525-527.
- Kaplan F, Hahn G, Zasloff M (1994) Heterotopic ossification: Two rare forms and what they can teach us. J Am Acad Orthop Surg 2: 288-296.
- Pignolo RJ, Bedfordm GC, Liljesthröm M, oira Durbin-Johnson, Blythe PS, et al. (2016) The natural history of flare-ups in fibrodysplasia ossificans progressiva (fop): a comprehensive global assessment. J Bone Miner Res 31: 650-656.
- Pignolo RJ, Shore EM, Kaplan FS (2011) Fibrodysplasia ossificans progressiva: Clinical and genetic aspects. Orphanet J Rare Dis 6: 80
- Wattjes MP, Kley RA, Fischer D (2010) Neuromuscular imaging in inherited muscle diseases. Eur Radiol 20: 2447-2460.
- Ortolan P, Zanato R, Coran A, Beltrame V, Stramare R (2015) Â Role of radiologic imaging in genetic and acquired neuromuscular disorders. Eur J Trans Myol 25: 5014.
- Straub V, Donahue KM, Allamand V, Davisson RL, Kim YR (2000) Contrast agent-enhanced magnetic resonance imaging of skeletal muscle damage in animal models of muscular dystrophy. Magn Reson Med 44: 655-659
- Piram M, Le MM, Bughin V, De Prost Y, Fraitag S, et al. (2011) Scalp nodules as a presenting sign of fibrodysplasia ossificans progressiva: A register-based study. J Am Dermatol 64: 97-101.
- Summers LE, Florez L, Berberian JM, Bhattacharjee M, Walsh JW (2007) Postoperative cranial fasciitis. J Neurosurg 106: 1080-1085.
- Keyserling HF, Castillo M, Smith JK (2003) Cranial fasciitis of childhood. Am J Neuroradiol 24: 1465-1467.
- Al-Salem AH (2011) Congenital-infantile fibrosarcoma masquerading as sacrococcygeal teratoma. J Pediatr Surg 46: 2177-2180.
- Simmonds J, Taki N, Chilton I, Vecchiotti M (2016) A rare case of pediatric Nontraumatic Myositis Ossificans in the posterior triangle. Int J Pediatr Otorhinolaryngol 84: 116-118.
- Gindele A, Schwamborn D, Tsironis K, Benz-Bohm G (2000) Myositis ossificans traumatica in young children: report of three cases and review of the literature. Ped Radiol 30: 451-459.
- Gonçalves AL, Masruha MR, De Campos CC, Ribeiro Delai PL, Pereira VLC (2005) Fibrodysplasia ossificans progressiva: Case report. Arq Neuropsiquiatr 63: 1090-1093.
- Adegbite NS, Xu M, Kaplan FS, Shore EM, Pignolo RJ (2008) Diagnostic and mutational spectrum of progressive osseous heteroplasia (POH) and other forms of GNASâ€based heterotopic ossification. Am J Med Genet 146A: 1788-1796.
- Salemi P, Skalamera OJM, Dickson LE, Germain-Lee EL (2018) Ossifications in albright hereditary osteodystrophy: role of genotype, inheritance, sex, age, hormonal status, and BMI. J Clin Endocrinol Metab 103: 158-168
- DÃaz-de la Torre J (2012) Fibrodysplasia ossificans progressiva. A case report. Acta Ortoped Mex 26: 192-196.
Citation: Anwar A, Elnadi I, Hussein M, Zaki I (2018) Fibrodysplasia Ossificans Progressiva: A Case Report. OMICS J Radiol 7: 301. DOI: 10.4172/2167-7964.1000301
Copyright: © 2018 Anwar A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 5204
- [From(publication date): 0-2018 - Feb 22, 2025]
- Breakdown by view type
- HTML page views: 4492
- PDF downloads: 712