Research Article Open Access
Fetus is Mature after 32 Weeks of Pregnancy
Maeda K1*, Serizawa M2 and Utsu M3
1Department of Obstetrics and Gynaecology, Tottori University Medical School, Yonago, Japan
2Department of Obstetrics and Gynaecology, Hamamatsu Medical Centre, Hamamatsu, Japan
3Department of Obstetrics and Gynaecology, Seirei Mikatahea Hospital, Japan
- *Corresponding Author:
- Maeda K
Department of Obstetrics and Gynaecology
Tottori University Medical School
Yonago, Japan
Tel: 81859226856
E-mail: maedak@mocha.ocn.ne.jp
Received date: June 24, 2017; Accepted date: June 26, 2017; Published date: June 30, 2017
Citation: Maeda K, Serizawa M, Utsu M (2017) Fetus is Mature after 32 Weeks of Pregnancy. J Preg Child Health 4:339. doi:10.4172/2376-127X.1000339
Copyright: © 2017 Maeda K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Research Article
We would like to confirm fetal maturation in the treatment of 164 MD twin pregnancy with caesarean delivery after the management of maternal rest, tocolysis and detailed monitoring with ultrasound techniques, where no TTTS developed in the twins, while the existence of mild blood transfer to the recipient twin from the donor, was confirmed by the enlargement of cardio-thorax ratio [1].
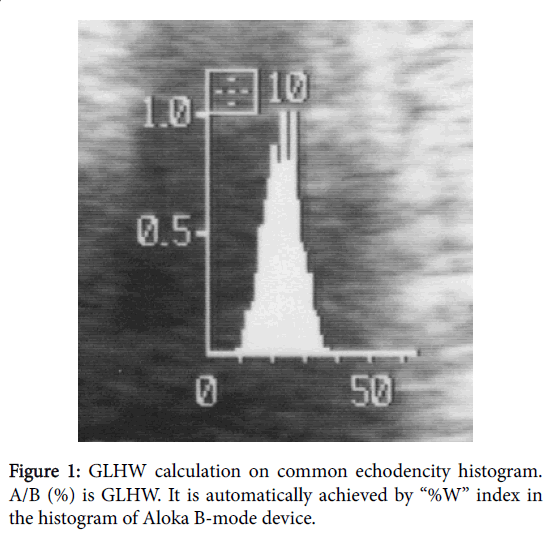
Fetal lung gray level histogram width (GLHW), an ultrasonic tissue characterization was measured in fetal lung and liver to estimate the lung maturity (Figure 1) [2] and the fetal age was studied in transient Braxton-Hichs uterine contraction.
Fetal lung GLHW was 35 and that of fetal liver was 36 in 32 weeks of pregnancy [3]. Fetal lung was mature, because the lung/liver ratio of GLHW multiplied by pregnancy weeks was 31, which was larger than 29 in 32 weeks of pregnancy [2], when the twins received caesarean delivery to avoid the TTTS after the first blood transfer to recipient from the donor, which was suspected to be caused by a Braxton Hicks contraction. Although there was very mild reactive cardiac function change in the recipient only within 2 days in the stay in NICU, the infants were healthy and no failure afterwards.
Novel treatment of MD twins to avoid the TTTS was beneficial because the MD twins received caesarean delivery (CD) after ultrasonic imaging of cardio-thoracic ratio (CTR) higher than 0.4, which was resulted by the inflow of blood into the recipient heart in the uncontrollable uterine contraction by the tocolysis of the mother in around 32 weeks of pregnancy [1], which would be Braxton-Hicks contraction caused by prostaglandin developed at placental site by fetal adrenal corticosteroids. In summary, the uncontrollable uterine contraction might be a Braxton Hichs contraction, which was caused by fetal reaction to the stress around in 32 weeks, where it will be a physiologic and endocrinologic reaction of a mature fetus to the stress. Therefore, it was uncontrollable by the tocolysis with terbutaline.
The 82 mothers of 164 MD twins who received the treatments with the rest and tocolysis followed by Caesarean delivery around at 32 weeks of pregnancy [1]. Why there was no TTTS before 28 weeks and in 24 weeks of pregnancy? The early TTTS might develop by blood transfer in no ultrasound monitoring in their pregnancy and controllable contraction was suppressed by maternal rest and tocolysis in our novel treatment. The 32 weeks of pregnancy will be important fetal age in the present novel study, namely, it may indicate fetal maturity, as the 32 weeks of pregnancy is the stage when transient Braxton-Hicks’ contraction initiates before the appearance of labor contraction. According to approved theory, the fetus excretes adrenal corticosteroids into umbilical blood which reached placenta, stimulating local decidua to secrete prostaglandin developing the initial uterine contraction at placental site as the pace-maker of whole uterine contraction, namely, the Braxton-Hicks contraction may show the fetal maturity in the production of protective adrenal corticosteroid against stresses. If so, the authors would keep the pregnancy until the stage of the functional maturity of twins to resist stresses. The Braxton- Hicks contraction will enhance the first blood transfer to the recipient from the donor, and enlarged the recipient heart in MD twin pregnancy. Thus, the twins were guarded by fetal functional maturity from the surgery of caesarean delivery, where the caesarean delivery would not damage twins. Also there was no problem in the infants after the caesarean delivery. The Braxton-Hicks contraction may promote the blood transfer, but there was the interval to prepare the caesarean delivery. Also, the Brasxton-Hicks contraction would be uncontrollable by the tocolysis, because it was physiologic and endocrinologic, Functional fetal maturity will develop at around 32 weeks of pregnancy, which was estimated by feal lung maturity and Braxton^ Hicks uterine contraction.
References
- Utsu M, Uehasa S M, Maeda K (2017) Favourable outcomes of 164 MD twins. JOGR
- Serizawa M, Maeda K (2010) Non-invasive fetal lung maturity prediction cases on ultrasonic gray level histogram width. Ultrasound Med Biol 36: 1998-2003.
- Maeda K, Utsu M, Yamamoto N, Serizawa M (1999) Echogenicity of fetal lung and liver quantified by the grey-level histogram width. Ultrasound Med Biol 25: 201-208.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 6643
- [From(publication date):
June-2017 - Jul 02, 2025] - Breakdown by view type
- HTML page views : 5769
- PDF downloads : 874