Feto-Maternal Outcome of Vaginal Birth after Cesarean and Associated Factors Among Mothers with Previous Cesarean Scar at Attat Lord Merry Primary Hospital, Gurage Zone, South Ethiopia
Received: 05-Sep-2018 / Accepted Date: 19-Sep-2018 / Published Date: 26-Sep-2018 DOI: 10.4172/2376-127X.1000390
Keywords: Previous cesarean section; Feto-maternal outcome; Success of VBAC; Factors associated
Introduction
ANC: Antenatal Care; APGAR: Appearance, Pulse Rate, Grimace, Activity and Respiratory Rate; CS: Cesarean Section; CSA: Central Statistics Association; CPD: Cephalo-Pelvic Disproportion; GA: Gestational Age; GC: Gregorian Calendar; GYN: Gynecology; HCT: Hematocrit; HIV: Human Immune Deficiency Virus; ICU: Intensive Care Unit; IEOS: Integrated Emergency Obstetrics and Surgery; LNMP: Last Normal Menstrual Period; LUSTCS: Lower Uterine Segment Cesarean Section; NGO: Non-Governmental Organization; NICU: Neonatal Intensive Care Unit; PMR: Per Natal Mortality Rate; VBAC: Vaginal Birth After Cesarean Section; WHO: World Health Organization; TOS: Trial of Scar
Background
Caesarean delivery is an operation done to deliver a baby through an incision in the uterus. It is the most frequently performed surgical procedure worldwide. Cesarean section is one of life saving procedures and intervention attributed to decrement of the maternal mortality and morbidity rates [1].
Even though, variation exists in rates of caesarean delivery across countries, currently the rate ranges from 10% to 40% [1,2]. Previous caesarean section has been found to be the commonest cause of increased caesarean section rate in many parts of the world [1]. Because of increased risk of maternal complications with repeat caesarean section and safety of VBAC, trial of labor for selected group of patients with previous scar has become a preferred strategy. A study recommended that, in the absence of a contraindication, a woman with one previous low transverse cesarean delivery be counseled attempt labor in a subsequent pregnancy [1]. These attempts were highly successful rates of Vaginal Birth After previous Cesarean (VBAC) increased from 3.4% to 28.3%, along with a concomitant decline in total cesarean delivery rates for the United States [2].
Vaginal Birth After Cesarean section (VBAC) is associated with shorter maternal hospitalizations, less blood loss and fewer transfusions, fewer infections and fewer thromboembolic events than cesarean delivery. Several reports have indicated that the absolute risk of uterine rupture attributable to a trial of labor is about 1 per 1000 [1-4]. A 60% to 80% success rate of vaginal birth after previous caesarean section has been reported by many authors if the primary caesarean was done for nonrecurring indications [1]. Some of the non-recurring indications for caesarean section are: poor labor progress, fetal distress, placenta previa, transverse lie, breech presentation, oblique lie, pregnancy induced hypertension and twins [1,3,4-6].
British figures indicate that among women with a prior caesarean section, 33% will successfully achieve vaginal birth in the subsequent pregnancy. Again there was considerable variation across institutions ranging from 6% to 64% [7]. One study in Lahore reported successful vaginal delivery in 70% of the patients and repeat emergency caesarean section in 30% of the patients. The leading indications for the repeat caesarean sections were: failure to progress, fetal distress and scar tenderness. There were no maternal and fetal complications occurred. They concluded that VBAC is a safe practice [8].
Both, attempting a vaginal birth and opting for an Elective Repeat Cesarean Section (ERCS) are associated with different risks for the mother and newborn and deciding a delivery plan involves a difficult weighing of those cases. For years, researchers have maintained an interest in the effective prediction or identification of factors, which can influence the outcome of a TOS. The ability to predict the outcome of an attempted trial of vaginal delivery plays an important role in initial counseling of pregnant women with previous one cesarean delivery [9].
Studies on predictors of success are few and most of them conducted in developed countries and difficult to generalize for resouce limited setting. There is no study that assessed feto-maternal outcome and factors associated among mothers with previous one caesarean scar at Attat Catholic Primary Hospital. Hence, the objective of this study was to determine the feto-maternal outcome of pregnancy among women with previous cesarean section who gave birth at Attat Catholic Hospital and associated factors. More specifically, to assess the common mode of delivery among mothers with the pervious one cesarean scar, to determine the outcome of VBAC and associated factors.
Materials and Methods
Study setting and design
The study was conducted at Aattat Primary Hospital Gurage Zone, SNNPR, Ethiopia, which is 175 km away from Addis Ababa and 410 km from regional city, Hawasa.
The hospital was established in 1961 E.C by Catholic Missionary and still now administered by them. The catchment population is 800,000, of which 51.2% females and 48.8% males. The Zone has 40 Health Centers and 2 newly established hospital which are government owned and all referred to this Hospital. It is one of affiliated hospital training IEOS students in conjunction with JUSU. It has 100 beds with delivery room, which give services for parturient mothers and other patients. The hospital has multidisciplinary staffs (Gynecologist, General Surgeon, emergency surgery students, Pharmacist, Lab. Technologist, midwives and clinical nurses). Through all the days of week the services are provided free of charge for all laboring mother.
Hospital based cross-sectional retrospective study design was used from October 01/2015-Septmeber 30/2016. All mothers with pervious one cesarean scar who gave birth in Attat Catholic hospital were source population and all mothers with one pervious cesarean scar who gave birth in Attat Catholic Hospital within the study period were study population. Women with one previous lower segment cesarean section, singleton pregnancy, cephalic presentation and term gestation were included in the study. However, Those women with two or more cesarean sections, previous uterine surgery like myomectomy and classical section were excluded.
Sample size
All mothers with one pervious cesarean scar who gave birth within the specified period in St. Luke Catholic Primary Hospital were included which is 169.
Study variables
Dependent variable is success of VBAC and independent variables were age, residence, gravidity, parity, LNMP, ANC follow up, GA, duration of labor, FHB, cervical dilatation, station, pre operation HCT, pervious indication for cesarean section, time of passage of liquor and history of vaginal birth after cesarean.
Method of data collection
Data were collected using structured, standard data extraction format/checklist to collect patient information from delivery registration books, operation registration books and individual charts. The check list was prepared in English and information abstracted from medical record books. Eight data collectors were participate in the data collection process after training them for one day. Before the actual data collection, the checklist was pre-tested on 5% of the total sample size. Day to day supervision was carried out during the whole period of data collection by the supervisor. At the end of each day, the questionnaire was review and cross checked for completeness, accuracy and consistency by the investigator and corrective discussion were under taken with collectors.
Data processing and analysis
The collected data was being checked for its completeness, entered using Epidata version 3.1 and exported to SPSS-20 for analysis. Frequency distributions of both dependent and independent variables were worked out and the association between independent and dependent variables was measured and tested using chi square and AOR. To identify candidate predictors of VBAC, bivariate analysis was done. AOR was used at 95 % confidence interval and 5% level of precision to check level of significance.
Operational definitions
Gestational age is calculated from the LNMP or fundal height that was documented on the card, if not from the duration of amenorrhea documented from mothers recall and is rounded to the nearest weeks. Amenorrhea of 9 months was taken as 37-42 weeks gestation for all mothers.
Cesarean section- means delivery of the fetus, membrane and placenta after 28 weeks of gestation by opening of abdomen and uterus.
Elective cesarean section- operation that done at a pre-selected time before onset of labour, usually at completed 39 week.
Elective Repeat cesarean section- cesarean section done at a preselected time before onset of labour in presence of previous cesarean section.
Successful VBAC- A vaginal delivery (spontaneous or assisted) in a woman had previous one cesarean section.
Parity- number of births (both life birth & stillbirth) of at least 28 weeks of gestational age.
TOL- trial of labor after cesarean section to achieve VBAC.
Station- degree of engagement of the presenting part, measured as distance in centimeters or between the fetus and the ischial spines.
Arrest Disorders- (1) secondary arrest of dilatation, with no progressive cervical dilatation in the active phase of labor for 2 h or more and (2) arrest of descent, with descent failing to progress for 1 h or more.
Cephalo-Pelvic Disproportion (CPD)- is failure of the fetus to pass safely through the birth canal because the fetal head being relatively larger than the maternal pelvic size.
Prolonged 2nd stage: The 2nd stage of labor lasting more than 1 h in multipara and 2 h in nulliparous.
Cervical dilatation status- active stage- In general, requires ≥ 80% effacement and ≥ 4 cm dilation of the cervix.
Full dilatation/second stage- is from full dilation (10 cm) until delivery of the baby.
APGAR- a score for the new born based on appearance, heart rate, grimace, activity (movement) and response.
Fetal distress (NRFHRP)- abnormal fetal heart rate pattern with tachycardia of >160 beats/min. and bradycardia of <110 beats/min.
Operative vaginal delivery- applying direct traction on the fetal skull with forceps or vacuum.
Uterine dehiscence- when the uterine muscle is separated but the visceral peritoneum is intact.
Results
General descriptive statistics
During the one year period a total number of 3260 deliveries were conducted at Attat Catholic primary hospital. From this 2537 (78%) were delivered by Spontaneous Vaginal Delivery (SVD) and 723 (22%) were delivered by Cesarean Section (C/S). From total delivery, 169 have pervious one caesarean section scar and from that 146 offered TOS, 65(44.5%) have successful VBAC, emergency repeated caesarean section were done for 81 (55.5%) mother and 23 elective repeat cesarean section were done. Retrospective chart review was done with chart retrieval rate of 97%.
Socio-demographic characteristics
From a total of 169 mothers who had previous one caesarean scar were delivered among which about 91 (53.8%) were in the age group 25-30 years with mean age of 28 years SD ± 4 and more than half were rural residents 117 (69.2%) (Table 1).
| Variables | Category | No. | % |
|---|---|---|---|
| Age in years | <25 | 45 | 26.6 |
| 25-30 | 91 | 53.8 | |
| <30 | 33 | 19.5 | |
| Residence | Urban | 52 | 30.8 |
| Rural | 117 | 69.2 |
Table 1: Socio demographic characteristics of mothers who had previous one caesarean scare and tried for VBAC in JUSH, 2016.
Obstetrics history
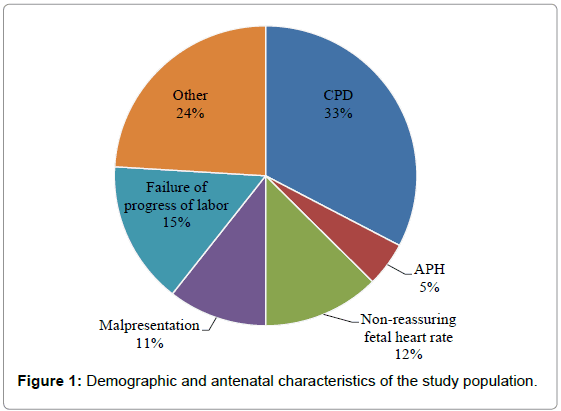
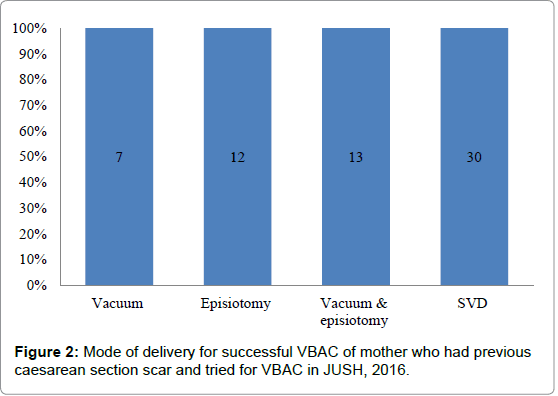
Most of the study subjects 69 (41 %) were Para one, majority of them were term by their gestational age 139 (82.2%) and who had at least one ANC visit 137 (81%). For more than half of the mother, there was no passage of liquor at admission and had history of VBAC 92 (54.4%), 73 (43.2%) respectively. Repeated caesarean section were 104 (61.5%) majority caesarean section were done as an emergence 81 (78 %) and station above zero at the time of admission 144 (85.2%), 65 (38.8%) have successful VBAC. Unknown indication for pervious caesarean section were the commonest 78 (46.2%), CPD were leading indication for current caesarean section and 34 (32.6%) SVD was the major mode of delivery for VBAC (Tables 2 and 3) (Figures 1 and 2).
| Variable | Frequency | % | |
|---|---|---|---|
| Gravidity | 02 Apr | 149 | 88.8 |
| >4 | 20 | 11.2 | |
| Parity | I | 69 | 41 |
| II | 59 | 35 | |
| >=III | 41 | 24 | |
| ANC Follow up | Yes | 137 | 81 |
| No | 32 | 19 | |
| Passage of liquor at the time of admission | Yes | 77 | 45.6 |
| No | 92 | 54.4 | |
| Duration of labor from the time of admission | <=12 | 123 | 72.8 |
| >12 | 13 | 7.7 | |
| Not in labor | 33 | 19.5 | |
| Cervical dilatation at the time of admission | <4 cm | 100 | 55 |
| 04 Jul | 64 | 38 | |
| 8-10 cm | 7 | 4.1 | |
| Not done | 5 | 3 | |
| Station at time of admission | Above 0 | 144 | 85.2 |
| 0 or below | 20 | 12 | |
| Not done | 5 | 3 | |
| HCT done before delivery | 07 Nov | 17 | 10 |
| >11 | 100 | 59.2 | |
| Not stated | 52 | 30.8 | |
| History of VBAC | Yes | 73 | 43.2 |
| No | 96 | 57.8 | |
Table 2: Obstetric history of mothers who had previous one caesarean scare and tried for VBAC in JUSH, 2016.
| Indications For Previous Caesarian Section | Frequency | % |
|---|---|---|
| Mal presentation | 16 | 9.5 |
| Failed induction | 5 | 3 |
| Non reassuring fetal heart rate | 24 | 14.2 |
| CPD | 44 | 26 |
| APH | 4 | 2.4 |
| Other | 6 | 3.6 |
| Unknown | 70 | 41.4 |
| Total | 169 | 100 |
Table 3: Indications for previous caesarean section for mothers who had previous one caesarean scare and tried for VBAC in JUSH, 2016.
Maternal and neonatal outcome
There was no maternal death during the study period, laparotomy were done for three scar dehiscence (2%) and 6 (3.6%) of mother had hemoglobin <7 and transfused blood. Majority of neonate with birth weights between 2500-4000 gm 161 (95%), 127 (75.1%) of neonate with first minute APGAR score of >=7 and 3 (1.8%) fetal death occurred (Table 4).
| Variable | No. | % | |
|---|---|---|---|
| Intra and post operation complication | PPH | 4 | 3.8 |
| Infection | 5 | 4.8 | |
| No complication | 95 | 91 | |
| Complication during vaginal birth | Scar dehiscence | 3 | 4.6 |
| PPH | 2 | 3 | |
| No complication | 60 | 92 | |
| Hemoglobin after delivery | <7 | 6 | 3.6 |
| >=7 | 112 | 30.2 | |
| Not stated | 51 | 66 | |
| Fetal out come | Alive | 166 | 98.2 |
| Dead | 3 | 1.8 | |
| Fifths minute Apgar score | <7 | 13 | 7.7 |
| >=7 | 153 | 90.5 | |
| 0 | 3 | 1.8 | |
Table 4: Maternal and neonatal outcome among mothers who had previous one caesarean scare and tried for VBAC in JUSH, 2016.
Factors associated with success of VBAC
The association between independent variables and success of VBAC was checked by binary logistic regression model to identify candidate variables (P<0.25). During bivariate analysis, parity, (COR-13.12, 95% CI: 4.99, 34.975 ), passage of liquor at admission (COR- 0.230, 95% CI: 0.116, 0.457), the indication for pervious cesarean section (OR-0.53, 95% CI: 0.14, 0.199), cervical dilation at admission (COR-3.6, 95% CI: 1.877, 6.903) and history of vaginal birth after cesarean section (COR- 0.46, 95% CI: 0.020, 0.103) were candidate variables identified for the final model.
In multivariate logistic regression after it was adjusted for the variables in the model, women who had passage of liquor at admission (AOR: 0.25, 95% CI: 0.084, 0.733), history of vaginal birth after cesarean (AOR: 1.88, 95% CI: 0.084, 0.733), cervical dilation at admission (AOR: 8.171, 95% CI: 3.303, 34.473) and type of indication for pervious cesarean section (AOR: 0.703, 95% CI: 0.014, 0.364) were significant factors associated with success of VBAC.
Three fourth (75%) of mothers who had passage of liquor at admission were less likely to have successful VBAC when compared to no history of passage of liquor at admission. Those mothers who had history of vaginal birth after cesarean section were almost 2 times more likely to have successful VBAC than counterparts. Those mothers who had dilated cervix at admission (>=4 cm) were 8 times more likely to have successful VBAC than counter parts. One third (30%) of mothers with NRFHR as an indication for pervious cesarean section were less likely to have successful VBAC than those mothers with unknown indication (Table 5).
| Variable | VBAC Success | COR 95%CI | AOR 95%CI | P value | ||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Parity | Para I | 8 | 61 | 13.12(4.99, 34.97)* | 1.436(.224, 9.902) | 0.702 |
| Para II | 31 | 28 | 1.456(.651, 3.29) | .488(.141, 1.692) | 0.258 | |
| Para III or + | 26 | 15 | 1 | 1 | - | |
| Passage of liquor | Yes | 16 | 61 | .230(.116, .457)* | .248(0.084, 0.733) | .012* |
| No | 49 | 43 | 1 | 1 | - | |
| History of VBAC | YES | 54 | 11 | .46(.20, .510)* | 1.88(0.220, 2.349) | .001* |
| No | 19 | 85 | 1 | 1 | - | |
| Cervical dilation at admission | <4cm | 23 | 42 | 3.6(1.877, 6.903)* | 8.171(3.303, 34.473)* | .001* |
| >=4cm | 69 | 30 | 1 | 1 | - | |
| Indication of previous C/S | Mal presentation | 8 | 8 | .373(1.2, 1.133) | .272(047, 1.586) | 0.148 |
| Failed induction and augmentation | 2 | 3 | .944(.143, 6.247) | 1.66(.121, 23.00) | 0.703 | |
| NRFHR | 21 | 3 | .053(014, .199) | .703(0.014, 0.864)* | .002* | |
| CPD | 11 | 33 | 1.118(.472, 2.647) | .813(.243, 2.72) | 0.737 | |
| APH | 1 | 3 | 1.118(.109, 11.445) | 6.564(.335, 128.6) | 0.215 | |
| Other | 3 | 3 | .373(.069, 2.009) | .109(.005, 2.258) | 0.152 | |
| Unknown | 19 | 51 | 1 | 1 | 1 | |
Table 5: Bivariate and multivariable logistic regression model showing factors associated with success of VBAC among mothers who had previous one caesarean scare in JUSH, 2016.
Discussions
Previous caesarean section was said to constitute the highest single indication for repeated caesarean section because obstetricians still regard vaginal birth after previous caesarean section as a high-risk option. This study revealed that common mode of delivery was repeated caesarean section 104 (61.5%) and CPD was the major indication for repeated caesarean section that may be due to unappropriate diagnoses of CPD. This study was conducted with the main objective of identifying factors associated with successful vaginal delivery on mothers offered trial of labor after previous one lower segment caesarean section. Significant factors were passage of liquor at admission, history of vaginal birth after cesarean, cervical dilation at admission and type of indication for pervious cesarean section were significant factors associated with success of VBAC.
The VBAC success rate vary from place to place 45.5% (in our study) was approximately similar with reported from three teaching hospitals such as Addis Ababa, Begum, Nigeria 49%, 43.2% and 50% respectively [5,9,10]. But our finding is lower than the rate of VBAC in Tanzania which was 55%, 69% in Havana Nigeria teaching hospital, 62.3% in India and 72.1% in Kuwaite and higher than the reported from USA 29% [3,4,11-13]. This discrepancy may be due to the variety type of indication diagnosed and applied for the previous cesarean section. Most probably if true CPD is an indication for the previous cesarean section, VBAC will fail. Other indications may not appear during trial of VBAC that is why the success rate is near to half. Our study revealed that successful VBAC was observed in 65 (45.5%) which was relatively lower than the standard accounts 60-80%.
In this study, the strongest predictor determining success of VBAC was cervical dilatation at admission. Those who were admitted with cervical diameter greater >=4 cm (Active first stage of labour) had a strong likelihood of vaginal delivery than those admitted at cervical diameter of 4,8,10]. Many authors reported previous vaginal birth was the single best predictor for successful VBAC [1,3,8-10].
Those mothers with fetal distress were indicated for pervious cesarean section has been found associated with high success of VBAC than unknown indication. CPD and failer of progress of labor were the main cause of failure which was the same result with Havana Specialist Hospital, Lagos, teaching hospitals in India [14,15]. Passage of liquor at admission was good prognostic factor which was having same finding with research done in Addis Ababa and other study Kuwait [4,9]. In our case parity is not a significant factor at the final model. However, multiparty were associated with high success rate of VBAC in another study. This discrepancy might be happened due to the sample size smaller in our case and other studies emphasized that increases in the number of vaginal deliveries increases the chances of having a successful VBAC, the same finding with Abu Dhabi and opposite to study in Addis Ababa [8,9].
In this study, maternal age, gestational age, duration of labor after admission, station at the time of admission and birth weight were not found significant determinants. However, Birth weight was one of the major predictor in another study [4,8]. Gestational age was not found as significant predictor of success of VBAC in our study. There are reports which found that gestational age above >=40 weeks is associated with poor success [4,8]. In our case, the finding could also be confounded by high number of unknown dates and ascertainment of correct date was not possible.
Perinatal and maternal outcome of labor were recorded among women who had trial of VBAC in this study were 3 scar dehiscence similar with research done in Tanzania 2%, India 2% and 3 perinatal death and no maternal death occurred which is similar finding with Malaysia 2 deaths [9,12,16]. Infection 5 (4.8%), PPH 4 (3.8%) were the major intra and post operation short term complication observed. However, when we compare these complications, it was higher than occurred during vaginal birth (VBAC). There is no difference in the first and fifth min APGAR score.
The possible limitations of this study were the clinical part of data abstracted from the secondary data or patient’s chart. This finding may be biased by the physician’s knowledge and skill who followed and did the procedures as well as documenting reliable information on the chart. In addition, we might miss other important variables due to incompleteness and unavailability of formats in the chart. The design is not strong enough to show cause and effect relationship rather it reveals with temporary factors which affect the outcome observed at a time. This finding may not be generalized to the target population because of non-probablity sampling technique used at a single facility.
Conclusion
Out of 169 mothers with previous one cesarean scar, 104 (61.5%) of them were undergone Trial of Labor (TOL). Of this, successful VBAC was observed in 65 (45.5%) which was relatively lower than the standard 60-80%. Passage of liquor at admission, history of vaginal birth after cesarean section, cervical dilation at admission >4 cm and indication (NRFHR) for pervious cesarean section were significant factors associated with success of VBAC.
Acknowledgments
We would like to express our deepest gratitude and appreciation to the hospital registry, health professionals working at Attat Catholic Primary hospital and Obstetrics and gynecology department of JU. We also aknowledge Jimma University-Institute of Health-IRB for securing ethical letter and for the fund provided.
Ethics approval and consent to participate
Ethical clearance and an approval letter obtained from Jimma University institute of health-institutional reviewing board, then support letter obtained from JUSH administrative office to the study hospital. Confidentiality was maintained by using anonymous codes and the patients’ chart number.
Consent to publish
All parties involved agreed to publish on international peer reviewed journal. During data abstraction, all concerned body informed and agreed on the major objective of the study which is for academic purpose including publication.
Availability of data and materials
The datasets used and/or analyzed during the current study are available. The SPSS (software) which is completed with raw dataset can be also shared. All data generated or analyzed during this study are included in this manuscript.
Conflict of Interest
All authors declare that they have no financial and non-financial competing interests. None of the authors of this paper has a financial or personal relationship with other people or organizations that could inappropriately influence or bias the content of the paper. It is to specifically state that “No Competing interests are at stake and there is No Conflict of Interest” with other people or organizations that could inappropriately influence or bias the content of the paper.
Authors contributions
Yibeltal Siraneh had made substantial contributions to conception and design, analysis and interpretation of data including manuscript preparation. Fanta Assefa and Mahlet Tesfaye worked a lot in acquisition of data and reviewed the manuscript for the intellectual content. All authors read and approved the final manuscript.
References
- Mc Graw-Hills Williams obstetrics: Prior cesarean delivery. (2007) Chapter 31. 24th edition.
- Fedhmeannacht (2013) Delivery after previous caesarean section, clinical practice guideline.in statute of Obstetricians and Gynaecologists, Royal College of Physicians of Ireland and Clinical Strategy and Programs Directorate, Health Service Executive Version 1.0 Guideline No. 5.
- Abdelazim IA, Elbiaa AM, Al-Kadi M, Yehia AH, Nusair BMS, et al. (2014) Maternal and obstetrical factors associated with successful trial of vaginal birth after cesarean section. J Turk Ger Gynecol Assoc 15: 245-249.
- Begum KS, Khan NU, Akter F (2014) Factors affecting the pregnancy outcome in patients with previous one caesarean section.
- Gupta JK (2015) Birth after previous caesarean birth. Royal collage of Obstetrician and Gynaecologists; Green-top Guideline No. 45.
- Balachandran L, Vaswani PR, Mogotlane R (2014) Pregnancy outcome in women with previous one cesarean section. J Clin Diagn Res 8: 99-102.
- Tan PC, Subramaniam RN, Omar SZ (2008) Trial of labor after one cesarean: Role of the order and number of prior vaginal births on the risk of emergency cesarean delivery and neonatal admission. Taiwan J Obstet Gynecol 47: 305-311.
- Birara M, Gebrehiwot Y (2013) Factors associated with success of vaginal birth after one caesarean section (VBAC) at three teaching hospitals in Addis Ababa, Ethiopia: A case control study. BMC Pregnancy Childbirth.
- Ugwu GO, Iyoke CA, Onah HE, Egwuatu VE, Ezugwu FO (2014) Maternal and perinatal outcomes of delivery after a previous cesarean section in Enugu, southeast Nigeria: A prospective observational study. Int J Womens Health 6: 301-305.
- Ezechi OC, Kalu BK, Njokanma FO, Ndububa V, Nwokoro CA, et al. (2005) Trial of labor after a previous caesarean section delivery: A private hospital experience. Ann Afr Med 4: 113-117.
- Dhillon BS, Chandhiok N, Bharti S, Bhatia P, Coyaji KJ, et al. (2014) Vaginal birth after cesarean section (VBAC) versus emergency repeat cesarean section at teaching hospitals in Indian: An ICMR task force study. Int J Reprod Contracept Obstet Gynecol.
- Pembe AB, Otham MK (2010) Pregnancy outcome after one previous caesarean section at a tertiary university teaching hospital in Tanzania. Tanzan J Health Res.
- Singh N, Tripathi R, Mala YM (2014) Maternal and fetal outcomes in patients with previous caesarean section undergoing trial of vaginal birth at a tertiary care centre in North India. J Preg Child Health.
- Boulvain M, Fraser WD, Brisson-Carroll G, Faron G, Wollast E (1997) Trial of labor after caesarean section in sub- Saharan Africa: A meta-analysis. Br J Obstet Gynaecol 104: 1385-1390.
- Patel RM, Jain L (2010) Delivery after previous cesarean: Short-term perinatal outcomes. Semin Perinatol 34: 272-280.
Citation: Siraneh Y, Assefa F, Tesfaye M (2018) Feto-Maternal Outcome of Vaginal Birth after Cesarean and Associated Factors Among Mothers with Previous Cesarean Scar at Attat Lord Merry Primary Hospital, Gurage Zone, South Ethiopia. J Preg Child Health 5: 390. DOI: 10.4172/2376-127X.1000390
Copyright: © 2018 Siraneh Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4488
- [From(publication date): 0-2018 - Apr 25, 2025]
- Breakdown by view type
- HTML page views: 3543
- PDF downloads: 945