Fetal Hibernation: A Case Report
Received: 02-Apr-2018 / Accepted Date: 23-Apr-2018 / Published Date: 30-Apr-2018 DOI: 10.4172/2376-127X.1000372
Abstract
Cardiotocography (CTG) is normally used to monitor fetal heart rate in order to determine the metabolic resources of the fetus and avoid intrauterine asphyxia. In our case study, the woman had preterm rupture of the membranes (at 39 weeks of gestation) but showed normal values e.g. CTG and fetal water. After 26.5 h, the CTG changed to a silent, hibernated pattern with tachycardia and reduced variability. Further, the mother developed fever and chorioamnionitis was suspected. Therefore, a sub-acute caesarean section performed followed by a medical examination of the newborn which showed normal values for Apgar score and vital parameters. Our interpretation is that the fetus responded to the maternal infection by a state of hibernation, shown by a pathological monotone heart rate pattern. It is remarkable that the fetus was able to sustain a well-preserved metabolism, shown by the normal acid-base status, considering the pathological and uniform CTG.
Keywords: Cardiotocography; Hibernation; Intrauterine asphyxia; Infection; Tachycardia
Introduction
Cardiotocography (CTG) is an integral part of intrapartum care in the majority of high-income countries [1]. CTG is used to monitor fetal heart rate (FHR) and the contractions of the uterus during pregnancy and birth, in order to determine the metabolic resources of the fetus and avoid intrauterine asphyxia. Lack of oxygen may result in an anaerobic metabolism and therefore potentially lead to a fetal metabolic acidosis. Severe acidosis can cause lactate accumulation and permanent damage to vital organs [2]. CTG is categorized into normal, suspicious, pathological and pre-terminal patterns based on the average pulse of the fetus [3]. FHR can be affected by many factors such as the activity of the fetus, the placental blood flow, intrauterine hypoxia, external stimuli, temperature increase and medication [3]. The lactate level determined from the scalp blood test’s level can be seen as a measure of the metabolic buffer capacity of the fetus and the acid-base conditions in the peripheral tissue. The lactate level indicates whether the fetus can maintain a sufficient oxygen saturation and energy supply through an aerobic metabolism or if an anaerobic metabolism with lactate formation is present.
The aim of this case report is to address a case with a pathological CTG with decreased variability, during birth, without the fetus having hypoxia.
Case
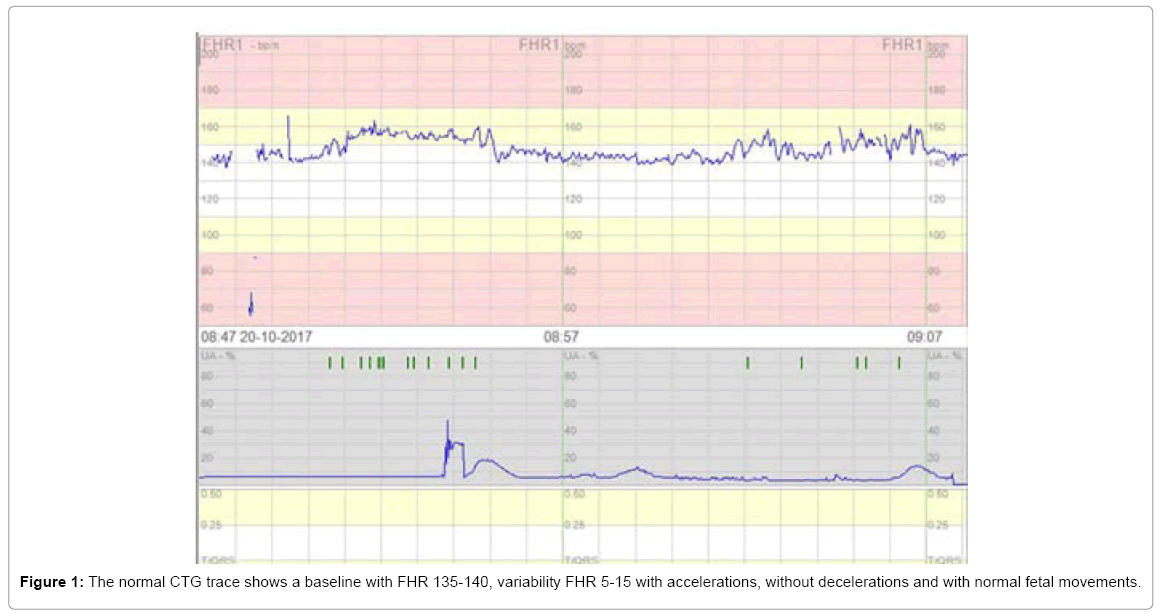
A 29 year old woman para 1, gravida 2, with BMI (Body Mass Index) of 48 and a previous uncomplicated pregnancy and birth came to the delivery room with preterm rupture of the membranes (PROM) at 39 weeks of gestation. Apart from hypothyroidism well treated on Eltroxin, the mother had no relevant medical history or prescription of medication. Upon arrival at the maternity ward (time 0 h after PROM), the vital parameters of the mother were normal with a temperature of 37.5°C, blood pressure 120/80 mm Hg, pulse 76 bpm and clear fetal water (FW). Furthermore, the urine stick was positive for blood and protein. A normal CTG from this case (t=0 after PROM) is shown in Figure 1. The CTG recorded a baseline FHR of 135-140 bpm, with a variability of 5-15 bpm, normal accelerations, without any kind of decelerations and normal fetal movements (Figure 1).
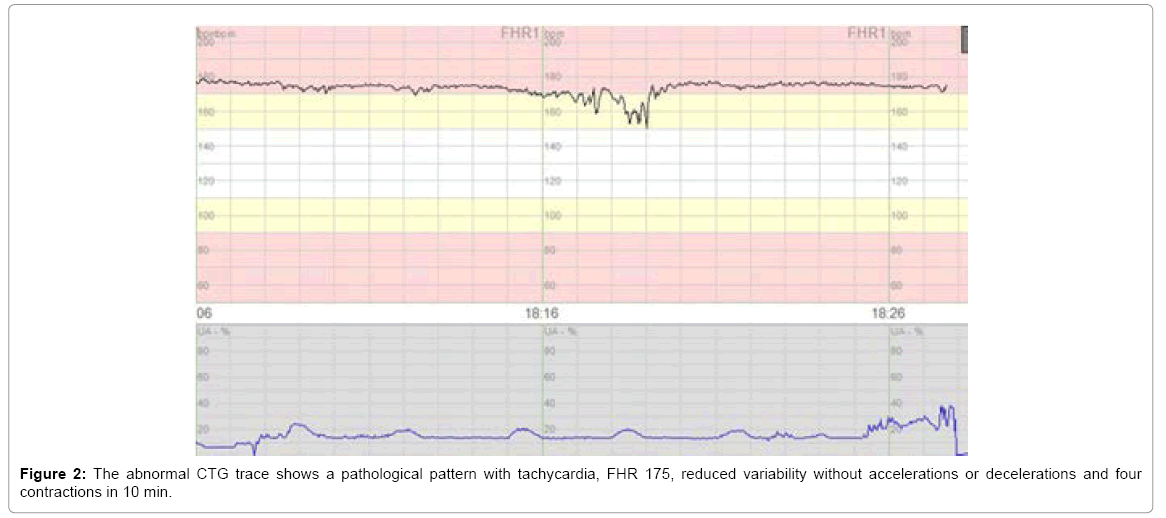
Later, the CTG graph (time 26.5 h after PROM) with a pathological pattern characterized by tachycardia, FHR (175 bpm), reduced variability without any acceleration and still no decelerations. There were four contractions of the uterus in 10 min. ½ h later, the CTG recorded one uncomplicated deceleration (loss of FHR greater than 60 bpm for less than 60 s). The cervix of the uterus was not fully dilated with cervical orifices measuring 3-4 cm, thus it was not possible to take a scalp blood lactate measurement and the scalp electrode could not be placed on the head of the fetus for internal monitoring of the FHR. The mother developed fever and the FW turned very thick, green and smelly. Chorioamnionitis was suspected and the mother was given antibiotics intravenously (Cefuroxime and Metronidazole). As a result of the pathological CTG over a period of 1 h (time 27 h and 45 min after PROM) and suspicious FW, a sub-acute caesarean section was performed (Figure 2).
The physical condition of the newborn was evaluated with the Apgar score according to colour, activity, pulse, respiration and reflexes, where a maximum of two points was given for each evaluation parameter [4]. The newborn was given eight points after one min (one point subtracted for both skin colour and activity), 10 points after five min and 10 points after ten min. The newborn had normal vital parameters including umbilical blood pH with 7.31 and base excess level at -4.1 mmol/L (arterial blood) and pH with 7.35 and base excess level at -3.2 mmol/L (venous blood), SaO2 93-98%, pulse, temperature and respiration.
Discussion
In our case, the fetus was heavily tachycardia with a baseline of 175 bpm and almost without variability and according to the guidelines in risk of acidosis [3]. However, despite a pathological CTG over a period of 1 h, the infant was not hypoxic after labor as would have been expected, but was delivered with a normal acid-base status, pH and vital values.
The fetus responded to the maternal infection by a state of hibernation, as it stopped responding to external stimuli and withdrew itself, shown by a pathological monotone heart rate pattern. It is necessary to recognize that a pathological CTG trace requires close attention to avoid the point at which the adaptive mechanisms of the fetus are failing. It is worth noting that the fetus in the present case was able to sustain a well-preserved metabolism, shown by the normal acidbase status, considering the pathological and uniform CTG (Figure 2).
It is already a well-known fact that Cardiotocography is essentially a test with high false positive rate and it is not rare that neonates with prenatal abnormal CTG findings do not show acidemia or hypoxemia.
It is the aim of intrapartum fetal monitoring to be able to early identify fetuses that are compromised and at risk for adverse outcomes [5]. However, interpretation of CTG data is subject to intra- and interobserver differences and it has not yet been possible to develop evidence-based CTG interpretation software that could support decision-making [6,7]. Consequently is becomes a medical challenge when the FHR becomes pathological and no longer reacts adequately to external stimuli. In order for a CTG to be considered reactive and normal, in the sense of determining whether the oxygen saturation of the fetus is sufficient, international guidelines prescribe a CTG with normal FHR baseline, variability and accelerations [3].
The phenomenon of fetal hibernation is not clearly described or studied in the literature. However, it is very important knowledge, when assessing if there is a need for invasive interventions during birth because interventions such as a caesarean section is associated with several risk factors for the mother and child. There is not yet agreement within the medical area on how to identify and describe the phenomenon of hibernation. We believe that this subject calls for attention in order to promote safe births for both mother and child.
Ethical Approval of Studies
The principles of the Helsinki Declaration were followed.
References
- Santo S, Ayres-de-Campos D, Costa-Santos C, Schnettler W, Ugwumadu A, et al. (2017) Agreement and accuracy using the FIGO, ACOG and NICE cardiotocography interpretation guidelines. Acta Obstet Gynecol Scand 96: 166-175.
- Colov NP, Hedegaard M, Hvidman L, Jørgensen JS, Lenstrup C (2008) Fosterovervågning under fødslen ved hjælp af STAN. Norske og danske STAN referencegruppe.
- Ayres-de-Campos D, Spong CY, Chandraharan E, Panel FIFMEC (2015) FIGO consensus guidelines on intrapartum fetal monitoring: Cardiotocography. Int J Gynaecol Obstet 131: 13-24.
- Committee on Obstetric Practice, American Academy of Pediatrics, Newborn CoFa (2015) Committee opinion no. 644: The apgar score. Obstet Gynaecol 126: e52-e55.
- Norén H, Amer-Wåhlin I, Hagberg H, Herbst A, Kjellmer I, et al. (2003) Fetal electrocardiography in labor and neonatal outcome: Data from the Swedish randomized controlled trial on intrapartum fetal monitoring. Am J Obstet Gynecol 188: 183-192.
- Noren H, Blad S, Carlsson A, Flisberg A, Gustavsson A, et al. (2006) STAN in clinical practice: The outcome of 2 years of regular use in the city of Gothenburg. Am J Obstet Gynecol 195: 7-15.
- Brocklehurst P, Field D, Greene K, Juszczak E, Kenyon S, et al. (2018) Computerised interpretation of the fetal heart rate during labour: A randomised controlled trial (INFANT). Health Technol Assess 22: 1-186.
Citation: Jensen LD, Grau J, Khalil MR (2018) Fetal Hibernation: A Case Report. J Preg Child Health 5: 372. DOI: 10.4172/2376-127X.1000372
Copyright: © 2018 Jensen LD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6801
- [From(publication date): 0-2018 - Dec 21, 2024]
- Breakdown by view type
- HTML page views: 6127
- PDF downloads: 674