Research Article Open Access
Feeding Practices and Morbidity Pattern of Infants in a Rural Area of Puducherry-A Follow Up Study
Srinivasan Vijayalakshmi*, Rajkumar Patil, Shib Sekhar Datta, Narayan KA and Fredrick StephenMahatma Gandhi Medical College and Research Institute Pondicherry, India
- *Corresponding Author:
- Srinivasan Vijayalakshmi
Assistant Professor
Mahatma Gandhi Medical College and Research Institute Pondicherry, India
Tel: 919788942682
E-mail: vijilakshmi121@gmail.com
Received date: June 26, 2014; Accepted date: August 18, 2014; Published date: August 25, 2014
Citation: Vijayalakshmi S, Patil R, Datta SS, Narayan KA, Stephen F (2014) Feeding Practices and Morbidity Pattern of Infants in a Rural Area of Puducherry-A Follow Up Study. J Community Med Health Educ 4:304. doi:10.4172/2161-0711.1000304
Copyright: © 2014 Vijayalakshmi S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
The feeding practices and illness during infancy are of critical importance for the growth and development of children. Though several programmes have been implemented by GOI along with WHO and UNICEF to improve the health status of newborns and infants, child morbidity and mortality rates in rural areas are still higher compared to urban areas in India. Objectives: To study the infant feeding practices, morbidity pattern and care given to infants in a rural area of Puducherry. Methodology: A longitudinal study done in Bahour commune from 1st April 2012 to 31st March 2013. Information regarding background/socio-demographic details, infant feeding practices; and morbidity pattern were recorded in semi-structured questionnaire by house to house visit. Total of 136 infants born during Jan-March 2012 were enrolled. Data were presented as percentages, ratios and Chi-square test was used to find association among variables. p value <0.05 was considered statistically significant. Results: The mean age of study infants during each visit was 3, 8 and 12 months respectively. 64.7% mother’s breastfed their infants within an hour after birth and 72% infants were exclusively breastfed till six months and 5.9% newborns were given prelacteal feed. The incidence of fever, diarrhoea and breathing difficulty were 2.9, 2.9 and 1.8 episodes/ child/ year respectively. On average 93% of mothers continued breastfeeding and gave excess oral fluid during an episode of diarrhoea. Morbidity among children was significantly associated with breastfeeding practices with exclusive breastfed children suffered less in the study area (p<0.05). Conclusions: The overall infant feeding pattern and care given during illness was good among mothers. However, Practices like giving pre-lacteal feed; stopping EBF before six months are still practiced in the study area. Therefore, faulty rearing practices need to be addressed to improve the health status of the infants.
Keywords
Infants; Feeding; Morbidity
Introduction
Infants are valuable treasure to the nation. Realizing the importance of child development, United Nations declared 1979 as the International Year of the Child (IYC) [1] and World Health Organisation (WHO) proposed a theme on World health day during 2003 as “Healthy environment for children” and 2005 as “Make every mother and child count” to focus the attention of planners, policy makers, administrators, health and social scientists on various problems faced by children [2].
Optimal infant and young child-feeding (IYCF) practice are crucial for nutritional status, growth, development, health and ultimately [3]. Breast milk is an important source of energy for infants and it provides immunity to fight against illness and reduce mortality. Exclusive breast feeding for six months is an essential component for growth and development of the infant [4]. For children older than six months, breast milk alone is no longer sufficient to meet the nutritional requirement and therefore other foods are needed along with breast milk. Introduction of semi-solid foods after first six months is essential to avoid the malnutrition in early life [5].
Globally seven million children, under five years of age died in 2011 and about one fourth (24%) of deaths occurred in India [3]. Around 86% of neonatal deaths are due to pneumonia, diarrhoea, and preterm births. As per WHO-Child Health Epidemiology Reference Group (CHERG) 2012 estimates, in India the major causes of child mortality in the age group 0–5 years in India are neonatal causes (52%), pneumonia (15%), diarrhoeal disease (11%), measles (3%), injuries (4%) and others (15%) [6].
Rationale of Study
Several programmes have been implemented by Government of India along with WHO and UNICEF to improve the health status of infants. Many customs are prevalent in India which affects health status of the infants. Understanding of the community and traditional practices of breastfeeding and care given during illness is necessary to implement the effective programme for promotion of new-borns and infant’s health. For the effective child health care delivery, information regarding infant feeding practices and pattern of morbidity is important. This study was done to describe selected newborn and infant feeding practices, morbidity pattern and care given during the episodes of illness in rural area of Puducherry.
Objectives
To study the infant feeding practices in a rural area of Puducherry To study the morbidity pattern and care given to infants during illness
Materials and Methods
The present study was conducted after getting clearance from Institutional Human Ethics Committee. This was a Community based longitudinal study done in the rural area over a period of one year from 1st April 2012 to 31st March 2013. Infants born to mothers during Jan- March 2012 were enrolled for the study through anganwadi registers from Bahour commune during April-June 2012. Total136 newborns were included in the study.
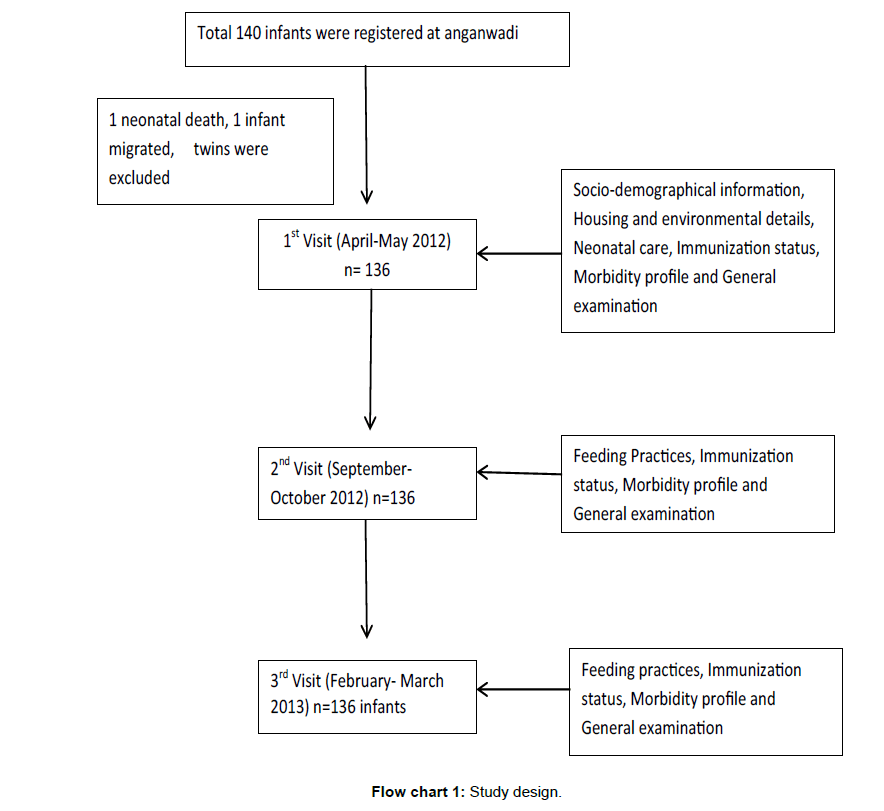
The investigator interviewed the mother in local language using a pre-designed proforma. Each infant-mother was interviewed for about 40 minutes. Mothers were informed through phone prior to each visit to be available in the houses and then house to house visit was done. Information about socio-demographic characteristics, feeding practices, occurrence and management of any childhood illness were collected. General examination was done to all infants (Flow chart 1).
Statistical Analysis
The data was entered and analyzed using Microsoft Excel. Data were presented as percentages and ratios. To find out association between infant care and rearing practices with socio-demographic characteristics and feeding practices, Chi-square test and Fisher’s exact p test were used. p-value <0.05 was considered as statistically significant.
Results
Total 136 infants’ mothers participated in the study. Among 136 infants, 63 (46.3%) were male and 73 (53.7%) were female. The mean age of the study infants was 2.8 ± 0.8 months, 7.9 ± 0.8 months and 12 month during first, second and third visits respectively.
Majority of the infants (94.9%) belonged to Hindu families. According to modified B.G. Prasad’s Classification for socio-economic status, 51 (37.5%) infants belonged to lower-middle class followed by 37 (27.2%) infants in poor class. Total 97 (71.3%) mothers were educated upto12th standard and 18 (13.2%) were graduate. Out of 136 mothers, 114 (83.8%) were housewives (Table 1). It was observed that, out of 136 infants, three (2.2%) did not receive colostrum for first two days after birth. Eight (5.9%) newborns were given prelacteal feed, among them five (62.5%) infants were given cow’s milk and three (37.5) were given honey water. Similarly, total 88 (64.7%) mothers breastfed their infants within an hour after birth, 38 (27.9%) were breastfed between one to six hours and ten (7.4%) were breastfed after six hours of delivery. Significant difference was observed between male and female newborns in terms of time of initiation of breastfeeding after birth (p=0.03). Demand feeding was practiced by 109 (80.1%) mothers, with 56 (88.9%) male newborns as compared to 53 (72.6%) female newborns being breastfed on demand (p=0.01) in the present study.
| Indicators | Male(n=63) | Female(n=73) | Total | p value |
|---|---|---|---|---|
| Colostrum discarded Yes No |
2 (3.2) 61 (96.8) |
1(1.4) 72 (98.6) |
3 (2.2) 133 (97.8) |
0.59 |
| Prelacteal feed given Yes No |
5 ( 7.9) 58 (92.1) |
3 (4.1) 70 (95.9) |
8 (5.9) 128 (94.1) |
0.34 |
| Type of prelacteal feed (n=8) Honey water Cow’s milk |
1(20) 4 (80) |
2 (66.7) 1 (33.3) |
3 (37.5) 5 (62.5) |
0.28 |
| Initiation of breastfeeding Within 1 hour 1-6 hours >6 hours |
47 (74.6) 11 (17.5) 5 (7.9) |
41 (56.2) 27 (37) 5 (6.8) |
88 (64.7) 38 (27.9) 10(7.4) |
0.03 |
| Breast fed on demand Yes No |
56 (88.9) 7 (11.1) |
53 (72.6) 20 (27.4) |
109 (80.1) 27 (19.9) |
0.01 |
| Exclusive breastfeeding <6 months >6 months |
12 (19) 51 (81) |
26 (35.6) 47 (64.4) |
38 (28) 98 (72) |
0.03 |
| Complementary feeding* Animal milk and milk products Boiled and smashed vegetables Fruits Cereals Egg Artificial feeds Chicken curry |
52 (82.5) 41 (65.1) 42 (66.7) 38 (60.3) 22 (34.9) 11 (17.5) 1 (1.6) |
60 (82.2) 55 (75.3) 41 (56.2) 44 (60.3) 35 (47.9) 11 (15.1) 0 |
112 (82.3) 96 (70.6) 83 (61) 82 (60.3) 57 (42) 22 (16.2) 1 (0.74) |
0.71 |
| Continued Breastfeeding at the time of third visit Yes No |
60 (95.2) 3 (4.8) |
61 (83.6) 12 (16.4) |
121 (89) 15 (11) |
0.03 |
Multiple answers, (Figures in parenthesis indicate percentages)
Table 1: Newborn feeding practices in the study area (N=136).
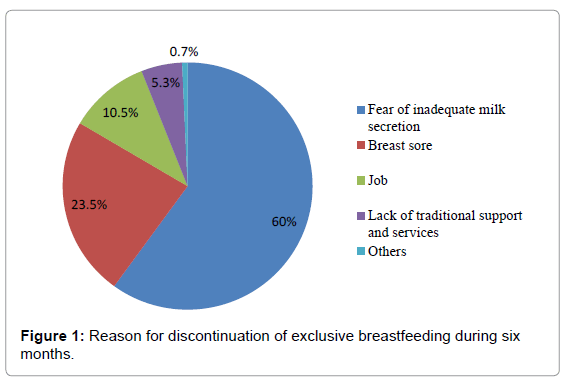
Out of 136 infants, 98 (72%) were exclusively breastfed for six or more than six months. Figure 1 shows that, 38 (28%) infants were not exclusively breastfed till six months, the major reasons stated by mothers include inadequate milk secretion (60%), breast sore (23.5%) and job of mothers (10.5%).
Regarding nature of complementary feeding, majority (82.3%) of the mothers used animal milk and milk products, 92 (70.6%) used boiled and smashed vegetables and nearly 80 (60%) mothers gave fruits and cereals. Majority (89%) of the mothers continued breastfeeding till the end of one year. Significant difference was observed between male and female infants when continuation of breastfeeding at the end of one year was considered (p=0.03) (Figure 2).
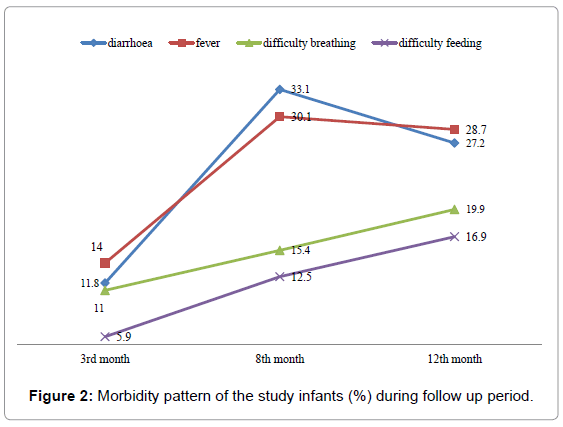
Table 2 shows the morbidity status of study infants during each visit. It was observed that, during first visit, out of 136 infants, 19 (14%) infants had fever followed by diarrhoea (11.8%) and difficulty in breathing (11%). During second visit, 45 (33.1%) infants had diarrhoea followed by fever (33.8%) and difficulty in breathing (15.4%). During third visit, 39 (28.7%) infants had fever and 37 (27.2%) suffered from diarrhoea.
| Morbidity | First visitN (%) | Second visitN (%) | Third visitN(%) | Episode per child per year |
|---|---|---|---|---|
| Diarrhoea | 16 (11.8) | 45 (33.1) | 37 (27.2) | 2.88 |
| Dysentery | 2 (1.5) | 1 (0.7) | 2 (1.5) | 0.15 |
| Fever | 19 (14) | 41 (30.1) | 39 (28.7) | 2.91 |
| Difficulty in breathing | 15 (11) | 21 (15.4) | 27 (19.9) | 1.85 |
| Difficulty in feeding | 8 (5.9) | 17 (12.5) | 23 (16.9) | 1.41 |
| Convulsion | 2 (1.5) | 4 (2.9) | 1 (0.7) | 0.20 |
Table 2: Morbidity status of study infants during follow up period.
The incidence of fever was high among infants with 2.91 episodes per child per year. The incidence of diarrhoea and breathing difficulty among study infants was 2.88 and 1.85 episodes per child per year respectively.
Figure 2 shows the morbidity status of study infants during the follow up period. It was observed that, 33.1% of the study infants had diarrhoea during second visit (mean age 8 months), as compared to 11.8% and 27.2% children respectively during first (average age 3 months), and third visit (average age 12 months). About 30.1% of the study infants had fever during second visit as compared to 14% and 28.7% children respectively during first and third visits.
A higher level of morbidity was observed during second visit among study infants followed by morbidity during third and first visit.
Table 3 shows care of sick infants during illness. It was observed that, more than 90% of mothers had given continued feeding with extra oral fluid during the episodes of diarrhoea in all visits. During the study period, total 40 (83.3%) infants were taken to a hospital for difficulty in feeding and 66 (66.7%) children sought consultation during an episode of fever. 52 (82.5%) infants out of 63 were given an antibiotic for difficulty breathing.
| Indicators | First visitN (%) | Second visit N(%) | Third visitN (%) | Total |
|---|---|---|---|---|
| Had feeding difficult and taken to a hospital | 7 (87.5)(n=8) | 15 (88.2)(n=17) | 18 (78.3)(n=23) | 40 (83.3)(N=48) |
| Consultation during an episode of fever | 15(78.9)(n=19) | 30 (73.1)(n=41) | 21 (53.8)(n=39) | 66 (66.7)(N=99) |
| Convulsion and taken to a hospital | 2 (100)(n=2) | 3(75)(n=4) | 1(100)(n=1) | 6 (85.7)(N=7) |
| Had difficulty breathing and given an antibiotic | 10 (66.7)(n=15) | 18 (85.7)(n=21) | 24 (88.9)(n=27) | 52 (82.5)(N=63) |
| Continued feeding and given extra fluid orally during an episode of diarrhoea | 17 (94.4)(n=18) | 42 (91.3)(n=46) | 37 (94.8)(n=39) | 96 (93.2)(N=103) |
| Blood in stool and taken to a hospital | 2(100)(n=2) | 1(100)(n=1) | 1(50)(n=2) | 4 (80)(N=5) |
Table 3: Care given to sick infants during illness.
Table 4 shows association of feeding practices and morbidity pattern of study infants. Out of eight infants who were given prelacteal feed, seven (87.5%) had diarrhoea during the study period. In the present study, out of 38 infants who did not receive exclusive breastfeeding till six months, 28 (73.7%) had one episode of diarrhoea during the study period, as compared to 34 (34.7%) who received EBF till six months. Significant association were observed between prelacteal feeding (p=0.01), EBF (p<0.001) and infants suffering from at least one episode of diarrhoea.
| Characteristics* | Pre-lacteal feeding | EBF | Continued breastfeeding till one year | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes (n=8) |
No (n=128) |
p-value | <6 months (n=38) |
≥6 months (n=98) |
p-value | Yes (n=121) |
No (n=15) |
p-value | |
| Diarrhoea Yes(n=62) No(n=74) |
7 (87.5) 1 (12.5) |
55 (43) 73 (57) |
0.01 | 28 (73.7) 10 (26.3) |
34 (34.7) 64 (65.3) |
<0.001 | 54 (44.6) 67 (55.4) |
8 (53.3) 7 (46.7) |
0.52 |
| Difficulty in breathing Yes(n=53) No(n=83) |
5 (62.5) 3 (37.5) |
48 (37.5) 80 (62.5) |
0.26 | 18 (47.4) 20 (52.6) |
35 (35.7) 63 (64.3) |
0.21 | 46 (38.1) 75 (61.9) |
7 (46.7) 8 (53.3) |
0.51 |
| Fever Yes(n=72) No(n=64) |
6 (75) 2 (25) |
66 (51.6) 62 (48.4) |
0.19 | 23 (60.5) 15 (39.5) |
49 (50) 49 (50) |
0.27 | 60 (49.6) 61 (50.4) |
12 (80) 3 (20) |
0.02 |
*Number of infants had at least one episode of illness during all three visits
Table 4: Association of feeding practices and morbidity pattern.
Out of 15 infants who did not continue breastfeeding till one year, 12 (80%) had one episode of fever during the study period. Significant difference was observed between continued breastfeeding till one year and infants suffering from at least one episode of fever (p=0.02).
Discussion
The present longitudinal study aimed at assessing the infant feeding practices and morbidity pattern in a rural area of Puducherry. This study described the feeding practices, common morbidities and examined their association.
Early initiation of breastfeeding, exclusive breastfeeding for six months and timely introduction of age-appropriate complementary feeding are the key interventions to achieve the Millennium Development Goal 1 and 4, which address child malnutrition and mortality components respectively [7].
Pre-lacteal feeding is almost universal in India; many studies indicate that mothers delay the breastfeeding for several hours to avoid giving colostrum and supplement breastfeeding with other foods or liquids. However, present study observed that percentage of infants who were given prelacteal feed was only 5.9%. Among them 62.5% were given animal’s milk as pre-lacteal feed and 37.5% infants were given honey water. The practice of giving pre-lacteal feed is observed in many countries also. Studies from rural Egypt, South Nepal and Pakistan [8-10] reported that the percentage of newborns that were given pre-lacteal feeds was 44%, 55.6% and 87.6% respectively, which were higher compared to the present study. Studies from other parts of India also reported the practice of giving prelacteal feeds [11-14].
Pre-lacteal feed to a newborn delay the establishment of lactation and also contamination of pre-lacteal food can cause diarrhoea in the newborn [15]. In the present study, association was observed between feeding practices and prevalence of diarrhoea among study infants (p=0.01). Out of eight infants who were given pre-lacteal feed, 87.5% had diarrhoea. It was also observed that, out of 38 infants who were not exclusive breastfeed till six months, 73.7% infants had one episode of diarrhoea during the study period, as compared to 34.7% infants who received EBF till six months. This shows that the exclusively breastfeeding offers the protective effects to the infants in preventing diarrhoea.
Colostrum is a thick, yellow secretion from the breast during initial two to three days after delivery. It is considered as nectar for the newborn. It provides a concentrated source of energy for the newborn which is easily digestible and also offers protection against childhood illnesses [5]. In the present study, 2.2% newborns did not receive colostrum even after two days of birth. Similar observations were reported from two studies conducted in Bangalore [13,14]. However, studies from other regions of India and other countries also showed even higher percentage of mothers discarding colostrum for first two days [10,14,16-18].
According to Infant and Young Child Feeding Practices (2006) guidelines in India, it is recommended that initiation of breastfeeding should begin immediately after birth. In the present study initiation of breastfeeding within one hour after birth was 64.7% and within 24 hours was almost 97%. Initiating breast-feeding within one hour was similar to DLHS-3 [19] findings for Pondicherry rural area (67.2%) and other studies conducted in Uttar Pradesh and rural Wardha [16,20]. However, our observations are more than the national and Tamil Nadu figures as per DLHS-3 [19] and NFHS-3 [21]. Mothers belonging to high socio-economic class families had better knowledge related to initiation of breastfeeding. Findings in regard to initiation of breast feeding in the present study was higher than studies reported from other states of the country and this could be attributed to high level of female literacy, effective antenatal advices to mothers and frequent postnatal visits by healthcare providers leading to increased knowledge regarding early initiation of breastfeeding and the importance of colostrum.
IMNCI recommends on-demand breastfeeding or feeding 8 times or beyond to the newborn [22]. In the present study it was observed that, majority of the mothers breastfed their infants on demand (80.1%), similar to the observations made by Joseph et al. [14] in Bangalore (87%) and Bandyopadhayay S K et al. in West Bengal [23].
There were also some other studies which have shown a demand breastfeeding with the range from 70% to 90% [24,25]. Early introduction of complementary feeding increases the risk of infection in infant. The national figures for EBF rates in NFHS-3 [21] and DLHS-3 [19] were 48.3% and 48.1% at 5 months respectively. However in the present study it was observed that, exclusive breastfeeding was 72%, which was higher than national figures and nearly equal to DLHS-3 [19] for Pondicherry (66%) and Tamil Nadu (68%) [19]. Studies conducted in Haryana, Karnataka, Bangalore, West Bengal observed lower rates for exclusive breastfeeding being 20.2%, 57.1%, 40% and 57.9% respectively [13,14,23,26].
The major reasons cited by mothers for not breastfeeding their child exclusively till six months were fear of inadequate milk secretion, presence of breast sore, lack of traditional support and time constraints for professional mothers.
Significant association was observed between gender of the newborns and initiation of breastfeeding, on-demand feeding, exclusively breastfeeding till six months and continuation of breastfeeding till one year.
One of the important strategies of IMNCI is to reduce the underfive mortality is educating the mother and/or caregiver regarding home-based care of the child during illness and after recovery [22]. The mother and/or care giver should be counselled for signs of severe illness for which the child should be taken immediately to a health worker. NFHS-3 [21] reported 15.1% children less than three years had fever two weeks preceding the survey which was higher than the present study (12%). However, in the present study, 66.7% mothers sought consultation for their infants from hospital during for fever which was lower than DLHS-3 for Puducherry (84.8%) [19].
According to NFHS-3 [21], 24% of all children had diarrhoea in rural area of India which was similar to the present study (24.03%). Studies from other parts of the country also reported prevalence of diarrhoea which ranges from 11% to 35% [27,28]. In the present study, more than 90% of mothers given continued breastfeeding and feeding with excess oral fluid during the episodes of diarrhoea in all visits indicating high awareness regarding home-care management of diarrhoea among mothers and high healthcare coverage in the study area.
Incidence of infants with breathing difficulty was lower in present study than other studies [27,28]. Majority of the infants (82.5%) sought treatment for breathing difficulty in present study. In the present study, incidence rate of diarrhoea was 2.9 episodes per child per year. Similar observations was made in systematic review done by Fischer et al. [27] from low and middle income countries. (2.9 episodes/child/year) [27].
Conclusion
EBF (72%) and on-demand feeding 80.1%. Majority (89%) of the mother continued breastfeeding at one year.Mothers adopted home care practices during their infant’s illness. Exclusive breastfeeding till 6 months was less among working mothers as compared to housewives. Faulty feeding practices like discarding the colostrum’s was significantly more among mothers from low socio-economic background.On average 93% of mothers continued breastfeeding and gave the newborn excess oral fluid during an episode of diarrhoea. The infants who were not exclusively breastfeed till six months were more prone for diarrhoea compared with infants who were exclusively breastfed till six months. A higher level of morbidity was observed during second visit among study infants followed by morbidity during third and first visit.
References
- UNICEF (1979) The Year of the Child. New York
- World Health Organization (2013)Previous World Health Days
- World Health Organization (2011) Neonatal mortality rate
- Sample Registration System (2013) SRS Bulletin: Census and Vital Statistics. India: Ministry of Home Affairs
- World Health Organization (2013) Essential Nutrition Actions: improving maternal, newborn, infant and young child health and nutrition.
- WHO, CHERG (2013) Major causes of child mortality in the age group of 0-5 years in India. http://www.who.int/pmnch/topics/part_publications/country_profiles.pdf
- Government of India (2011) Millennium Development Goals India country report 2011. New Delhi: Central Statistical Organisation
- Darmstadt GL, Hussein MH, Winch PJ, Haws RA, et al (2007)Neonatal home care practices in rural Egypt during the first week of life.Trop Med Int Health 12: 783-797
- Karas DJ, Mullany LC, Katz J, Khatry SK, LeClerq SC, et al (2012) Home care practices for newborns in rural southern Nepal during the first 2 weeks of life. J Trop Pediatr58: 200-207.
- Khadduri R, Marsh DR, Rasmussen B, Bari A, Nazir R et al (2008) Household knowledge and practices of newborn and maternal health in Haripur district, Pakistan. J Perinatol 28:182-187.
- Das P, Ghosh S, Ghosh M, MandalA (2008)A study on delivery and newborn care practices in a rural block of West Bengal.Indian J Public Health 52:159-160
- Meshram II, Arlappa N, Balakrishna N, MallikharjunaRao K, Laxmaiah A, et al (2012) Trends in the prevalence of undernutrition, nutrient and food intake and predictors of undernutrition among under five year tribal children in India. Asia Pac J ClinNutr 21:568-576.
- Kumar N, Unnikrishnan B, Rekha T, Mithra P, Kulkarni V, et al (2012) Infant feeding and rearing practices adapted by mothers in coastal South India. Indian J Colla Res Int Med &Publ Health 4:1-12.
- Joseph N, Unnikrishnan B, Naik VA, Mahantshetti NS, Mallapur MD, et al (2013) Infant rearing practices in South India: A Longitudinal study. J Fam Med &Pri Care 2:37-45
- WHO, UNICEF (2011) Operational guide enhancing optimal infant and young child feeding practices through the public health system
- Thakur N, Kumar A (2012)A study on delivery and newborn care practices in urban slums. Antrocom online J of Anthropology
- Bang AT, Bang RA,Baitule S, Deshmukh M, Reddy H (2001) Study on burden of morbidities and unmet need for health care in rural neonates. Indian Pediatric Journal38:956-965.
- Madhu K, Chowdary S, Masthi R (2009) Breast Feeding Practices and Newborn Care Practices in a Rural Block of West Bengal. Indian J Public Health 34: 243-246
- International Institute for Population Sciences (2010) District Level Household and Facility Survey
- Dongre AR, Deshmukh PR, Rawool AP, Garg BS (2010) Where and how breastfeeding promotion initiatives should focus its attention? A study from rural wardha. Indian J Community Med 35:226-229.
- National Family Health Survey India.
- National Institute of Health and Family Welfare
- Bandyopadhayay SK, Chaudhury N, Mukhopadhyay BB (2000) Breastfeeding practices in rural areas of West Bengal. Indian J Public Health 44: 137-138.
- Bhosale NA, Deshpande SG, Zodpey SP, Jog SN, Vasudeo ND (1997) Infant feeding practices- a clinic based study. Indian J Med Sci 5: 396-399.
- Bhandari NR, Patel GP (1973) Dietary and feeding habits of infants in various socio economic groups. Indian J Peditr 10: 233-238
- Upadhyay RP, Rai SK, Anand K (2012) Community neonatal practices and its association with skilled birth attendance in rural Haryana, India. ActaPaediatr 101: 535-539
- Fischer Walker CL, Perin J, Aryee MJ, Pinto BC, Black RE (2011) Diarrhoea incidence in low- and middle-income countries in 1990 and 2010: a systematic review. BMC Public Health. 2012 Mar 21; 12: 220. 59 Sutariya S, Talsama N, Shah C. Study of prevalence of diarrhoeal diseases in Ahmadabad. National J of Community Medicine 2: 96-99.
- Abhay BM, Dohare S, Gitte SV (2012) Child health: Understanding the home care practices in some illness among under five children in IMNCI implementation area. Int J Biol Med Res 2: 1251-1254
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 16543
- [From(publication date):
September-2014 - Nov 27, 2024] - Breakdown by view type
- HTML page views : 11926
- PDF downloads : 4617