Review Article Open Access
Family Medicine in Saudi Arabia-Next Steps
Richard B Birrer*, Al-EnazyH and Sarru EDepartment of Medicine, St. Joseph’s University Medical Center, USA
- *Corresponding Author:
- Richard B Birrer
Department of Medicine
St. Joseph’s University Medical Center, USA
Tel: 516-671-6751
E-mail: rbbirrer@yahoo.com
Received date: February 19, 2014; Accepted date: March 17, 2014; Published date: March 19, 2014
Citation: Birrer RB, Al-Enazy H, Sarru E (2014) Family Medicine in Saudi Arabia- Next Steps. J Community Med Health Educ S2:005. doi: 10.4172/2161-0711.S2-005
Copyright: © 2014 Birrer RB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
The increased prevalence of communicable, non-comunicable diseases, the global expanding of the elderly population, significant mental health issues,rising health costs,overutilization and medicalization of illnesses necessitate the need for a reliable community-based health care team. Efforts towards efficient, well organized family medicine speciality programs will produce needed, commited, and skilled primary care or family physicians that qualify them to provide continuous, comprehensive and accountable evidence-based health care for patients of all age groups. The Saudi Aramco Medical Services Organization (SAMSO), the first JCIA accredited hospital in the Middle East has taken significant strides to address the challenges facing the family medicine discipline.We aim through the following review to emphasize the role of family physicians, highlight some challenges globally and in Saudi Araba and provide list ofgeneral recommendations that would support the model.
Keywords
Communicable and non-communicable diseases; Family medicine; Primary care; JCIA (Joined Commision International Accreditation); Saudi Aramco Medical Services Organization (SAMSO); Saudi Arabia
Introduction
Non-communicable diseases like cardiovascular (e.g., coronoray artery disease, hypertension, stroke), chronic respiratory diseases (e.g., chronic obstructive pulmonary diseases and asthma), diabetes mellitus and cancer are responsible for 63% of all death world-wide. 80% of non-communicable diseases occur in low-middle income countries and in people less than 60 years of age (WHO) [1,2]. Most of noncommunicable and communicable diseases can be prevented through effective interventions like standard infection precautions, judicious use of antimicrobials, smoking cessation, healthy diet, physical activity and evidence-based community cancer screening programs.
Primary care is the provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs through the development of a sustained partnership with patients and practicing in the context of family and community. The guiding principles of primary health care are ready accessibility to care, public participation, home care, health education and application of evidence-based medical care for acute and chronic conditions to all age groups [2]. Societies in in the Middle East struggle for a preferred model of primary care and a sufficient numbers of certified family medicine specialists in a world where Western subspecialization is the dominant model.
The current review highlights the importance of developing and cultivating strong family medicine programs and providing healthcare practice opportunities and systems that leverage the strengths of the cost-effective model.
Is There a Preferred Model of Primary Care?
The Institute of Medicine in 1978 and 1994 defined the essential elements of primary care: accessibility, accountability, affordability, coordination, continuity and comprehensive care. Accessibility and continuity of physician care is associated with more positive outcomes and appears to be particularly important for more vulnerable patients [3-6]. Comprehensive care emphasizes the uniqueness of the whole person as opposed to emphasizing an organ system. Accountability and coordination of care assure that there is one person ultimately responsible for the patient’s care [7,8].
Of the primary care specialties (i.e., internal medicine, pediatrics, obstetrics-gynecology and family medicine) only the latter fulfills these criteria the best since the entire family is cared for-both genders and all age groups for across all body systems whether acute and chronic illness. The panel population is heterogeneous. Physician extenders (e.g., nurse practitioners, physician assistants) can also provide primary care along this continuum. Family physicians provide a unique role in public health including disease prevention, health promotion and the provision of medical care for urgencies or emergencies. As the most versatile example of primary care, the availability of family medicine physicians is associated with improved health outcomes and life expectancy and reduces all-cause cancer, heart disease, stroke and infant mortality rates. The specialty’s impact on mental health is significant as family dynamics often plays a significant role in chronic illness. Psychotherapeutics is fundamental in the treatment approach [9]. The ‘tenured’ family relationship results in less fragmented care and division of responsibility, lower referral and consultation rates, lower laboratory and imaging utilization and less prescriptions [10]. The focus is on the whole person in the context of the unit of care, the family, rather than disease management. The result is a strong physician-patient relationship promoting an improved quality of life [11].
Challenges Facing Family Medicine
A work force report by American Academy of Family Physicians projected the need for 139,531 family physicians by 2020 in order to meet the need for primary medical care. However, current USA based residency programs only attract half of needed family physicians. The Arab world needs more than 160,000 family physician specialists; however, what is available is far less than that number [12]. The majority of graduates in the Arab world work in clinical practice, with predominance of specialized care over primary care health services and tendency to be centralized in urban areas [13].
A growing number of US-based family physicians have become surrogate internists, caring for a pool of only adult patients. Additionally, the skills and knowledge base in obstetrics are quietly being eroded and with it care of the newborn. Procedural skills are often deferred to the referring subspecialist. Remuneration in healthcare emphasizes procedures rather the time intense bedside skills of cognitive behavioral therapy, family therapy, marriage counseling etc. lastly, the specialty is not promoted on par with other specialties, making it appear as a second tier or class specialty [14].
What is the Impact of Primary Care?
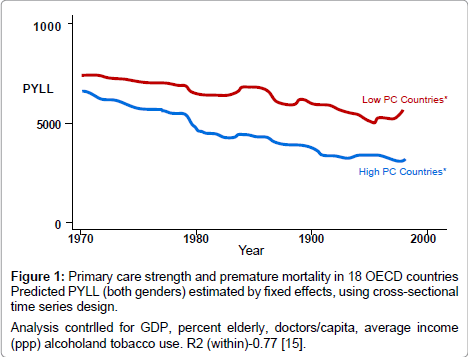
Pooled results for all-cause mortality suggest that an increase of one primary care physician/10,000 population is associated with average mortality reduction of 5.3% or 49/100,000 (Figure 1) [15].
Figure 1: Primary care strength and premature mortality in 18 OECD countries Predicted PYLL (both genders) estimated by fixed effects, using cross-sectional time series design.
Analysis contrlled for GDP, percent elderly, doctors/capita, average income (ppp) alcoholand tobacco use. R2 (within)-0.77 [15].
A similar significant trend has been found in those countries using a strong primary care base versus those countries without the model (Table 1) [16].
| Age 40 | Age 65 | Age 80 | ||||
| Female | Male | Female | Male | Female | Male | |
| Wors primary care (Belgium, France, Germany, and USA*) |
7.8 | 9.5 | 8.0 | 8.0 | 7.4 | 6.9 |
| Better primary care (Australia, Canada, Japan, Sweden, Denmark, Finland, Netherlands, Spain, UK**) |
6.7 | 5.9 | 6.6 | 6.6 | 6.8 | 7.1 |
indicate better performance.
**England and Wales only.
Table 1: Average rankings* for life expectancy at ages 40, 65 and 80 for countries grouped by primary care orientation.
In England, each additional primary care physician per 10,000 (about a 20% increase) is associated with a decrease in mortality of about 5%, adjusting for limiting long-term illness and for various demographic and socioeconomic characteristics [17]. In the United States similar results have been identified and the impact is greatest if the primary care model is based on family medicine. For each additional family physician per 10,000 population there is a 9% decrease in mortality [18-20]. Primary care in adults has been associated with a 33% reduction of health care cost while at the same time a 19% decrease in mortality [21]. A 10% increase in the supply of primary care physicians is associated with a 4% increase of diagnosing early stage breast cancer [21]. In a regression analyses that adjusted for sociodemographic characteristics, each one-third increase in the supply of family physicians decreased the incidence of invasive cervical cancer by 10% and its mortality by 20%. Similar trends have been noted for melanoma and cervical and colorectal cancers [22-24]. In a large meta-analysis spanning fifteen years the total and individual mortality rates for infants, cancer, heart and stroke were lower the higher the penetration of primary care physicians, whereas the mortality rates increased the higher the specialist ratio [19].
In 2000 an estimated 5 million admissions to US hospitals, with a resulting cost of more than $26.5 billion, may have been preventable with high quality primary care.
Assuming that an average hospital stay costs $5,300 per admission, even a modest 5 percent decrease in hospitalizations for these ambulatory care sensitive conditions would save more than $1.3 billion in inpatient costs [25]. Increasing the number of primary care physicians by 1 per 10,000/population will reduce inpatient admissions by 5.5%, outpatient visits by 5%, emergency department visits by 10.9% and surgeries by 7.2 % [26]. There are similar global trends. Healthcare reform in Bolivia lowered the mortality rates for under-5 years to rates similar to industrialized countries by emphasizing a primary care model. In Costa Rica, primary care reforms in the 1990s decreased the infant mortality and increased life expectancy to rates comparable to those in developed countries.In Mexico improvements in primary care practices reduced child mortality in socially deprived areas [27-30]. A well-integrated primary care experience is associated not only with improved self-rated overall and mental health but also with reductions in disparities between more- and less-disadvantaged communities in ratings of overall health [31].
Additional benefits of primary care include improved satisfaction with communication [32,33], enhanced patient confidence, increased trust and treatment compliance [34], better integration of preventive and proactive care [35], fewer readmissions [36] and usage of emergency services [37], more efficient use of resources [5,13,38,39], fewer adverse treatment effects [40-42] and lower costs [43].
What is the Kingdom’s Position on Primary Care?
In Saudi Arabia there are nine recognized family medicine residency programs. In 1983 Saudi universities started the post graduate family medicine program, and 10 years later (1993) the Saudi Family Medicine Fellowship Program started [44]. Albar pointed out that 90% of the 10,000 physicians working in Saudi primary care sector are non-Saudis and majority of them are not certified in family medicine [44]. However, Albar reflected an active strategy towards certifying 3,000 family physicians by 2020, and AlKhoja emphasized the already existing Saudi accreditation program in primary health care and family medicine [12].
In 2008 the Ministry of Health agreed to develop the necessary policies for the promotion of the family medicine concept. It further set forth to establish a positive image for the role of primary health care centers. Since then there has been a shift in the approach by replacing primary health centers with family and community medicine. It is felt that this will ensure improved health services through the integration of standard therapeutics and prevention, particularly for high risk communities and special groups like children, pregnant females and the poor.
What is SAMSO Care Partners Doing About This Challenge?
SAMSO’s care model is referred to as Care Works. Currently, all patients are assigned to a primary care physician. Every effort is made to assign the entire family to a family physician whenever possible, respecting culture mores and the availability of family physicians. SAMSO has been 70% successful in this regard but the target is 100%. Until recently, there were no Saudi medical students sent for training in family medicine. 50% of candidates are now selected for this type of residency because of its cultural appeal and cost-efficacy. Furthermore, a decision was made to require board certification in all primary care specialties within three years of completion of the training program.
The primary care physician leads the patient family-centered care model by working directly with a nurse, pharmacist, educator, social worker and scheduler in order to streamline continuity and coordination of the patient’s care. Because ‘form follows function’ the design of the practice sight is being re-engineered to provide swing rooms for all physicians.A telephone triage and consultation system will shortly be added which will provide improved satisfaction and care, particularly after hours. Primary care physicians are also encouraged to be involved with their patients who require admission and in-patient care. Lastly, home visits, where appropriate, are utilized. Well established evidencebased guidelines are used for acute (e.g., pharyngitis, sinusitis, otitis media etc.) as well as chronic (e.g., congestive heart failure, chronic obstructive pulmonary disease, community acquired pneumonia etc.) diseases and provide the basis for continuous quality improvement.
Key Recommendations
1. Primary care delivery systems, built on the family practice model, should be aggressively developed that will make the services available to all citizens. Physician as well as physician extender models (nurse practitioners, physician assistants) should be addressed.
2. Insurance coverage should be provided to all citizens so that the benefits of primary care are more uniformly available.
3. Because the quality, efficiency, and responsiveness of primary care are enhanced by the use of interdisciplinary teams the adoption of the team concept of primary care should be emphasized wherever possible.
4. Primary care should be made available to all underserved groups and communities with special needs.
5. Health promotion and disease prevention activities should be a critical element of primary care services.
6. Financial and regulatory barriers to the practice of primary care should be reduced or removed as much as possible, particularly in the areas of long-term care and mental health.
7. Uniform methods and measures to monitor the performance of health care systems and individual clinicians in delivering primary care should be developed and monitored. Performance measures should include cost, quality, access, and patient and clinician satisfaction. The results should be made available to public and purchasers of care, provider organizations, clinicians, and the general public.
8. Academic health institutions should explicitly accept primary care as one of their core missions and provide leadership and positive role modeling in the development of primary care teaching, research, and service delivery programs. The specialty of family medicine should be premiered with departmental status.
9. All medical schools should require their undergraduate medical students to experience training in settings that deliver primary care, especially family medicine.
10. Common core competencies for primary care clinicians, regardless of their disciplinary base, should be defined by a coalition of appropriate educational and professional organizations and accrediting bodies.
11. The Ministry of Health (MOH) or designated organization should accredit primary care training programs and support curricular reforms that teach the common core competencies and essential elements of primary care.
12. The training of primary care clinicians should include experience with the delivery of health care by interdisciplinary teams; and academic health centers should liaise with health maintenance organizations, group practices, community health centers, and other health care delivery organizations using interdisciplinary teams to develop clinical rotations for students and residents.
13. The MOH should identify a lead agency for primary care research and appropriate funds for this agency in an amount adequate to build both the infrastructure required to conduct primary care research and fund high-priority research projects, including the development of and provide ongoing support for a national database (based on a sample survey) that reflects the majority of health care needs in the Kingdom and includes a uniform primary care data set based on episodes of care. This national survey should capture data on the entire population, regardless of insurance status.
14. A public-private, nonprofit primary care consortium consisting of professional societies, private foundations, government agencies, health care organizations, and public representatives should be formed to monitor progress in primary care including distribution, mixand competency of the workforce.
Conclusion
Family medicine as a disciplinecontinues to struggle globally for its rightfull place in the pantheonl of health care professions.The challenges differ among countries due to several variables; however, research is beginning to identify the benefits andimpact of primary care and family physicians. The specialty of family medicine needs rigorous developing and nurturing globally, especially in the Middle East where family and community are strong. Governments and health care authorities must see the model as the keystone for a proficient health care system.
References
- World health organization (2007) People at the center of health care: harmonizing mind and body, people and systems.
- The World Health Report (2008) Primary Health Care (Now More Than Ever).
- Institute of Medicine (1978) A Manpower Policy for Primary Health Care: Report of a Study. Washington DC: National Academy of Sciences.
- Institute of Medicine (1994) Defining Primary Care: An Interim Report. Washington DC: National Academy Press.
- Weinick RM, Zuvekas SH, Cohen JW (2000) Racial and ethnic differences in access to and use of health care services, 1977 to 1996. Med Care Res Rev 57 Suppl 1: 36-54.
- Forrest CB, Starfield B (1998) Entry into primary care and continuity: the effects of access. Am J Public Health 88: 1330-1336.
- Donaldson MS, Yordy KD, Lohr KN, Vanselow NA (1996) Primary Care. America's Health in a New Era. Committee on the Future of Primary Care. Division of Health Care Services. Institute of Medicine.
- Meyers DS, Clancy CM (2009) Primary care: too important to fail. Ann Intern Med 150: 272-273.
- Gulbrandsen P, Hjortdahl P, Fugelli P (1997) General practitioners' knowledge of their patients' psychosocial problems: multipractice questionnaire survey. BMJ 314: 1014-1018.
- Woodward CA, Abelson J, Tedford S, Hutchison B (2004) What is important to continuity in home care?. Perspectives of key stakeholders. SocSci Med 58: 177-192.
- Ferrer RL, Hambidge SJ, Maly RC (2005) The essential role of generalists in health care systems. Ann Intern Med 142: 691-699.
- WONCA News An international forum for Family Doctors.
- Osman H, Romani M, Hlais S (2011) Family medicine in Arab countries. Fam Med 43: 37-42.
- Brown DC (1979) Family Practice-What's the Difference? Can Fam Physician. 25: 1487- 1521.
- Macinko J, Starfield B, Shi L (2003) The contribution of primary care systems to health outcomes within Organization for Economic Cooperation and Development (OECD) countries, 1970-1998. Health Serv Res 38: 831-865.
- Starfield B, Shi L (2002) Policy relevant determinants of health: an international perspective. Health Policy 60: 201-218.
- Starfield B, Shi L, Macinko J (2005) Contribution of primary care to health systems and health. Milbank Q 83: 457-502.
- Gulliford M, Figueroa-Munoz J, Morgan M, Hughes D, Gibson B, et al. (2002) What does 'access to health care' mean? J Health Serv Res Policy 7: 186-188.
- Shi L, Macinko J, Starfield B, Wulu J, Regan J, et al. (2003) The relationship between primary care, income inequality, and mortality in US States, 1980-1995. J Am Board FamPract 16: 412-422.
- Franks P, Fiscella K (1998) Primary care physicians and specialists as personal physicians. Health care expenditures and mortality experience. J FamPract 47: 105-109.
- Ferrante JM, Gonzalez EC, Pal N, Roetzheim RG (2000) Effects of physician supply on early detection of breast cancer. J Am Board FamPract 13: 408-414.
- Roetzheim RG, Pal N, van Durme DJ, Wathington D, Ferrante JM, et al. (2000) Increasing supplies of dermatologists and family physicians are associated with earlier stage of melanoma detection. J Am AcadDermatol 43: 211-218.
- Roetzheim RG, Pal N, Gonzalez EC, Ferrante JM, Van Durme DJ, et al. (1999) The effects of physician supply on the early detection of colorectal cancer. J FamPract 48: 850-858.
- Campbell RJ, Ramirez AM, Perez K, Roetzheim RG (2003) Cervical cancer rates and the supply of primary care physicians in Florida. Fam Med 35: 60-64.
- Kruzikas DT, Jiang HJ, Remus D et al (2004) Preventable hospitalizations. A Window into primary and preventive care. HCUP Fact Book No. 5. 1-64.
- Kravet SJ, Shore AD, Miller R, Green GB, Kolodner K, et al. (2008) Health care utilization and the proportion of primary care physicians. Am J Med 121: 142-148.
- Perry H, Robison N, Chavez D, Taja O, Hilari C, et al. (1998) The census-based, impact-oriented approach: its effectiveness in promoting child health in Bolivia. Health Policy Plan 13: 140-151.
- Reyes H, Perez-Cuevas R, Salmeron J, Tome P, Guiscafre H, et al. (1997) Infant mortality due to acute respiratory infections: the influence of primary care processes. Health Policy Plan 12: 214-223.
- Bixby LR (2004) Assessing the impact of health sector reform in Costa Rica through a quasi-experimental study. Rev PanamSaludPublica 15: 94-103.
- Rosero-Bixby L (2004) Spatial access to health care in Costa Rica and its equity: a GIS-based study. SocSci Med 58: 1271-1284.
- Shi L, Starfield B, Politzer R, Regan J (2002) Primary care, self-rated health, and reductions in social disparities in health. Health Serv Res 37: 529-550.
- Jaturapatporn D, Dellow A (2007) Does Family Medicine training in Thailand affect patient satisfaction with primary care doctors? BMC FamPract 8: 14.
- Fiscella K, Meldrum S, Franks P, Shields CG, Duberstein P, et al. (2004) Patient trust: is it related to patient-centered behavior of primary care physicians? Med Care 42: 1049-1055.
- Mead N, Bower P (2000) Patient-centredness: a conceptual framework and review of the empirical literature. SocSci Med 51: 1087-1110.
- Weinberger M, Oddone EZ, Henderson WG (1996) Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. N Engl J Med 334: 1441-1447.
- Gill JM, Mainous AG 3rd, Nsereko M (2000) The effect of continuity of care on emergency department use. Arch Fam Med 9: 333-338.
- Hjortdahl P, Borchgrevink CF (1991) Continuity of care: influence of general practitioners' knowledge about their patients on use of resources in consultations. BMJ 303: 1181-1184.
- Roos NP, Carrière KC, Friesen D (1998) Factors influencing the frequency of visits by hypertensive patients to primary care physicians in Winnipeg. CMAJ 159: 777-783.
- Schoen C, Osborn R, Doty MM, Bishop M, Peugh J, et al. (2007) Toward higher-performance health systems: adults' health care experiences in seven countries, 2007. Health Aff (Millwood) 26: w717-734.
- Rothwell PM (2005) Treating individuals 2. Subgroup analysis in randomised controlled trials: importance, indications, and interpretation. Lancet 365: 176-186.
- Kravitz RL, Duan N, Braslow J (2004) Evidence-based medicine, heterogeneity of treatment effects, and the trouble with averages. Milbank Q 82: 661-687.
- Forrest CB, Starfield B (1996) The effect of first-contact care with primary care clinicians on ambulatory health care expenditures. J FamPract 43: 40-48.
- Abyad A, A-Baho AK, Unluoglu I, Tarawneh M, Al Hilfy TK (2007) Development of family medicine in the middle East. Fam Med 39: 736-741.
- Albar AA (1999) Twenty years of family medicine education in Saudi Arabia. East Mediterr Health J 5: 589-596.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 33396
- [From(publication date):
specialissue-2014 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 28824
- PDF downloads : 4572