Research Article Open Access
Family Functioning and Parental Invalidation of Depressed Adolescents with Borderline Personality Disorder Traits
Mbekou Valentin1*, MacNeil Sasha1, Mikedis Theodora1, Malinski Cecilia1, Zanga Jean-Chrysostome1 and Renaud Johanne1,21Standard Life Centre for Breakthroughs in Teen Depression and Suicide Prevention and Douglas Mental Health University Institute, Canada
2McGill Group for Suicide Studies, McGill University, Canada
- *Corresponding Author:
- Mbekou Valentin
Outpatient Clinic of Depressive and Suicidal Disorders
6875 Lasalle Boulevard, Montreal, Quebec, H4H 1R3, Canada
Tel: 514-761-6131
Fax: 514-888-4466
E-mail: Valentin.mbekou@douglas.mcgill.ca
Received Date: June 16, 2015 Accepted Date: August 19, 2015 Published Date: August 26, 2015
Citation: Valentin M, Sasha M, Theodora M, Cecilia M, Chrysostome ZJ, et al. (2015) Family Functioning and Parental Invalidation of Depressed Adolescents with Borderline Personality Disorder Traits. J Child Adolesc Behav 3:235. doi:10.4172/2375-4494.1000235
Copyright: © 2015 Valentin M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
Background: Parental invalidation is thought to contribute to severity of borderline personality disorder (BPD) severity. Certain family functioning environments may foster more invalidation than others. The current study serves to examine how dysfunctional family functioning may allow for BPD symptoms development through the fostering of invalidating environments. Method: 60 female adolescents completed the Borderline Symptoms List (BSL-23), the Family Adaptability and Cohesiveness Evaluation Scale (FACES-V), and the Invalidated Childhood Environment Scale adapted for adolescents (ICES-A) at baseline of a 20-week dialectical-behavioural therapy. Results: Only maternal invalidation was positively correlated with severity of BPD symptoms. Furthermore, maternal invalidation mediated the relationship between disengaged family functioning and adolescent BPD symptoms. Limitations: The ICES-A is currently undergoing validation, therefore results should be interpreted cautiously. Also, the clinical sample used in the study presented with a restricted upper-bound range of symptoms, thus limiting generalizability. Conclusions: These findings highlight the need to work upon the family environment for the treatment of BPD symptoms, especially in adolescence before symptoms become consolidated.
Keywords
Adolescent; Borderline personality disorder; Family environment
Introduction
Borderline personality disorder (BPD) is an important mental health problem defined by a pervasive pattern of instability of interpersonal relationships, self-image, and affects. It is further characterized by impulsivity, recurrent suicidal behaviours or selfmutilation, chronic feelings of emptiness, and intense emotional reactivity and anger [1,2] widely accepted biosocial etiological model of BPD posits that borderline traits develop as a function of inherent deficits in emotion regulation systems combined with dysfunctional environments. Therefore, research looking to identify types of dysfunctional environments which may affect the development of BPD is necessary in order to better provide treatments targeted towards these problematic environmental circumstances. The current study serves to examine how dysfunctional family systems may allow for BPD symptoms development through the fostering of invalidating environments.
Linehan’s et al. [2] biosocial model maintains that emotional dysregulation vulnerabilities interact with invalidating childhood environments to contribute to the further development and maintenance of emotional dysregulation, which is at the core of BPD symptoms. Therefore, the emotional dysregulation of individuals with BPD is thought to be sustained within the context of an invalidating childhood environment. An invalidating caregiver will inappropriately respond to the child’s communication of private experiences through punishment, trivialization, or otherwise extreme responses [2]. In contrast, validating caregivers acknowledge the child’s emotions, help them to experience, and accept emotions appropriately. The consequences of invalidating caregivers are such that the child does not learn to label private emotional experiences as valid, normative and trustworthy. The individual does not learn to tolerate distress, or form realistic goals or expectations; instead the individual develops a pattern of oscillating between emotional inhibition and extreme emotional states observed in BPD [2,3]. Research has provided evidence for the role of invalidating childhood environments in the development and maintenance of emotion dysregulation and BPD symptomology. Firstly, an investigation of risk factors for BPD showed an important association between BPD and deranged family environments. Patients with BPD experienced more separation from their parents (growing up in foster homes), experienced more criminality and violence in the family (parental violencetowards children, or spousal violence), and parents displayed inappropriate rearing styles with less care and affection towards their children [4]. In an adult community sample, findings revealed that perceptions and/or experiences of parental invalidation during childhood accounted for the largest association with emotion dysregulation [5]. Counter evidence also exists, however, indicating that parental invalidation is not always related to BPD symptomatology [6,7]. Therefore, there is a need for further research to examine the association between invalidating environments and the development of BPD traits.
The associations between invalidating childhood environments, emotion dysregulation, and borderline symptomatology have mostly been assessed retrospectively with adult samples. Investigation of these associations with adolescents could provide concurrent evidence of the role of invalidating environments in the etiology of BPD traits. However, validity of the BPD diagnosis in adolescence has been very controversial, thus limiting research in this area. Some argue an overlap between the symptoms of BPD and the range of normative developmental behaviors for adolescence, such as risk-taking and impulsive behaviors. Adolescents are particularly susceptible to emotion regulation difficulties, due to the transitional aspect of this developmental period. Adolescence is marked by changes in social situations and the experience of less positive and more negative and intense emotions [8]. Yet the psychic pain, desperation, and high risk for suicide are not typical during this period [9], and research is increasingly demonstrating that BPD can be reliably identified in adolescence, which can permit early and appropriate intervention before symptoms become consolidated [10,11]. Furthermore, research is providing evidence for the contributions of adolescent BPD symptoms to impaired functioning in adulthood, as evidenced by lower life satisfaction, social support and relationship quality, and more chronic stress [12]. As such, examination of BPD symptom development in an adolescent sample can be a reliable opportunity for examining the effects of parental invalidation as it occurs. Considering the difficulties of adolescence, this time may pose increased vulnerability to the effects of parental invalidation. Initial studies have shown that internalizing and externalizing symptoms in adolescents have been positively associated with adolescent-reported parental invalidation of emotions [13]. These authors also suggest that the association between parental invalidation and internalizing and externalizing symptoms in adolescence is due to difficulties with emotion dysregulation. Furthermore, adolescents participating in family-based psychological interventions were found to experience more invalidating behaviours from their parents, which was associated with more externalizing behavioural problems and less effective emotion regulation [14]. Low levels of parental affection and presence of harsh punishment, neglect, or ignoring the child have also been associated with BPD symptoms in adolescence [15,16]. Thus, initial evidence points towards an influence of parental invalidation on adolescent symptoms of BPD.
To date, research has explored effects of invalidation on BPD. However the influence of other characteristics of family systems may be important to understand the context in which parental invalidation occurs. The Circumplex Model [17] posits that family cohesion, flexibility, and communication are important dimensions to consider in assessing the effective functioning of a family system. Family cohesion refers to the emotional bonds between family members, and the extent to which members can balance closeness to each other with individual separateness. Family flexibility is the capacity of the family to change its leadership roles and rules in order to adapt to events that may require a shift in the established system. This model proposes a curvilinear relationship between these dimensions, such that balanced, or moderate, levels of cohesiveness and flexibility are considered most adaptive. At these levels, members will balance change and stability, as well as separateness and closeness, while engaging in adaptive communication to maintain the balance of these two dimensions. In particular, adaptive communication serves to help families transition fluidly between balanced and unbalanced states of cohesion and flexibility, as necessitated by given situations. In contrast, constant unbalanced, or extreme levels of cohesion and flexibility are considered to be maladaptive to family functioning. For example, families can either be enmeshed (too close) or disengaged (too separate), chaotic in their rules (too flexible) or rigid in their rules (not flexible enough). These families will likely engage in poor communication between members, and thus keep the family functioning unbalanced. Therefore, according to this model, balanced families will be able to more effectively cope with crises than will unbalanced families, due to better familial resources and skills in flexibility, cohesion, and communication [18]. Family systems can be challenged when one of the members enters adolescence, as they search for their identity and struggle against role confusion [19]. The adolescent’s growing need to create his/her identity and assert themselves in their new role can force the family system to reorganize itself [20]. In fact, research has found that adolescents who presented more advanced identity development belonged to more balanced families, while those who reported less identity formation tended to come from unbalanced families [21]. According to the Circumplex Model, balanced families encourage individuality, and thus will be better able to cope with the added developmental pressures of adolescence, thereby facilitating better adolescent identity formation [21]. On the other hand, research suggests that less flexible and cohesive families may not be able to adequately meet the adolescent’s demands and needs for change within the family system, which may contribute to problematic behaviour [22]. For example, it has been found that adolescent perceptions of cohesion and flexibility in the family are significant predictors of suicide attempts [23]. Childhood depression has also been associated with disengaged family systems, marked by inadequate closeness and support [24]. Unbalanced family functioning has also been associated with the severity of manic symptoms in adolescent bipolar disorder [25]. Furthermore, unbalanced levels of family cohesion and flexibility lead to more verbal and physical aggression during conflicts with parents [26]. Taken together, these findings suggest that unbalanced family types likely provide a negative environment that fosters the development of psychosocial problems in adolescents due to extreme levels of cohesion, flexibility, and negative communication styles.
The influence of family systems on children and adolescents may be of importance within the context of borderline personalitydisorder (BPD). Early research into the family functioning of BPD patients points to the prominence of unbalanced family systems for these individuals. In an initial qualitative study of three BPD patients, all individuals experienced both rigid and diffuse boundaries, and inconsistent expressions of emotion. They also reported rapid fluctuations in their emotions towards other family members, role reversals within the family system, and ineffective communication styles lacking expression of love, warmth, or understanding [27]. Although, there is a paucity of further research, one study indicates that low family cohesion, maternal support, and high mother-child discord during adolescence predict borderline symptoms in adulthood [28], However, contrasting results showed that the association between family functioning and BPD was accounted for by the experience of childhood emotional abuse, rather than family functioning per se [29]. Therefore, the role of family functioning in BPD still requires further research in order to assess its contribution to onset of the disorder and to elaborate adequate interventions targeting problematic family systems. To our knowledge, no research has examined the role of familial cohesion and adaptability in relation to the expression of borderline symptoms in adolescents, who may be at particular risk for experiencing negative consequences. Therefore, the aim of the current study is to provide initial evidence for the contribution of familial cohesion and adaptability to borderline symptomatology. Specifically, this study aims to investigate if unbalanced family systems extreme in flexibility and cohesion engender a maladaptive familial dynamic in which parental invalidation can occur, thereby facilitating the development of borderline symptoms in adolescence. It is thus hypothesized that unbalanced family systems will predict more parental invalidation as a negative communication style. Furthermore, it is hypothesized that parental invalidation will be a mediator for the relationship between unbalanced family systems and severity of BPD symptoms.
Method
Participants
Sixty-three female adolescents aged between 13 and 18 years of age (M=15.75, SD=1.16) were included in the study. Participants were referred from first or second line health clinics to the Depressive and Suicidal Disorders Outpatient Clinic (youth section) at the Douglas Mental Health University Institute because of depressive symptoms. Participants with Axis II Cluster B traits were recruited over a 7-year period at the clinic to take part in a specialized dialectical-behaviour therapy (DBT) program. Inclusion criteria for the DBT program consisted of an axis I diagnosis within the last year, clinical presentation of cluster B personality traits, suicidal and/or parasuicidal behaviors, and availability and motivation of both the adolescent and their parent(s) to participate in weekly group and individual sessions. Exclusion criteria for the DBT program included psychosis and intellectual deficiencies characterized by an IQ below 80. The psychiatric profile of the participants is presented in Table 1. The mean number of Axis I diagnoses was 1.81 (SD=0.96; Range 0-4), suggestive of a high psychiatric severity among this sample [30]. A majority of participants (n=49, 82%) provided data regarding both parents, whereas 13% (n=8) provided data only regarding the mother and 0.05% (n=3) provided data only regarding the father.
| % (N) | Range | M | SD | Level | |
|---|---|---|---|---|---|
| Axis I Diagnoses Depressive Disorders |
69.8 (44) | ||||
| Eating Disorders | 33.3 (21) | ||||
| Anxiety Disorders | 28.5 (18) | ||||
| Disruptive Behavior Disorders | 27.0 (17) | ||||
| Substance Use Disorders Sleep Disorder |
11.1 (7) 1.6 (1) |
||||
| Learning Disorder | 1.6 (1) | ||||
| Axis 2 Diagnoses | |||||
| Cluster B Traits (Borderline) | 100.0 (63) | ||||
| Cluster C Traits | 6.4 (4) | ||||
| BSL-23 | 1.00 âÂ?Â? 83.00 | 48.22 | 22.99 | ||
| ICES-A Maternal invalidation |
1.00 âÂ?Â? 4.50 | 2.15 | 0.79 | ||
| Paternal invalidation | 1.07 âÂ?Â? 4.43 | 2.33 | 0.64 | ||
| FACES-IV * Balanced Cohesion |
10 âÂ?Â? 90 | 35.84 | 25.15 | High Balanced Cohesion |
|
| Balanced Flexibility | 10 âÂ?Â? 98 | 40.65 | 23.79 | High Balanced Flexibility | |
| Disengaged | 15 âÂ?Â? 98 | 41.91 | 18.55 | Moderate Disengagement | |
| Enmeshed | 10 - 95 | 26.75 | 13.86 | Very Low Enmeshment | |
| Rigid | 15 - 85 | 38.71 | 15.96 | Low Rigidity | |
| Chaotic | 12 - 95 | 39.68 | 21.11 | Low Chaos |
Note. BSL-23=Borderline Symptom List; ICES-A=Invalidating Childhood Environment Scale-Adolescents; FACES-IV=Family Adaptability and Cohesion Evaluation Scale-IV.
*FACES-IV is reported in percentile scores.
Table 1: Psychiatric Profile.
Measures
Invalidating environment: The Invalidating Child Environment Scale [31] is a retrospective measure of parental invalidation experienced during childhood. In this study, the ICES was adapted from a retrospective evaluation during adulthood to a format assessing current parental invalidation for use with adolescents [32]. Each parent is rated separately for paternal or maternal invalidation with score ranging from 0 to 5, where higher scores indicate more parental invalidation. Psychometric evaluations of the original ICES scale are good, showing adequate internal consistency in clinical eating disorder samples with alpha coefficients ranging from .77 to .90 for both maternal and paternal subscales [33]. Among non-clinical samples of eating disorders, on the other hand, internal consistency was found to be less reliable, with alpha coefficients ranging from 0.53 to 0.67 [31,34]. However, good internal consistency was reported among a nonclinical sample evaluated for BPD (0.88-0.90) thereby providing the first psychometrically sound evidence for this measure among clinical and nonclinical samples Robertson et al. [35] also found good concurrent validity for the ICES with BPD samples, whereby all six subscales of the ICES positively correlated with borderline symptoms. The ICES-A used for this study is currently in the process of validation, but initial psychometric data for this sample suggest adequate internal consistency, with Cronbach’s alpha at .80 for the paternal invalidation scale and at 0.91 for the maternal invalidation scale.
Family Functioning: The Family Adaptability and Cohesion Evaluation Scale – IV [36] is a 42-item family self-report assessment evaluating family functioning according to the Circumplex Model. This scale contains six subscales, two for balanced levels of functioning (Balanced Cohesion and Balanced Flexibility), and four representing the unbalanced levels of functioning: enmeshed (high cohesion), disengaged (low cohesion), chaotic (high flexibility) and rigid (low flexibility). Percentile scores corresponding to levels of balance (very low, low, somewhat high, high) are calculated for each subscale. Higher scores on the balanced subscales reflect positive family functioning, while higher scores on the unbalanced subscales reflect poor family functioning. Psychometric validation of this scale has reported adequate internal consistency for all subscales, with Cronbach’s alphas ranging from 0.77 (enmeshed) to 0.89 (balanced cohesion) [36].
BPD Symptoms: The short form of the Borderline Symptom List (BSL-23; Bohus et al., 2009) contains 23 items assessing the extent to which respondents have suffered from particular BPD symptoms in the past week from 0 (not at all) to 4 (very much). Scores range from 0 to 92, with higher scores indicating higher endorsement of presence and severity of symptoms. Psychometric evaluations of this scale suggest a unidimensional factor structure with high internal consistency, whereby Cronbach’s alphas range from 0.94 to 0.97 across various samples. Furthermore, this scale discriminates adequately between those with BPD and those with Axis I diagnoses [37]. Furthermore, the BSL-23 was found to be strongly associated with the presence of BPD assessed via semi-structured interview, thereby indicating the usefulness and validity of the BSL-23 as a clinical tool [38].
Procedure
All participants took part in an adapted 20-week dialectical behaviour-therapy (DBT) multi-skills family training [32].Participants completed all measures (BSL-23, FACES-IV, and ICES-A) at baseline during the first individual meeting with their therapist.
Results
The diagnostic profile of participants and descriptive statistics for all the measures are provided in Table 1. Participants experienced more levels of typical caregiving family environments than any other type. Furthermore, family functioning was adaptive and flexible, with scores on the unbalanced family functioning subscales ranging from very low to low unbalanced functioning.
Correlational analyses were conducted to evaluate the association between parental invalidation and unbalanced family functioning with borderline symptomatology. Of all four unbalanced family functioning subscales and both parental invalidation subscales, only maternal invalidation (r=0.330, p=0.016) and disengaged family functioning (r=0.25, p=0.05) were significantly associated with borderline symptoms.
Further, correlational analyses showed that maternal invalidation significantly correlated with disengaged family functioning (r=0.477, p<0.000). Paternal invalidation was not significantly correlated with any form of unbalanced family functioning.
To test whether unbalanced family functioning predicted parental invalidation, linear regression analyses were conducted. The four unbalanced family functioning subscales from the FACES-IV were entered as predictor variables to determine their influence on maternal and paternal invalidation separately.
Results showed that this model significantly predicted maternal invalidation (F (4, 61)=7.66, p<0.000), accounting for about 30% of the variance. Of the four predictors, only disengaged family functioning was found to be a significant contributor to the variance accounted for by the model (β=0.56, t (4)=4 825, p<0.001). The same model predicting paternal invalidation was non-significant. As such, unbalanced family functioning, more specifically disengaged family functioning, significantly predicted maternal invalidation, but not paternal invalidation.
Based upon these results, a mediational analysis using the PROCESS macro for SPSS [39] was conducted to determine whether maternal invalidation mediated the association between disengaged family functioning and BPD symptoms. The FACES-IV disengaged family functioning subscale was entered as the predictor variable, the ICES-A maternal invalidation subscale as the mediator, and the BSL-23 total score as the outcome variable.
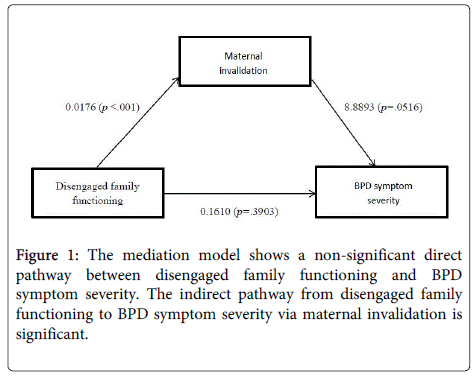
The mediation model is depicted in Figure 1. The direct effect of disengaged family functioning on BPD symptom severity, c`=0.1610, was not statistically significant from zero, t (57)=0.865, p=0.39 with a 95% confidence interval of -0.2115 to 0.5336.
The indirect effect of disengaged family functioning via maternal invalidation on borderline symptoms was significant. The coefficient for this effect (ab=0.1568) was statistically different than zero, as indicated by a 95% BC Bootstrap confidence interval of 0.0152 to 0.3755 that is entirely above zero [39]. Thus, the association between disengaged family functioning and borderline symptom severity among depressed adolescents was mediated by adolescent-reported maternal invalidation.
Discussion
To our knowledge, this study is the first to directly examine the role of family system functioning in the adolescent development of BPD symptoms, specifically, and the mediating role of parental invalidation. This is important within the context of adolescent BPD considering the proximity of adolescents to their parents, and difficult transitional aspect of this developmental period [19,20]. It was hypothesized that unbalanced family functioning would predict BPD symptoms through the presence of parental invalidation. Results showed that only disengaged family functioning was related to maternal invalidation. Disengaged family functioning did not directly predict BPD symptoms, yet the indirect pathway via maternal invalidation did. As such, disengaged family functioning predicts BPD symptom severity in adolescence through maternal invalidation.
According to theory, disengaged families find themselves very low on the cohesion dimension of functioning typically exhibiting rejecting parenting styles, whereby parents do not pay attention to their children, are uninvolved, and do not interact much with the child unless the child interferes with their own activities. In this sample of adolescents with BPD traits, disengaged family functioning was reportedly higher than other types of families. According to our results, these types of families seem to foster adolescent perceptions of invalidating maternal responses, whereby the mother may be unresponsive to the adolescent’s expressions of emotions [2]. The association of disengaged family functioning with poor family quality and more family problems has previously been reported [40]. This suggest the importance of family cohesion for the adequate functioning of the family system, the appropriate expression of emotions by its members, and the expression of validating responses. In turn, maternal invalidation mediated the relationship between disengaged family functioning and adolescent BPD symptoms in this study. Research has supported the role of maternal communication as a risk factor for development of BPD in adolescence among community samples. Adolescent girls who experienced less positive interactions and satisfaction with their mothers reportedly experienced stable levels of BPD symptom severity when compared to the decreasing severity of BPD symptoms experienced by those with positive maternal interactions [41]. Furthermore, adolescent girls with mothers who reported using invalidating behaviours utilized more maladaptive emotion regulation strategies, thus putting them at risk for BPD symptom development [42]. This study thus extends evidence for the contribution of maternal invalidation to BPD symptom severity to a clinical adolescent sample by providing initial evidence of the context which may foster such communication style. Adolescent girls who experience few interactions with their mothers, as with disengaged families, may be at risk of perceiving such family systems as invalidating. Accordingly, such perceptions of parental invalidation can lead to the development of BPD symptoms. This study therefore suggests that parental invalidation is the process by which BPD symptoms develop in the context of disengaged family functioning.
The role of maternal invalidation as a mediator for the association between disengaged family functioning and BPD symptoms in this study provides support for the social and environmental aspects of Linehan’s biosocial model [2], whereby inherent emotional vulnerability and environmental invalidation lead to emotional dysregulation and BPD symptoms. Many studies have shown the importance of individual differences in emotional vulnerability as a contributor to BPD symptoms [43,44]. Few studies have, however, examined the environmental component of this model, with existing literature providing mixed results [4-7,44]. This study thus contributes to the body of literature supporting the role of the environment and of parental invalidation as risk factors for the development of BPD symptoms in adolescence. Many studies have assessed this association using retrospective measures of parental invalidation with adults, yet it is important to consider how parental invalidation may affect the development of BPD as it occurs to allow for therapists to target such patterns directly with adolescents and parents in order to influence symptom development and progression [45]. As such, treatment options for BPD such as dialectical-behavioural therapy (DBT) for adolescents can emphasize parental validation strategies skills-training to affect better outcomes. We could anticipate that teaching validation strategies, in addition to the core DBT skills, could lead to better adolescent-parent relationships marked by less parental invalidation, thus modifying the developmental trajectory of BPD symptoms.
The findings of this study must be considered within some limitations. Firstly, the adaptation for adolescents of the original ICES used in this study is currently undergoing validation, therefore results should be interpreted cautiously. Second, this study was conducted with a sample of adolescent girls referred to the specialized adolescent depression clinic for their cluster B traits to attend the DBT program. As such, our sample presents with a restricted upper-bound range of BPD symptom severity. Furthermore, the findings from this study cannot address trends of family functioning and invalidation among male samples. Also, these results must also be considered within the framework of the comorbid clinical depression diagnosed in almost 70% of the sample. The homogeneity of the sample in this study does limit the generalizability of these findings beyond the clinical context, where up to 83% of patients with BPD who can evidence this comorbid diagnostic profile [46]. Future research should examine the association of family functioning, parental invalidation, and BPD symptom severity in a broader sample outside of a specialized clinical setting. Furthermore, considering the small sample size to conduct mediation analyses, these findings are tentative and should be interpreted cautiously. However, bootstrap estimates allow for certain confidence in the results. Finally, data for this study is cross-sectional, with all questionnaires evaluated at baseline of treatment. Futures studies could benefit from using a longitudinal design to evaluate treatment outcomes based on family functioning and parental invalidation.
Despite these limitations, this study highlights the importance of identifying early developmental risk factors that could influence the outcomes of BPD, notably the role of disengaged family functioning and maternal invalidation. It seems that disengaged family functioning leads to the development of more severe BPD symptoms through a process of maternal invalidation [47-51]. Thus, this study emphasizes the need to work upon the family environment for the treatment of BPD symptoms, especially in adolescence before symptoms become consolidated.
References
- Powers AD,Gleason ME, Oltmanns TF (2013) Symptoms of borderline personality disorder predict interpersonal (but not independent) stressful life events in a community sample of older adults. J AbnormPsychol 122: 469-474.
- Linehan M (1993) Cognitive-Behavioral Treatment for Borderline Personality Disorder: The Dialects of Effective Treatment. New York, NY: Guilford Press.
- Fruzzetti AE, Shenk CE (2008) Fostering validating responses in families. Social Work in Mental Health 6: 215-227.
- Bandelow B, Krause J, Wedekind K, Broocks A, Hajak G, et al. (2005) Early traumatic life events, parental attitudes, family history, and birth risk factors in patients with borderline personality disorder and healthy controls. Psychiatry Res 134: 169-179.
- SturrockB,Mellor D (2014) Perceived emotional invalidation and borderline personality disorder features: a test of theory. Personal Ment Health 8: 128-142.
- Cheavens JS, Rosenthal MZ, Daughters SB, Nowak J, Kossonc D, et al. (2005) An analogue investigation of the relationships among perceived parental criticism, negative affect, and borderline personality disorder features: the role of thought suppression. Behaviour Research and Therapy 43:257–268.
- Hooley JM,Hoffman PD (1999) Expressed emotion and clinical outcome in borderline personality disorder. Am J Psychiatry 156: 1557-1562.
- Larson R,Lampman-Petraitis C (1989) Daily emotional states as reported by children and adolescents. Child Dev 60: 1250-1260.
- Westen D, Shedler J, Durrett C, Glass S, Martens A (2003) Personality diagnoses in adolescence: DSM-IV Axis II diagnoses and an empirically derived alternative. Am J Psychiatry 160: 952-966.
- Larrivée MP (2013) Borderline personality disorder in adolescents: the He-who-must-not-be-named of psychiatry. Dialogues ClinNeurosci 15: 171-179.
- Miller AL,Muehlenkamp JJ, Jacobson CM (2008) Fact or fiction: diagnosing borderline personality disorder in adolescents. ClinPsychol Rev 28: 969-981.
- Winograd G,Cohen P, Chen H (2008) Adolescent borderline symptoms in the community: prognosis for functioning over 20 years. J Child Psychol Psychiatry 49: 933-941.
- Buckholdt KE, Parra GR, Jobe-Shields L (2013) Intergenerational transmission of emotion dysregulation through parental invalidation of emotions: Implications for adolescent internalizing and externalizing behaviors. J Child Fam Stud 23: 324-332.
- Shenk CE, Fruzzetti AE (2013) Parental validating and invalidating responses and adolescent psychological functioning: An observational study. The Family Journal 22: 43-48.
- Johnson HD (2002) Associations among family adaptability and cohesion, interparental conflict, and tactics used during young adults, conflict with parents. Psychol Rep 9: 315-325.
- Johnson JG, Cohen P, Chen H, Kasen S, Brook JS (2006) Parenting behaviors associated with risk for offspring personality disorder during adulthood. Arch Gen Psychiatry 63: 579-587.
- Olson DH, Russell CS, Sprenkle DH (1983) Circumplex model of marital and family systems: VI. Theoretical update. Fam Process 22: 69-83.
- Olson DH (2000) Circumplex model of marital and family systems. Journal of Family Therapy 22: 144-167.
- Erikson EH (1968) Identity: Youth and Crisis. New York: Norton.
- Minuchin P (1985) Families and individual development: provocations from the field of family therapy. Child Dev 56: 289-302.
- Bhushan R,Shirali KA (1992) Family types and communication with parents: A comparison of youth at different identity levels. J Youth Adolesc 21: 687-697.
- Joh JY,Kim S, Park JL, Kim YP (2013) Relationship between Family Adaptability, Cohesion and Adolescent Problem Behaviors: Curvilinearity of Circumplex Model. Korean J Fam Med 34: 169-177.
- Sheftall AH,Mathias CW, Furr RM, Dougherty DM (2013) Adolescent attachment security, family functioning, and suicide attempts. Attach Hum Dev 15: 368-383.
- Kashani JH,Allan WD, Dahlmeier JM, Rezvani M, Reid JC (1995) An examination of family functioning utilizing the circumplex model in psychiatrically hospitalized children with depression. J Affect Disord 35: 65-73.
- Sullivan AE,Judd CM, Axelson DA, Miklowitz DJ (2012) Family functioning and the course of adolescent bipolar disorder. BehavTher 43: 837-847.
- Johnson JG, Cohen P, Gould MS, Kasen S, Brown J, et al. (2002) Childhood adversities, interpersonal difficulties, and risk for suicide attempts during late adolescence and early adulthood. Arch Gen Psychiatry 59: 741-749.
- Kirsten DK, Lellyveld VV, Venter CA (2006) Perceptions that patients diagnosed with Borderline Personality Disorder have of their families. South African Journal of Psychology 36: 319-339.
- Stepp SD, Olino TM, Klein DN, Seeley JR, Lewinsohn PM (2013) Unique influences of adolescent antecedents on adult borderline personality disorder features. Personality Disorders: Theory, Research, and Treatment 4: 223-229.
- Carr S, Francis A (2009) Childhood familial environment, maltreatment, and borderline personality disorder symptoms in a non-clinical sample: A cognitive behavioural perspective. Clinical Psychologist 13: 28-37.
- Angst J,Sellaro R, RiesMerikangas K (2002) Multimorbidity of psychiatric disorders as an indicator of clinical severity. Eur Arch Psychiatry ClinNeurosci 252: 147-154.
- Mountford V,Corstorphine E, Tomlinson S, Waller G (2007) Development of a measure to assess invalidating childhood environments in the eating disorders. Eat Behav 8: 48-58.
- Mbekou V, Mikedis T, Janelle A, Zanga JC, Renaud J (2011) Invalidating Childhood Environment Scale – Adolescent Version (ICES-A). Unpublished Document.
- HaslamM,Mountford V, Meyer C, Waller G (2008) Invalidating childhood environments in anorexia and bulimia nervosa. Eat Behav 9: 313-318.
- Sturrock BA, Francis A, Carr S (2009) Avoidance of affect mediates the effect of invalidating childhood environments on borderline personality symptomatology in a non-clinical sample. Clinical Psychologist 13: 41-51.
- Robertson CD, Kimbrel NA, Nelson-Gray RO (2013) The invalidating childhood environment scale (ICES): Psychometric properties and relationship to borderline personality symptomatology. J PersDisord 27: 402-410.
- Olson D1 (2011) FACES IV and the Circumplex Model: validation study. J Marital FamTher 37: 64-80.
- Bohus M, Kleindienst N, Limberger MF, Stieglitz RD, et al. (2009) The short version of the Borderline Symptom List (BSL-23): Development and initial data on psychometric properties. Psychopathology 42: 32-39.
- Glenn CR,Weinberg A, Klonsky ED (2009) Relationship of the Borderline Symptom List to DSM-IV borderline personality disorder criteria assessed by semi-structured interview. Psychopathology 42: 394-398.
- Hayes AF (2012) PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling.
- Craddock AE (2001) Family system and family functioning: Circumplex model and FACES IV. Journal of Family Studies 7: 29-39.
- Whalen DJ, Scott LN, Jakubowski KP, McMakinm DL, Hipwell AE, et al. (2014) Affective behavior during mother-daughter conflict and borderline personality disorder severity across adolescence. Personality Disorder 5: 88-96.
- Yap M BH, Allen NB, O’Shea M, di Parsia P, Simmons JG, et al. (2011) Early adolescents’ temperament, emotion regulation during mother-child interactions, and depressive symptomatology. DevPsychopathol 23: 267-282.
- Kuo JR, Linehan MM (2009) Disentangling emotion processes in BPD: physiological and self-reported assessment of biological vulnerability, baseline intensity, and reactivity to emotionally evocative stimuli. J AbnormPsychol 118: 531-544.
- Reeves M,James LM, Pizzarello SM, Taylor JE (2010) Support for Linehan's biosocial theory from a nonclinical sample. J PersDisord 24: 312-326.
- Rathus JH, Miller AL (2015) DBT Skills Manual for Adolescents. New York, NY: The Guilford Press.
- Biskin RS Paris J (2013) Comorbidities in borderline personality disorder. Psychiatric Times.
- Bellino S,Patria L, Paradiso E, Di Lorenzo R, Zanon C, et al. (2005) Major depression in patients with borderline personality disorder: a clinical investigation. Can J Psychiatry 50: 234-238.
- ComtoisKA,Cowley DS, Dunner DL, Roy-Byrne PP (1999) Relationship between borderline personality disorder and Axis I diagnosis in severity of depression and anxiety. J Clin Psychiatry 60: 752-758.
- Dolle K, Schulte-Korne G, O’Leary AM, von Hofacker N, Izat Y, et al. (2012) The Beck Depression Inventory-II in adolescent mental health patients: Cut-off scores for detecting depression and rating severity. Psychiatry Res 200: 843-848.
- Henry CS, Robinson LC, Neal RA, Huey EL (2006) Adolescent perceptions of overall family system functioning and parental behaviors. Journal of Child and Family Studies 15: 308-318.
- Miller AL, Rathus JH, Linehan MM (2007) Dialectical Behavior Therapy with Suicidal Adolescents. NY: The Guilford Press.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 19453
- [From(publication date):
October-2015 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 14561
- PDF downloads : 4892