Research Article Open Access
Failed Agility LP Total Ankle Replacement with Severe >40 Varus Deformity Revision with Prosthesis Conversion and Soft-Tissue Procedures Alone
Thomas S. Roukis*Orthopaedic Center, Gundersen Health System, South Avenue, La Crosse, Wisconsin
- *Corresponding Author:
- Thomas S. Roukis
Orthopaedic Center, Gundersen Health System
Mail Stop: C02-006, 1900 South Avenue
La Crosse, Wisconsin 54601-5467
Tel: 608-775-9673
Fax: 608-775-6707
E-mail: tsroukis@gundersenhealth.org
Received Date: April 02, 2016; Accepted Date: June 22, 2016 ; Published Date: June 30, 2016
Citation: Roukis TS (2016) Failed Agility™ LP Total Ankle Replacement with Severe >40° Varus Deformity Revision with Prosthesis Conversion and Soft-Tissue Procedures Alone. Clin Res Foot Ankle 4:190. doi:10.4172/2329-910X.1000190
Copyright: © 2016 Thomas S. Roukis. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Clinical Research on Foot & Ankle
Abstract
Achieving frontal plane alignment of the ankle joint during primary and revision total ankle replacement is essential for long-term success. This manuscript presents the revision of a failed Agility™ LP total ankle replacement system with severe > 40° varus ankle deformity that was corrected with explanation and conversion to an INBONE™ II total ankle system coupled with soft-tissue release/reconstruction employing percutaneous Achilles tendon lengthening, posterior tibial tendon intramuscular recession lengthening and modified Evans peroneus longus lateral ankle stabilization. Additionally, prophylactic tarsal tunnel release was performed to reduce potential for postoperative nerve compression. At short-term 2.5-years follow-up the patient had a well-balanced and painless foot/ ankle and return of a functional lower limb.
Keywords
Ankle Mal-alignment; Complications; Deformity; Musculotendinous imbalance; Total ankle arthroplasty
Introduction
Achieving a plantigrade foot and ankle is essential for the success of total ankle replacement (TAR)[1-8]. The general tenet of soft-tissue balancing involves the release of the contracted soft-tissue on the concave side and reinforcement on the convex side of the ankle[1-6].Uncorrectable mal-alignment of the ankle joint is an accepted contraindication to both primary and revision TAR but the boundaries of what constitutes such a deformity are unknown [9].
Henricsonet al. [1] published a study of 196 second generation TAR’s and reported that of the ankles with pre-operative varus or valgus deformities nearly 50% (29/55 varus and 23/46 valgus) retained some mal-alignment after the procedure.Those retaining 15° of varus or valgus deformity after the index TAR surgery had markedly greater failure rate [1]. That study, as well as others [2-6], found the predominate frontal plane deformity to be ankle varus and stated that any deformity should be corrected at the time of the index TAR surgery with corrective joint resection osteotomies and/or soft-tissue release/reconstruction.
Hobson et al.[2] examined 91 TAR’s with ≤ 10° frontal plane deformity and 32 TAR’s with frontal plane deformity between 11° and 30°. A series of osseous and soft-tissue procedures were performed in order to achieve hindfoot alignment to within 5° of neutral at the time of TAR implantation. At a mean follow-up of 4-years there were no differences in post-operative range of motion or complications with 84% of the TAR’s with ≤ 10° deformity, as well as, those with deformity between 11° and 30° as long as the achieved final hindfoot alignment to within 5° of neutral. Similarly, Queen et al.[5] examined 17 TAR’s with > 15° frontal plane deformity, 27 with 5° to 15° varus, and 38 with neutral alignment defined as < 5° frontal plane deformity. A series of osseous and soft-tissue procedures were performed in order to achieve hindfoot alignment to within 5° of neutral during the index TAR surgery. At a mean follow-up of 2-years there were no differences regarding clinical outcomes and physical performance measures based on pre-operative frontal plane deformity when post-operative alignment was restored to within 5° of neutral during the index TAR surgery. Finally, Sung et al.[6] examined 20 TAR’s with frontal plane deformities ≥ 20° and 79 ankles with deformities < 20°, the investigators showed no difference between the outcomes measured between these groups at 2-years post-operative. Each of these studies credited not only osseous correction but also careful attention to soft-tissue balancing until the entire foot and ankle were in proper alignment during the index TAR as the keys to success with frontal plane deformities ≤ 30° [2,5,6].
The potential to reduce severe ≥ 30° varus deformity to neutral alignment during primary and/or revision TAR without osteotomy remains poorly understood. Hobson et al.[2] presented a subset of 6 Scandinavian Total Ankle Replacement prostheses (STAR™, Waldemar Link, Hamburg, Germany/Stryker, Mahwah, NJ) with pre-operative varus deformity between 26° and 30° corrected to within 5° of neutral through fractional lengthening or transection of the deltoid ligament, posterior tibial tendon lengthening, lateral ankle ligament reconstruction, calcaneal osteotomy or subtalar arthrodesis. No data analysis for this patient population was performed but the overall conclusions of the authors were that patients with an ankle varus deformity ≤ 30° can safely undergo TAR, expecting to achieve equivalent results to those of patients with neutral alignment. Hamel[10] presented a subset of 5 STAR™ prostheses with pre-operative varus deformity between 25° and 30° and another two with 32° and 41° deformities. All varus deformities were corrected to within 5° of neutral through whole anterior tibial tendon transfer to the intermediate/lateral cuneiform coupled with fractional lengthening or transection of the deltoid ligament, posterior tibial tendon lengthening or tenotomy, peroneus longus to peroneus brevis transfer, lateral ankle ligament reconstruction, as well as, medial malleolar, calcaneal and/or first metatarsal osteotomy. The patient with a 41° varus deformity was corrected to 1° varus but developed tibial nerve compression post-operatively that required tarsal tunnel decompression with full recovery noted. Finally, Hanselman et al.[11] presented a case of a 54-year old man involving correction of a 29° varus deformity to 2° varus at 8-months follow-up without peri-articular osteotomy. They employed an INBONE™ II total ankle system with PROPHECY™ computed-tomography-derived patient-specific cutting guides (Wright Medical Technology, Inc., Arlington, TN) and lateral ankle stabilization alone.
The author presents a case involving a failed Agility™ LP total ankle replacement system (DePuySynthes Joint Reconstruction, Warsaw, IN) with severe > 40° varus ankle deformity that was corrected with explantation and conversion to INBONE™ II total ankle replacement system and soft-tissue release/reconstruction employing percutaneous Achilles tendon lengthening, posterior tibial tendon intramuscular recession lengthening and modified Evans peroneus longus lateral ankle stabilization. Additionally, prophylactic tarsal tunnel release was performed to reduce potential for post-operative nerve compression.
Case Study
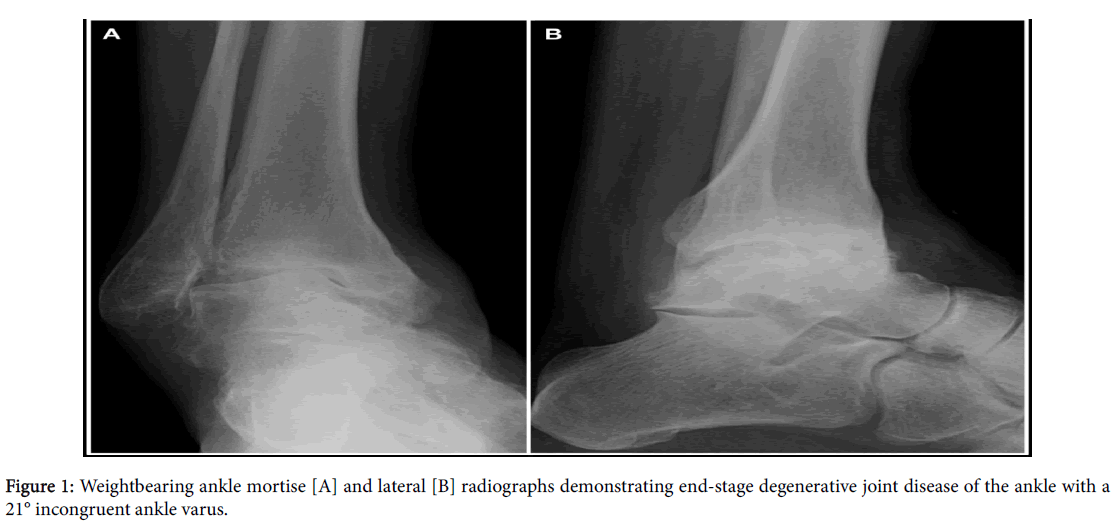
A 54-year old man was evaluated in January 2007 by a foot and ankle orthopaedic surgeon at the author’s institution for chronic right ankle pain. The ankle pain stemmed from a severe inversion ankle injury in 1975 followed by a series of inversion ankle sprains over the ensuing years that culminated with a severe injury occurring when he slipped on an icy dock at work around 1995 that never healed properly. Subsequent to the last severe inversion injury, he had chronic right ankle pain and instability even on flat ground that precluded him from his desired goals of golfing or walking for exercise. He trialed symptomatic relief measures and structural control with valgus wedged in-shoe inlays, lateral build-ups on the sole of his shoe and custom bracing all of which failed to relieve his symptoms or improve his function. The documented clinical exam revealed a grossly unstable ankle to inversion stress that could be corrected to nearly a neutral ankle with valgus stress. Weightbearing radiographs of his ankle revealed end-stage degenerative joint disease with a 21° incongruent ankle varus(Figure 1) and a computerized tomography scan revealed medial osseous gutter impingement.
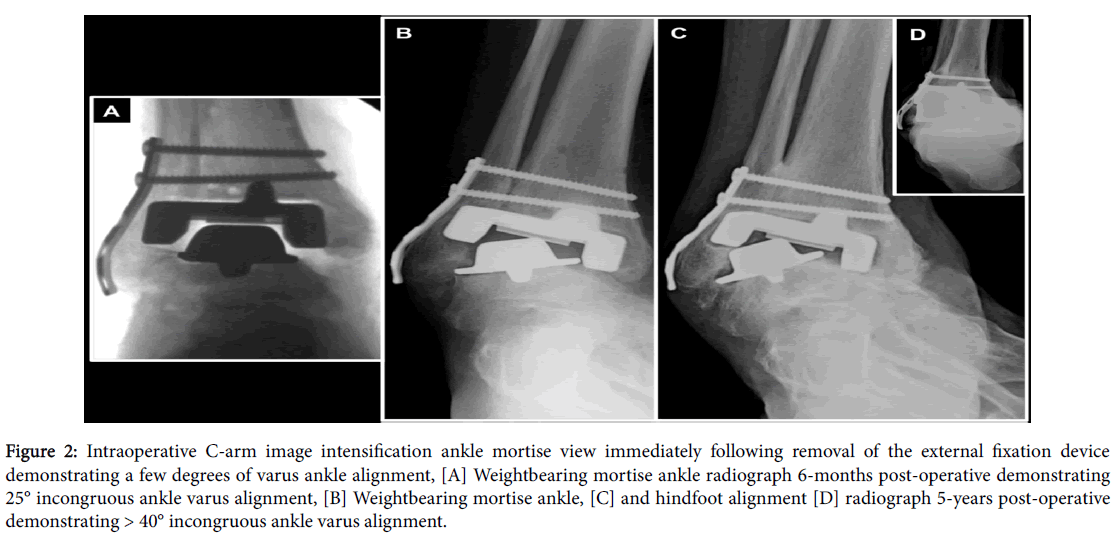
He declined an ankle arthrodesis for fear of not being able to play golf and instead underwent an Agility™ LP TAR system size 4 tibialcomponent, size 4 LP talar component and neutral 0-mm polyethylene insert in October 2008. Review of the operative report reveals the ankle was corrected to 5° of varus manually but to neutral with the external fixation device. A deltoid sleeve release was performed. After removing the external fixation device the ankle was appreciated to turn into a few degrees of varus(Figure 2A) and the post-operative films demonstrate this with the first post-operative visit revealing correctable varus of a few degrees. During subsequent visits the ankle varus progressed until it worsened past the pre-operative value of 21° to 25° (Figure 2B) at which time he was placed into a fixed angle ankle-foot orthosis, high-topped lace-up boots and valgus wedge insole/outersole to his shoe. He was scheduled for revision surgery in May 2009 to perform a repeat release of the deltoid ligament complex and lateral ankle ligament reconstruction along with closing wedge subtalar arthrodesis but this surgery never occurred and he did not return for surveillance. When questioned, he stated the reason he did not proceed with the surgery was that he was not having significant pain although the varus deformity made selection of shoe gear difficult and also interfered with his golfing and walking activities. Based on his outcome following the primary TAR, he was also uncertain if the ankle could predictably be corrected such that he would have improved function.
Figure 2:Intraoperative C-arm image intensification ankle mortise view immediately following removal of the external fixation device demonstrating a few degrees of varus ankle alignment, [A] Weightbearing mortise ankle radiograph 6-months post-operative demonstrating 25° incongruous ankle varus alignment, [B] Weightbearing mortise ankle, [C] and hindfoot alignment [D] radiograph 5-years post-operative demonstrating > 40° incongruous ankle varus alignment.
The author evaluated him in September 2013. He could only comfortably ambulate in plastic clog shoes as he struggled with any shoe that had ankle support or a heel counter due to pressure about the lateral ankle deformity. He used a single point cane as a gait aide. Clinical examination demonstrated that the right ankle TAR ankle was fixed in varus> 40° and equinus of 5° with no mobility in the frontal plane or sagittal plane appreciated. There was global pain with any attempt at ankle movement. Overall foot posture and alignment was a cavus foot posture with varus heel originating from the ankle with no plantarflexed first ray, peroneus longus overdrive or intrinsic muscle atrophy appreciated. Although limited due to the rigid deformity, his muscle strength for all prime movers of the foot and ankle were graded at 5/5 to manual stress except for the peroneus brevis that appeared absent. He walked with a limp and avoided pushing-off the TAR foot. Multiple weightbearing views of the right ankle including sagittal plane stress views demonstrated no meaningful dorsiflexion or plantarflexion and heel varus of 42°. The tibial and talar components were mal-aligned in 41° varus with the lateral wing of the talar component eroding a hole in the fibula and appearing fixed in place (Figures 2C and 2D). The syndesmosis was solidly united and the lateral side plate and screw fixation sound.
Based on the progression of his varus deformity and degree of problems he was having with his ankle the potential for a meaningful revision without major complication over time would decrease to a point where he would either have to live with the condition, use supportive aides at all times or have the leg amputated below-the-knee. He had contemplated amputation but did not desire this as an index revision procedure; however, he also did not want to continue to live with the pain/problems or use brace therapy permanently due to prior poor results.
Based on the above, the author discussed one of two meaningful options: (1) explantation of the Agility™ LP prosthesis and deep hardware with release of the deltoid ligament, release the laciniate ligament to limit potential for nerve compression injury due to deformity correction, percutaneous Achilles tendon lengthening, posterior tibial tendon intramuscular recession lengthening and once reduction was anatomic, tibio-talo-calcaneal arthrodesis with a bulk femoral head allograft using a retrograde locked intramedullary nail; or (2) explantation of the Agility™ LP prosthesis and deep hardware with conversion to an INBONE™ II total ankle replacement system including frontal plane alignment to neutral with release of the deltoid ligament, release of the laciniate ligament, percutaneous Achilles tendon lengthening, posterior tibial tendon intramuscular recession lengthening and modified Evans peroneus longus lateral ankle stabilization secured to the anterior-medial tibia and talar neck. We discussed, and he agreed, that the most appropriate course of action would be for him to be consented for both approaches and if it was not possible to convert to an INBONE™ II prosthetic device then the arthrodesis would be performed and, in this manner, he would not awaken from surgery with another TAR that would not function well for him. The revision surgery was performed in November 2013.
Surgical Procedures
A popliteal and saphenous nerve block to his right lower leg was performed in the pre-operative holding area by the anesthesia service. The patient was then brought into the operating room and placed in the supine position. The anesthesia services then performed general anesthesia with oral endotracheal intubation. A validated surgical preparation involving the foot, ankle and lower leg using a 3-minute scrub with foam sponges impregnated with chlorhexidinegluconate (4%) solution followed by painting with ethyl alcohol and iodine (1%) topical solution (1 gm iodine/100- ml ethyl alcohol) (Spectrum Chemical Manufacturing Corporation, Gardena, CA) was performed[12]. Per the authors revision TAR protocol,[13] the toes were covered with an impermeable incise barrier, the exposed skin is intermittently re-painted with Betadine Solution (10% povidone iodine solution, Purdue Products, LP, Stamford, CT) and the surgical site was serially irrigated with a pulsed lavage system impregnated with 50,000 IU Bacitracin solution (Pfizer, Inc., New York, NY) per 3-liter bag. The operating room had a laminar flow system without ultraviolet lights. Each member of the surgical team wore double surgical masks or a surgical hood/space suit based on personal preference.
Attention was directed to the lateral ankle were under direct C-arm image intensification the most inferior lateral screw was removed without incident. The second more superior screw was left to provide fibular support during removal of the tibial tray due to the ballooning osteolysis erosion of the fibula in an attempt to limit fracture at this level.
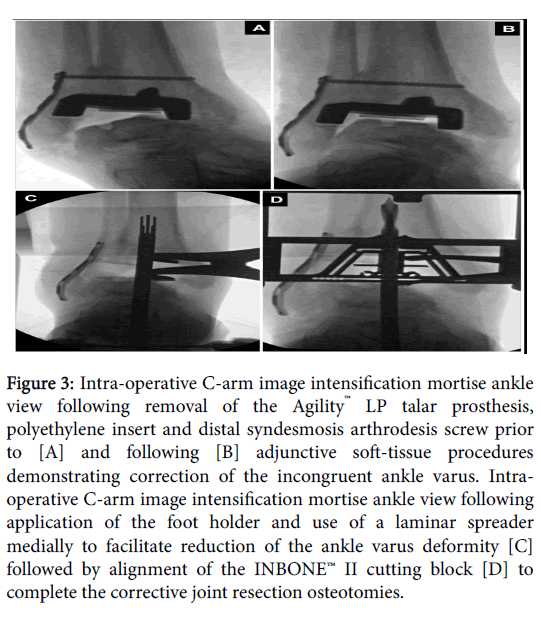
Next, attention was directed to the previous anterior skin incision that was extended proximally and distally and carried down to the level of extensor retinaculum. During this exposure, the medial branch of the superficial peroneal nerve was freed from surrounding scar tissue. Using the extensor hallucislongus as a landmark, the extensor sheath was incised and the tendon moved laterally allowing visualization of the neurovascular bundle that was mobilized off of the underlying bone and protected laterally. The anterior tibial tendon sheath was never incised and the tendon never exposed. The periosteum was elevated off of the anterior tibia and talus and exposed the ankle joint that was filled with scar tissue. This was resected with a combination of hand instruments. The ankle was contracted into a varus position and the implant components wedged together in this posture as expected from the pre-operative radiographs and clinical examination. The talar component was removed and noted to have poor osseous ongrowth. The polyethylene insert was also removed and revealed a deep groove consistent with severe edge loading. Much polyethylene particular wear debris was appreciated in and around the joint and this was removed in its entirety. The tibial component was firmly bonded to the adjacent bone requiring this to be cut free from the medial, superior, and lateral adjacent bone. The syndesmosis site was directly visualized and revealed good osseous stability consistent with the pre-operative imaging. The remaining lateral screw was removed without incident at this time but the side plate retained as it was firmly adhered to the fibula and believed to limit fibular fracture if retained. The foot was noted to be fixed in varus and could only be corrected a few degrees towards neutral following removal of the TAR (Figure 3A). Accordingly, several secondary procedures were required to achieve neutral alignment.
Figure 3:Intra-operative C-arm image intensification mortise ankle view following removal of the Agility™ LP talar prosthesis, polyethylene insert and distal syndesmosis arthrodesis screw prior to [A] and following [B] adjunctive soft-tissue procedures demonstrating correction of the incongruent ankle varus. Intraoperative C-arm image intensification mortise ankle view following application of the foot holder and use of a laminar spreader medially to facilitate reduction of the ankle varus deformity [C] followed by alignment of the INBONE™ II cutting block [D] to complete the corrective joint resection osteotomies.
First, intramuscular recession lengthening of the posterior tibial tendon [14,15] was performed. A linear incision was at the medial aspect of the operative lower extremity slightly inferior to the junction of the middle and distal one-thirds of the lower leg overlying the posterior-medial border of the tibia. The incision was deepened to the junction of the posterior tibialmusculotendinous junction that was verified with manual traction on the posterior tibial tendon through eversion and dorsiflexion of the foot. With the foot held in dorsiflexion and eversion the posterior tibial tendon was transected within the muscle belly.
Next, the laciniate ligament was deemed taught and concern raised regarding compression of the neurovascular bundle with full reduction of the varus[15]. Attention was directed to the medial aspect of the tarsal tunnel region of the ankle and lower leg where a short Dellon-type incision was placed overlying the tarsal canal and the flexor retinaculum/laciniate ligament was incised overlying the inferior aspect of the flexor digitorumlongus tendon. Additionally, a small portion of fascia at the deep surface of the abductor hallucis muscle belly was resected and the talo-navicular joint capsule incised vertically to allow for correction of the varus tethering of the talus. The foot was mobilized at the ankle and hindfoot and revealed no further evidence of fascial compression (Figure 3B).
Next, the remaining syndesmosis arthrodesis screw was removed but the fibular side plate retained to limit fracture of the fibula. The foot-holder was then applied for the INBONE™ II total ankle system and the alignment verified in the anterior-posterior, oblique, and lateral planes utilizing the alignment guide-rod instrumentation and intra-operative C-arm image intensification[16]. With the joint surface maintained in corrected position using laminar spreaders (Figure 3C)[17], the primary drill hole was placed through the calcaneus/talus and into the distal tibia along the axis of the guide-rods. The distal tibia and talar joint surfaces were then resected (Figure 3D) and contoured with care taken to protect the residual medial and lateral malleoli from fracture and the neurovascular and tendon structures especially within the posterior medial depths of the incision.
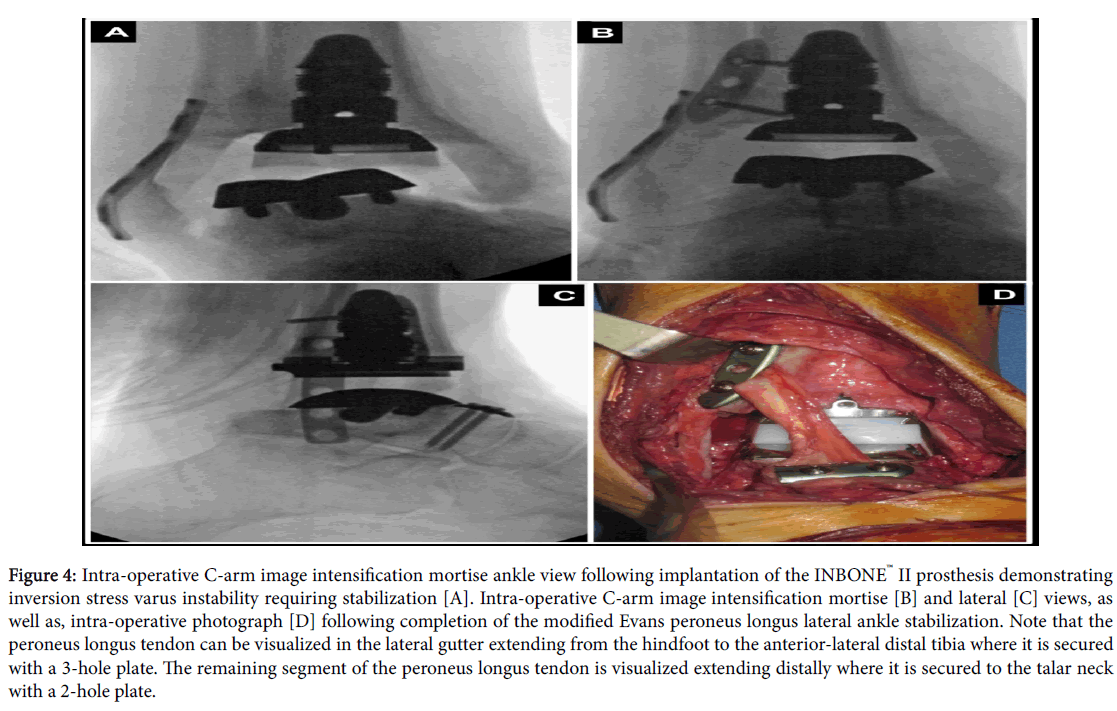
Complete resection of the remaining distal tibia and talus was verified with visual and tactile inspection, as well as, C-arm image intensification. The distal tibia was then reamed followed by insertion of a trial tibial tray base that appeared to seat with no frontal, sagittal, or transverse plane abnormality as verified with intra-operative C-arm image intensification views. Next, the tibial stems were sequentially inserted followed by the tibial base tray and the position and alignment was verified with intra-operative C-arm image intensification views. It should be noted that the tibial base tray was inserted with a thin layer of antibiotic impregnated polymethylmethcrylate cement (Simplex P with Tobramycin, Stryker Orthopaedics, Mahwah, NJ) coating the anterior ¼ of the component. The foot was removed from the foot holder at this time. The trial polyethylene insert was replaced and the trial talar dome inserted followed by range of motion of the ankle in the sagittal plane that revealed a taught Achilles tendon in need of lengthening. Accordingly, the topographic anatomy of the Achilles tendon was outlined and three incisions were utilized on the posterior midline aspect of the Achilles tendon to perform percutaneous lengthening [18]. After verifying the ability to dorsiflex the foot at the ankle appropriately, we sought out to determine the proper alignment of the talar component to optimize talar coverage. This required a release of the deep deltoid ligament off of the talar body and neck [3,4,19] to allow for some frontal plane de-rotation of the talus and proper coverage/alignment to the talar component. We purposely placed the talar component anteriorly for some posterior stabilization of the foot relative to the ankle and therefore limit anterior subluxation of the talar component relative to the polyethylene insert [20]. Next, with the tibial tray protected for damage, the talus was reamed to accept the anterior pegs and talar stem with care taken to verify proper alignment as verified on intra-operative C-arm image intensification views. The talar stem and talar dome were then inserted with a layer of antibiotic impregnated polymethylmethcrylate cement added to the anterior ¼ undersurface of the talar component between the small anterior pegs. The appropriate sized trial polyethylene insert was then placed securely into the joint space and articulation with the tibial tray verified. The surgical site was the copiously irrigated with pulse lavage including 3 liters sterile saline impregnated with 50,000 IU Bacitracin solution. The INBONE™ II prosthesis final component specifics were: tibial top-stem: 16-mm, mid-stem: 16-mm and 18-mm; tibial prosthesis size 4 long; talar sulcus dome size 3; stem length 10-mm; polyethylene sulcus insert size 3+ with 10-mm thickness. The ankle was then placed through full range of motion and revealed appropriate range of motion in the sagittal plane but inversion instability and development of a jumped facet with inversion movement (Figure 4A). Therefore it was deemed necessary to perform a modified Evans lateral ankle stabilization using the peroneus longus tendon[15,21].
Figure 4:Intra-operative C-arm image intensification mortise ankle view following implantation of the INBONE™ II prosthesis demonstrating inversion stress varus instability requiring stabilization [A]. Intra-operative C-arm image intensification mortise [B] and lateral [C] views, as well as, intra-operative photograph [D] following completion of the modified Evans peroneus longus lateral ankle stabilization. Note that the peroneus longus tendon can be visualized in the lateral gutter extending from the hindfoot to the anterior-lateral distal tibia where it is secured with a 3-hole plate. The remaining segment of the peroneus longus tendon is visualized extending distally where it is secured to the talar neck with a 2-hole plate.
Accordingly, a linear incision was at the lateral aspect of the operative lower extremity slightly superior to the junction of the middle and distal one-thirds of the lower leg overlying the peroneal tendons. The incision was deepened through the subcutaneous tissues to the level of the peroneal tendon sheath that was incised to expose the peroneus longus tendon verified with manual traction as intact. The peroneus brevis tendon had clearly been ruptured as suspected on clinical examination and likely contributed to his progressive varus ankle deformity. The peroneus longus tendon was dissected distally and transected proximally to obtain the maximum length. Next, the foot was held in eversion and posteriorly translated in the ankle and the peroneus longus tendon was brought into the anterior incision and secured to a side plate placed anterior-lateral and compressed between the plate-bone-and screws. This achieved excellent stability and limited the inversion movement. The appropriate sized final polyethylene insert was then placed securely into the joint space impacted until fully engaged. There was still a tendency to have the foot anteriorly sublux slightly and as a result a two hole plate was placed on the anterior talar neck and the remaining peroneus longus tendon brought under the plate and tensioned to act as a check-rein against anterior translation of the foot. This proved very sound and no inversion or anterior migration was evident under stress examination (Figures 4 B through 4D). The redundant tendon was sutured back on itself. The surgical site was then copiously irrigated using pulse lavage with an additional 3 liters sterile saline impregnated with 50,000 IU Bacitracin solution. A closed-suction drain was sewn in place and the deep tissues were approximated in layered fashion with absorbable suture and the skin edges approximated without tension using non-absorbable sutures.
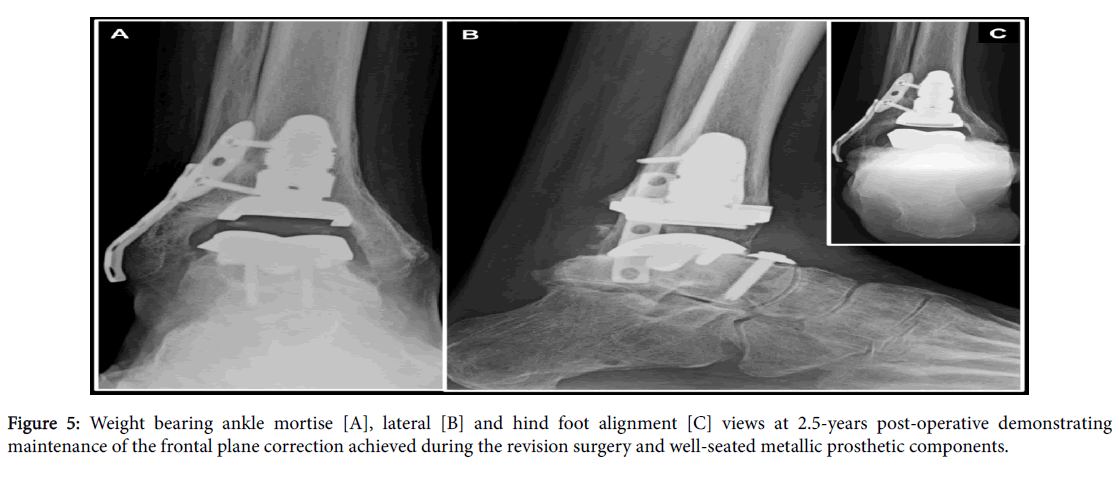
An anterior windowed folded WebrilUndercast Padding (Kendall-Coviden, Mansfield, MA) cutout to the anterior incision line[22] was applied with additional Sir Robert Jones compression dressing and posterior molded plaster splint[23]. The anterior windowed folded WebrilUndercast Padding limits contact pressure on the tenuous anterior incision and the Sir Robert Jones dressing affords edema reduction during the postoperative period. A standard post-operative protocol for TAR was employed[24] that includes: hospital admission, 48-hours of intravenous antibiotic therapy with a first generation cephalosporin, strict bed rest protocol with lower extremities elevated above heart level and heels offloaded using pillow cocoon and a semi-Fowler bed positioning protocol. Although anecdotal, supplemental oxygen via nasal cannula during the hospitalization was employed as it may reduce incision and ischemia-related wound healing problems. The patient was maintained on a strict mechanical and pharmacologic thromboembolic prophylaxis protocol until return to full weightbearing and activity was realized at 12-weeks. He then transitioned to full weightbearing and back into a supportive lace-up high-topped boot with fixed angle ankle-foot orthosis employed for 1-year post-operative. An annual surveillance program employed by the author ensued. Although controversial, dental antibiotic prophylaxis will continue lifelong. At 2.5-years follow-up the ankle was stable to manual stress and weightbearing radiographs demonstrated no change in position or alignment of the osseous structures and prosthetic components (Figure 5). At the time of most recent follow-up the patient had no pain, ambulated without a brace or modified shoes and only intermittently employed a single point cane for balance. He continues golfing and walking for exercise.
Discussion
Myriad osseous and soft-tissue procedures have been described to address varus ankle deformity during TAR[1-8,25]. However, only one case of a severe > 40° varus corrected during primary TAR exists and this required tibialis anterior tendon transfer with lengthening, posterior tibialtenotomy, lateral ankle ligament reconstruction and dorsiflexory first metatarsal osteotomy, as well as, secondary tarsal tunnel release to address acute tibial nerve compression [9]. To the authors knowledge, the current report is the first report involving revision TAR for severe >40° varus ankle deformity. This involved explanation of the failed Agility™ LP TAR and conversion to an INBONE™ II prosthesis with corrective osteotomy through the ankle joint, percutaneous Achilles tendon lengthening, tarsal tunnel decompression through release of the laciniate ligament, posterior tibial tendon recession and modified Evans peroneus longus lateral ankle stabilization. The specific procedures selected warrant further discussion.
Traditionally, transection or fractional lengthening of the tibialis posterior tendon itself has been used to correct a varus ankle contracture[2,3,7,8].This can be difficult to perform and unreliable. Instead of lengthening the tendon itself, the technique the author employs involves recession of the tibialis posterior tendon at the musculotendinous junction in the lower leg [14]. This technique represents a safe, straight-forward, minimally invasive and reproducible procedure that can effectively correct the ankle varus deformity associated with primary or revision TAR. This approach is advantageous when additional incisions on the foot or adjacent to the medial malleolus could result in wound healing problems or excessive lengthening that could result in overcorrection or instability. The use of reproducible topographic anatomic landmarks is essential to perform the technique properly and limit the potential for complications.
The flexor retinaculum is continuous with most of the bands or fibers of the superficial deltoid ligament layer and, as such, can also tether the hindfoot in varus even after sequential release of the deep deltoid off of its osseous origin(s) and/or insertion(s). In these situations, we elect to perform flexor retinaculum release, which is commonly referred to as tarsal tunnel decompression[15]. Unlike with the surgical treatment of tarsal tunnel syndrome, it is not routinely necessary to release the deep fascia in the lower leg or fibrous septum about the deep surface of the abductor hallucis muscle[26]. However, these steps may be required in severe varus ankle deformities ≥ 25° when acute correction would result predictably in compression of the neurovascular components of the entire tarsal tunnel. It should be noted that the neurovascular contents of the tarsal tunnel are not actually manipulated to limit the potential for scar formation and subsequent nerve entrapment. Likewise, the skin is closed in a single layer without re-approximation of the deeper tissues to avoid compression of the neurovascular bundle.
When modifications of the Broström-Gould lateral ankle stabilization are not sufficient then procedures involving tendon transfer are warranted. A well-known and simple non-anatomic lateral ankle stabilization procedure was described by David L. Evans[27].Evans described a release of the peroneus brevis tendon at the musculotendinous junction, transfer through a drill hole in the fibula from anterior-distal to posterior-proximal followed by suturing of the peroneus brevis tendon back to itself in a shortened fashion.The author has employed a modification of the Evans tendon transfer in which the peroneus brevis or peroneus longus tendon is harvested through limited lateral incisions using simple topographic anatomical landmarks[21]. The harvested peroneal tendon is then transferred deep along the calcaneus and talus and secured to the anterior-distal tibia with plate and screw fixation. The redundant tendon can be secured to the talar neck with plate and screw fixation should additional restraint against anterior subluxation be required. Although non-anatomic, the modified Evans tendon transfer employed by the author is useful in providing lateral ankle and subtalar stability associated with varus unstable ankles when performing primary or revision TAR.
Explantation of failed Agility and Agility™ LP TAR Systems with conversion to the INBONE II total ankle system has been reported previously and is considered a limb-salvage procedure. DeVries et al.[28] reported an incidence of complications of 64.3% (9/14) with Agility TAR explantation and conversion to the INBONE™ I total ankle system. Meeker et al.[29] reported an incidence of complications of 27.7% (5/18) with Agility™ TAR explantation and conversion to the INBONE™ II total ankle system. Williams et al.[30] from the same institution as Meeker et al.[29] reported an overall incidence of complications of 31.4% (11/35) with Agility™ TAR explantation and conversion to the INBONE™ II total ankle system. Roukis et al. [13] detailing their learning curve experience with revision TAR, reported an incidence of complications of 75% (6/8) with Agility™ TAR explantation and conversion to the INBONE™ II total ankle system. In summary, the overall incidence of complications with Agility™ TAR explantation and conversion to the INBONE™ I or II total ankle systems was 41.3%. Although it is obviously beneficial to have a TAR system capable of revising the massive osseous defects created with explantation of the Agility™ TAR system, the incidence of complications utilizing the INBONE™ I or II total ankle systems is unacceptable. Although not available for use in the United States, the HINTEGRA™ ankle prosthesis (Newdeal, Lyon, France/Integra) has readily available revision TAR components capable of revising failed STAR™ prostheses[31,32].
Explantation of a failed TAR with conversion to the Salto Talaris™ XT revision ankle prosthesis (Integra Lifesciences, Plainsboro, NJ) is a promising option when limited bone loss exists, especially about the distal tibial metaphysis. Following explantation of the failed TAR, implantation of the Salto Talaris™ XT Revision ankle prosthesis involves only a few straightforward steps for accurate implantation[33,34]. The ability to mismatch the tibial and talar components one size is beneficial when the tibial defect is wider than the available talar surface such as when revising failed Agility™ TAR prostheses. Once thicker polyethylene inserts, wider tibial base plates, long-stemmed tibial and talar components, and augmented height tibial and talar components are readily available, it will afford a universal option for revision of failed TAR systems available for use in the United States[35].
Conclusions
A case involving a failed Agility™ LP prosthesis with severe > 40° varus ankle deformity that was treated with explantation and conversion to INBONE™ II prosthesis coupled with soft-tissue release/reconstruction employing percutaneous Achilles tendon lengthening, posterior tibial tendon intramuscular recession lengthening and modified Evans peroneus longus lateral ankle stabilization is presented. A prophylactic tarsal tunnel release was performed to reduce potential for post-operative nerve compression and add to the varus correction achieved. The above-described techniques offer safe and reproducible procedures that can effectively correct frontal plane varus deformities frequently encountered with revision TAR. Although at short-term follow-up this patient has restoration of a functional lower limb, explantation of failed TAR systems with conversion to alternative TAR systems is associated with myriad potential complications that can negatively affect outcome. Therefore, the surgeon and patient should expect a high incidence of complications to occur with this approach, which should be reserved for situations where alternative revision strategies are not possible and tibio-talo-calcaneal arthrodesis[35,36] is undesirable.
References
- Henricson A, Agren PH (2007) Secondary surgery after total ankle replacement, the influence of preoperative hindfoot alignment. Foot Ankle Surg 13:41-44.
- Hobson SA, Karantana A, Dhar S (2009) Total ankle replacement in patients with significant pre-operative deformity of the hindfoot. J Bone Joint Surg Br 91: 481-486.
- Kim BS, Choi WJ, Kim YS, Lee JW (2009) Total ankle replacement in moderate to severe varus deformity of the ankle. J Bone Joint Surg Br 91: 1183-1190.
- Choi WJ, Yoon HS, Lee JW (2013) Techniques for managing varus and valgus malalignment during total ankle replacement. ClinPodiatr Med Surg 30: 35-46.
- Queen RM, Adams SB Jr, Viens NA, Friend JK, Easley ME, et al. (2013) Differences in outcomes following total ankle replacement in patients with neutral alignment compared with tibiotalar joint malalignment. J Bone Joint Surg Am 95: 1927-1934.
- Sung KS, Ahn J, Lee KH, Chun TH (2014) Short-term results of total ankle arthroplasty for end-stage ankle arthritis with severe varus deformity. Foot Ankle Int 35: 225-231.
- Coetzee JC (2008) Management of varus or valgus ankle deformity with ankle replacement. Foot Ankle Clin 13: 509-520.
- Mayich DJ, Daniels TR (2012) Total ankle replacement in ankle arthritis with varustalar deformity: pathophysiology, evaluation, and management principles. Foot Ankle Clin 17: 127-139.
- Elliott AD, Roukis TS (2016) Current indications and contraindications for primary total ankle replacement: Primary and Revision Total Ankle Replacement. Springer International Publishing, Switzerland.
- Hamel J (2012) Early results after tibialis anterior tendon transfer for severe varus in total ankle replacement. Foot Ankle Int 33: 553-559.
- Hanselman AE, Powell BD, Santrock RD (2015) Total ankle arthroplasty with severe preoperative varus deformity. Orthopedics 38: e343-346.
- Roukis TS (2010) Bacterial skin contamination prior to and after surgical preparation of the foot, ankle, and lower leg in patients with diabetes and intact skin versus patients with diabetes and ulceration: A prospective controlled therapeutic study. J Foot Ankle Surg 49:348-356.
- Roukis TS, Simonson DC (2015) Incidence of Complications During Initial Experience with Revision of the Agility and Agility LP Total Ankle Replacement Systems: A Single Surgeon's Learning Curve Experience. ClinPodiatr Med Surg 32: 569-593.
- Roukis TS (2013) Tibialis posterior recession for balancing varus ankle contracture during total ankle replacement. J Foot Ankle Surg 52: 686-689.
- Roukis TS, Elliott AD (2015) Use of soft-tissue procedures for managing varus and valgus malalignment with total ankle replacement. ClinPodiatr Med Surg 32:517-528.
- Abicht BP, Roukis TS (2013) The INBONE II Total Ankle System. ClinPodiatr Med Surg 30: 47-68.
- Ellis S, DeOrio JK (2010) The INBONE total ankle replacement. Oper Tech Orthop 20:201-210.
- Schweinberger MH, Roukis TS (2008) Surgical correction of soft-tissue ankle equinus contracture. ClinPodiatr Med Surg 25: 571-585.
- Choi WJ, Lee M, Lee JW (2016) Managing varus and valgus malalignment after total ankle replacement: Primary and Revision Total Ankle Replacement. Springer International Publishing. pp: 231-240.
- Gougoulias N, Badekas T, Maffulli N (2016) Managing soft-tissue ankle equinus and anterior/posterior translation of the talus during total ankle replacement: Primary and Revision Total Ankle Replacement. Springer International Publishing, Switzerland.
- Roukis TS1 (2013) Modified Evans peroneus brevis lateral ankle stabilization for balancing varus ankle contracture during total ankle replacement. J Foot Ankle Surg 52: 789-792.
- Elliott AD, Roukis TS (2016) Anterior incision off-loading for primary and revision total ankle replacement: A comparative analysis of two techniques. The Open Orthopaedics Journal; In Press, corrected proof .
- Schade VL, Roukis TS (2008) Use of a surgical preparation and sterile dressing change during office visit treatment of chronic foot and ankle wounds decreases the incidence of infection and treatment costs. Foot Ankle Spec 1:147-154.
- Schweinberger MH, Roukis TS (2010) Effectiveness of instituting a specific bed protocol in reducing complications associated with bed rest. J Foot Ankle Surg 49: 340-347.
- Walcher MG, Barg A, Rudert M, Hoberg M, Valderrabano V (2014) Total ankle replacement in varus ankle osteoarthritis. Clin Res Foot Ankle.
- Heimkes B, Posel P, Stotz S, Wolf K (1987) The proximal and distal tarsal tunnel syndromes. An anatomical study. IntOrthop 11: 193-196.
- EVANS DL (1953) Recurrent instability of the ankle; a method of surgical treatment. Proc R Soc Med 46: 343-344.
- DeVries JG, Scott RT, Berlet GC, Hyer CF, Lee TH, et al. (2013) Agility to INBONE: anterior and posterior approaches to the difficult revision total ankle replacement. ClinPodiatr Med Surg 30: 81-96.
- Meeker J, Wegner N, Francisco R, Brage M (2013) Revision techniques in total ankle arthroplasty using a stemmed tibialarthroplasty system. Tech Foot Ankle Surg 12:99-108.
- Williams JR, Wegner NJ, Sangeorzan BJ, Brage ME (2015) Intraoperative and perioperative complications during revision arthroplasty for salvage of a failed total ankle arthroplasty. Foot Ankle Int 36: 135-142.
- Hintermann B, Zwicky L, Knupp M, Henninger HB, Barg A (2013) HINTEGRA revision arthroplasty for failed total ankle prostheses. J Bone Joint Surg Am 95: 1166-1174.
- Brunner S, Barg A, Knupp M, Henninger HB, Barg A (2013) The Scandinavian Total Ankle Replacement: Long-term, eleven to fifteen-year, survivorship analysis of the prosthesis in ?seventy-two consecutive patients. J Bone Joint Surg Am 95:711-718.
- Roukis TS1 (2015) The Salto Talaris XT Revision Ankle Prosthesis. ClinPodiatr Med Surg 32: 551-567.
- Gaudot F, Judet T, Colombier JA, Bonnin M (2016) The Salto Talaris XT revision total ankle replacement system: Primary and Revision Total Ankle Replacement. Springer International Publishing, Switzerland.
- Roukis TS (2014) Strategies for revision total ankle replacement. Journal of Orthopaedics, Trauma and Rehabilitation 18: 59-68.
- Donnenwerth MP, Roukis TS (2013) Tibio-talo-calcaneal arthrodesis with retrograde compression intramedullary nail fixation for salvage of failed total ankle replacement: a systematic review. Podiatr Med Surg 30: 199-206.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 16442
- [From(publication date):
July-2016 - Mar 29, 2025] - Breakdown by view type
- HTML page views : 15258
- PDF downloads : 1184