Factors That Moderate or Mediate Pregnancy Complications in Women with Anxiety and Depression
Received: 10-Nov-2017 / Accepted Date: 20-Dec-2017 / Published Date: 27-Dec-2017 DOI: 10.4172/2376-127X.1000360
Abstract
Background: Maternal anxiety and depression is noted in approximately 10-20% of pregnant women and can impact pregnancy and neonatal health, however, little is known about the factors. This study explored the roles of specific risk factors such as age, marital status, stress, substance use and ethnicity as either a moderator or a mediator to better understand the relationship between maternal anxiety or depression and major pregnancy complications and birth outcomes.
Methods: A cohort of 646 women were studied longitudinally over three time points in early and late pregnancy and early postpartum. Maternal anxiety and depression were considered primary predictors with pregnancy complications i.e., gestational diabetes, edema and birth outcomes, i.e., low birth weight or preterm birth, as outcome variables. Socio-demographic factors were examined as moderator variables and psychosocial and behavioral factors were considered as mediator variables. For moderating and mediating analyses, a series of logistic regression analyses were performed.
Results: Almost one-quarter of the women reported to have two or more pregnancy complications, 5.7% had a pre-term birth and 7.6% had a low birth weight baby. Stress in late pregnancy showed both a partial and a full mediating pathway between maternal anxiety and depression and pregnancy complications such as gestational diabetes, hypertension and edema. History of sexual abuse, single or divorced marital status, younger maternal age and Aboriginal ancestry had moderating effects in early and late pregnancy for adverse pregnancy and birth outcomes (i.e., low birth weight).
Conclusion: Identifying mothers with stress, history of abuse, unpartnered, younger and of Indigenous ancestry will help clinicians and policy makers target timely interventions for pregnant women with anxiety and depression symptoms.
Keywords: Depression; Anxiety; Pregnancy outcomes; Moderator; Mediators
Introduction
Pregnancy marks a time of role change and transition, not only physically, but also socially and psychologically [1,2]. Up to 60% of women experience anxiety and/or depression during or after pregnancy [3-5]. The reported prevalence of antenatal anxiety varies widely from 9.1% to 59.5% [6,7]. Approximately 10% to 20% women suffer from antenatal and postnatal depression, with the prevalence of depression reported higher in pregnancy than postpartum [3]. Bowen et al. [8] found that prevalence of depression among socially vulnerable pregnant women is 29.5% with thee prevalence of depression greater in the first trimester at 11%, dropping to 8.5% in the second and third trimesters.
Depression in pregnancy profoundly affects a woman’s daily activity, relationships and overall sense of well-being [9,10]. It is seen as a major risk factor in developing postnatal depression, adverse obstetric complications, birth outcomes and fetal growth restriction [6,11]. Maternal anxiety is associated with intrauterine growth restrictions, impaired fetal growth i.e., preterm birth, short gestational period and lack of motor development in the offspring [12,13].
Factors associated with antenatal anxiety and depression include abuse (i.e., physical, emotional or sexual), low social support, low income, unplanned pregnancy, history of depression and immigrant or Aboriginal ethnicity status [14,15]. Depression during pregnancy is also associated with increased risk behaviours such as tobacco smoking, lack of physical activity, alcohol consumption and recreational drug use [16-18].
While studies indicate an association between depression and pregnancy complications and poor birth outcomes such as preterm birth, low birth weight and lower Apgar scores, there is sparse evidence that show in detail the role of underlying factors, beyond as confounders in this relationship [4,19]. Specifically, major risk factors such as experiencing abuse, behavioral and psychosocial factors i.e., smoking, drinking alcohol, poor physical activity, stressors, etc., are not only just confounders, but they may either moderate (mitigate or exacerbate effects) or mediate the effects (show specific pathways) between anxiety and depression and pregnancy complications and poor delivery outcomes. Rahman et al. reported significant moderating and mediating effects of potential risk factors in developing depression throughout the pregnancy period from this same cohort [3]. In epidemiological studies, it is necessary to disentangle the causal pathway of the risk factors that link the exposure to the outcome [20]. Longitudinal studies of pregnant women followed throughout the pregnancy to postpartum period presents an opportunity to clarify the relationships between depression and anxiety, measured at specific times in pregnancy and pregnancy and birth outcomes.
Despite increasing literature suggesting a linkage between depression and anxiety and pregnancy complications and birth outcomes, there is a paucity of knowledge in understanding the mechanism or causal pathways of these risks [21,22]. Therefore, the purpose of this paper is to answer the research question, what are the moderating and mediating effects of a set of variables such as experiencing physical, emotional or sexual abuse or alcohol, tobacco or recreational drug use, stress and social support, measured at different times during pregnancy on the relationship between antenatal depression and anxiety and pregnancy and birth outcomes. We hypothesize that anxiety and depression increase the risk for pregnancy and birth outcome complications and risk factors that may mediate or moderate these effects.
Materials and Methods
Sample
The Feelings in Pregnancy and Motherhood study (FIP) is a longitudinal epidemiological study of maternal mental health in 646 women at three time points, Time 1=early pregnancy (17.4 ± 4.9 weeks), Time 2=late pregnancy (30.6 ± 2.7 weeks) and Time 3=postpartum (4.2 ± 2.1 weeks). Data were collected through face to face interviews by trained research assistants using self-reported questionnaires. Ethical approval was obtained from the Office of Research Ethics at University of Saskatchewan. Participants provided informed written consent.
Measures
To measure the primary predictor variables, anxiety and depression during pregnancy the Edinburgh Postnatal Depression Scale (EPDS), was used to assess symptoms at all three-time points [23,24]. The validity of the EPDS has been widely documented with the internal consistency of the EPDS has previously been found to be satisfactory [3,23]. The scale has a sensitivity ranging from 34% to 100% and a specificity ranging from 49% to 100%. The score can range from 0 to 30 [23]. For this study, the cut-off score for depression on the EPDS was defined as a score of 12 or more [25]. Anxiety defined as a score 4 or more on the anxiety subscale within the EPDS (items 3, 4 and 5), with a maximum score of 9 [4,25]. The outcome variables included pregnancy complications (gestational diabetes, gestational hypertension, edema, swelling, bleeding and abruption) and birth outcomes (preterm birth and low birth weight) at time 3 (early postpartum) [26]. For poor birth outcomes, participants who gave birth before 37 weeks were considered as preterm birth. Low Birth Weight (<2500 g) of the term newborn were also considered as poor birth outcomes [6,27-29]. Sociodemographic data (i.e., age was collected as a continuous variable and collapsed into below 25 and 25 and above, ethnicity was categorized as Aboriginal or Non-aboriginal, which included Caucasian and a small amount of other ethnicities), income was collected in five categories and collapsed into income below $40,000 and greater than $40,000, education was collapsed into two categories less than grade 12 and greater than grade 12 and marital status was collapsed into two categories-single/divorced and widowed or married/partnered) were collected. Women were asked about their history of emotional, sexual or physical abuse. They were also asked about their sources of social support (a list of supports i.e., partner, mother, female relatives, father, others) and satisfaction with their partner relationship and were asked to identify different types of stressors they were experiencing from a list that included “being pregnant, partner relationship, family, finances, birth of the baby, health of the baby, their own health, work, school and where I live” were counted as sum of stressors for the analysis. Women were asked whether they presently, previously or never used tobacco, alcohol and recreational drugs, this was categorized into yes or no to present use of these substances.
Analysis
Bivariate analysis was performed to understand the associations between the independent and dependent variables where depression and anxiety were considered as primary predictors. Covariables included maternal age, education, ethnicity, marital status, social support, stress, satisfaction with the current relationship, exercise, smoking, drinking alcohol, using other recreational drugs. To analyze the moderator and mediator variables, the p-value was set to ≤ 0.1 for significance,
Moderating analysis
To test the moderating effect, hierarchical regression procedures were performed [3,30]. At step 1, the primary predictor variables i.e., anxiety and depression at Time 1 were entered into the regression equation to predict pregnancy complications and birth outcomes at Time 3. At step 2, the moderating variables, any type of abuse, age, ethnicity, education, income, marital status were entered into the regression equation. Finally, at step 3, the product term of predictor variable and moderator variables were included once they were significant (p ≤ 0.1) at step 2. Product terms that were significant at step 3, were kept in the model and indicated as a significant moderator effect.
Mediating analysis
According to Barron and Kenny, mediating analysis involves four steps [30]. Step 1, examines whether there is a significant relationship (p ≤ 0.1) between the predictor and outcome. Step 2 specifies that the predictor variable must be related to the mediator variable. Step 3 examines whether the mediator variable is related to the outcome variable and that it is predicted to influence the effects of the predictor on the outcome. Finally step 4 indicates that the coefficient relating to the independent variable and the dependent variable is larger (in absolute value) than the coefficient relating the independent variable and the dependent variable in the regression model with both the independent and the mediating variable included [31]. If the independent variable is no longer significant (p-value >0.1 in this study) while controlling for the mediator variable, then the result supports full mediating effect. If the independent variable is found to be still significant (p ≤ 0.1) along with the mediator variable in the regression model, the finding supports a partial mediating effect.
Results
In this longitudinal population-based study, of the initial 646 women who were recruited, thirty-five women were lost to followup and twenty-one women did not finish the study mostly due to miscarriage and stillbirth. However, 646 women completed the questionnaire at early pregnancy (Time 1), 596 (91.8%) women completed the study at early postpartum (Time 3). The women were assessed at three points of time (Time 1=early pregnancy (17.4+4.9 weeks), Time 2=late pregnancy (30.6+2.7 weeks) and Time 3=postpartum (4.2+2.1 weeks). The average age of the women was 28.9+/-4.8 years, Table 1 describes the sociodemographic characteristics of the study population (Table 1).
| Variables | Participant’s n (%) |
|---|---|
| Maternal age | |
| =25 years’ old | 22.6 (146) |
| >25 years’ old | 77.4 (500) |
| Marital status | |
| Married/Common-Law | 90.2 (583) |
| Single/Divorced/Widowed | 9.8 (63) |
| Ethnicity | |
| Aboriginal | 8.5 (55) |
| Non-aboriginal | 91.3 (590) |
| Education | |
| 5.0 (32) | |
| Grade 12 or over | 94.9 (613) |
| Income | |
| <$40,000 | 31.3 (202) |
| =$40,000 | 68.7 (444) |
Table 1: Socio-demographic characteristics of study population.
Almost half of the women (47.1%, n=304) experienced anxiety symptoms (i.e., anxiety score >4) in early pregnancy, which decreased to 38.4% (n=231) in late pregnancy. The prevalence of depressive symptoms (EPDS score >12) was 14.1% (n=91) in early pregnancy (Time 1) and 10.2 % (n=61) in late pregnancy (Time 2). More than five percent of women had preterm births, whereas 7.6 % women delivered low birth weight (<2500 g) newborns. Twenty-two percent of women reported to have two or more pregnancy complications (i.e., gestational diabetes, edema/swelling, gestational hypertension, bleeding or abruption) and 3.6% women also experienced common labour complications (i.e., infection, premature rupture of membrane, postpartum hemorrhage and preterm labour).
Mediating effect
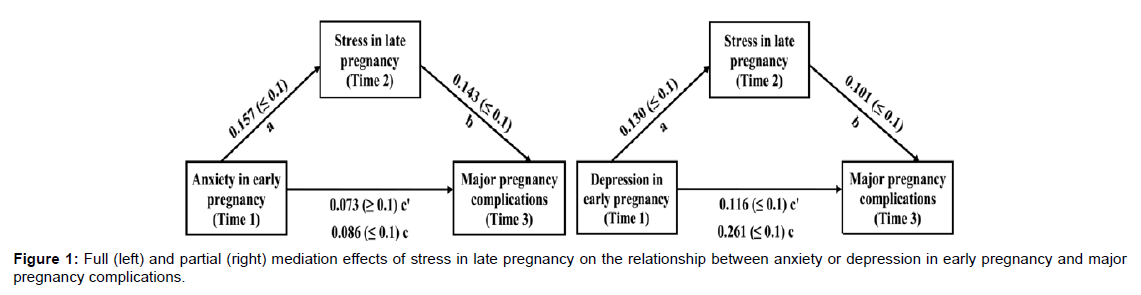
Seven mediator variables were tested for mediation analysis, but only stress was found to have significant mediation effect The sum of stressors in late pregnancy showed a fully mediated pathway between anxiety in early pregnancy and major pregnancy complications. In contrast, stressors in late pregnancy showed partially mediated pathway between depression in early pregnancy and major pregnancy complications. Complications (Figure 1).
Moderating effect
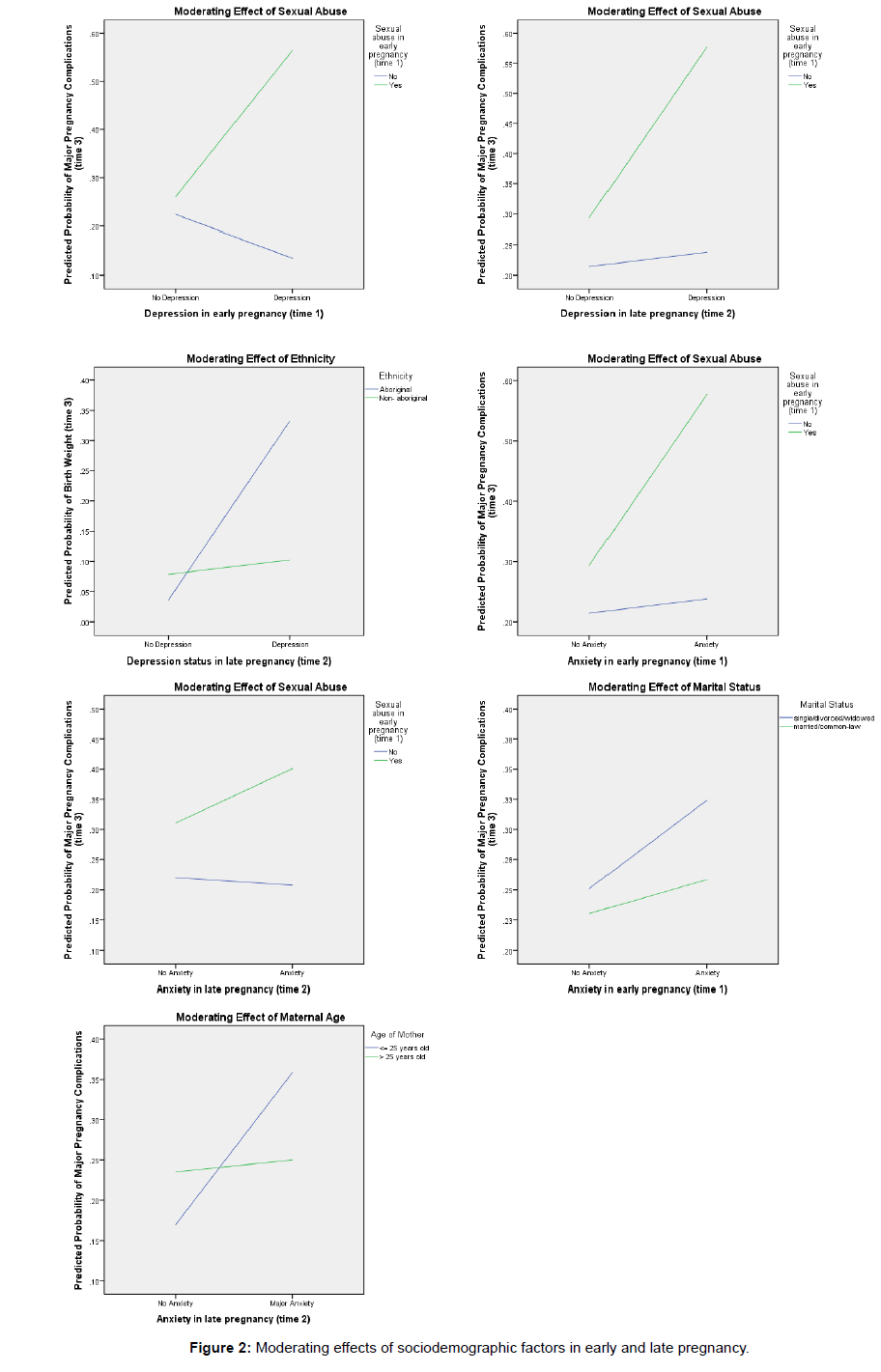
Four variables-history of sexual abuse, marital status, maternal age and ethnicity showed significant moderating effects on the relationships between depression and anxiety in early or late pregnancy and major pregnancy complications. Furthermore, the extent to which moderation was observed depended on the moderator and the time in pregnancy, depression or anxiety were reported in Figure 2.
Specifically, the effects of depression on major pregnancy complications were greater among women who had reported sexual abuse in early pregnancy than among women who had reported no sexual abuse. This was true whether women reported depression in early or late pregnancy. Moreover, the effects of depression on poor birth outcomes i.e., low birth weight were more significant among Aboriginal mothers who reported depression in late pregnancy than among non-Aboriginal participants. Like depression, the effects of anxiety on major pregnancy complications were greater among women who had reported sexual abuse in early pregnancy than among women who had reported no sexual abuse. This was true whether women reported anxiety in early or late pregnancy. Furthermore, the effects of anxiety on major pregnancy complications were significant among women who were not partnered when contacted in early pregnancy than among women who were partnered. The effects of anxiety on major pregnancy complications were greater among women less than 25 years old in late pregnancy compared to those over 25 years of age.
Discussion
Most studies related to depression or anxiety have focused on factors either as an independent risk factor or protective factor in developing depression or anxiety symptoms during pregnancy [4,19,32]. The present longitudinal study examined specific moderating and mediating roles of certain risk factors on the relationships between depression and anxiety and pregnancy complications and poor birth outcomes.
Mediating effects
To our knowledge, there is limited evidence on the mediating effect of stress on the relationship between maternal mental health and pregnancy complications. That is to say, we do not know very much what factors demonstrate a role in a potential pathway between depression and anxiety and pregnancy outcomes. This study suggests that mothers who were more anxious in early pregnancy experienced more stressors in late pregnancy resulting in more pregnancy complications.
Our results also indicate that pregnant women who experienced depression in early pregnancy were more likely to report cumulative stressors (such as concern about the health of the unborn baby, financial support or relationship with the partner, housing or inadequacy of food) in their late pregnancy, compared to women who reported not experiencing depression. Hence, women who are depressed experienced more stressors resulting two or more pregnancy complications compared with non-depressed women who reported fewer stressors. Rahman et al., showed stress as a significant mediator which either partially or fully mediated the relationship with depression in late pregnancy confirms our findings reporting stress as a strong mediator for pregnancy complications [3]. Although there is limited evidence on the mediating role of psychosocial factors, (i.e., stressors). Several studies highlighted stress as a potential risk factor in developing depression, which in turn result in more pregnancy complications and adverse neonatal outcomes [33,34]. One possible explanation might be depression during pregnancy promotes the release of stress hormones such as cortisol and decreased uterine blood flow, which leads to pregnancy complications and negative birth outcomes [10,24,32].
Moderating effects
Our findings suggest that sexual abuse moderated the relationship between early or late pregnancy maternal mental health and pregnancy complications such as gestational diabetes, hypertension. One casecontrol study in Tehran suggested that women with depression and anxiety symptoms were more prone to suffer stress during their pregnancy, which was a primary predictor in developing pre-eclampsia [35,36]. Although little is published about the moderating effects of sexual abuse for pregnancy complications, it is well documented that physical abuse or intimate partner violence (physical, sexual, verbal, or emotional) during pregnancy confers considerable risk to the health of the woman and her unborn child [37-39]. Research also confirms that different form of abuse such as physical, sexual or emotional abuse during pregnancy is associated with a number of pregnancy complications, including vaginal bleeding and abruption placenta [38,40,41]. Furthermore, preterm labour, low birth weight and preterm delivery are common consequences of different types of abuse among mothers [42-44].
Our study confirms a positive moderating effect of marital status on the relationship between anxiety symptoms and pregnancy complications, it is likely that women who are partnered, experience less stress or anxiety during pregnancy due to increased support received, in turn decreases the risk of pregnancy complications [42]. Another study also found moderating role of marital status (i.e., buffering effect) on the relationship between depression and recreational drug use [3]. Our study found a significant moderating effect of age of the mother on the relationship between anxiety and major pregnancy complications. Young mothers who reported anxiety symptoms in late pregnancy were at higher risk of experiencing multiple pregnancy complications, they may feel more anxiety about the unborn child and have poor social support during their pregnancy, resulting in more psychological stress or anxiety than older women. Rahman et al. also showed a moderating effect of younger maternal age for depression symptoms in late pregnancy [3,4,12]. Our study pointed to maternal Aboriginal ethnicity as a significant moderator of the relationship between depression and low birth weight, along with poor partner relationship and lack of social support increase the risk of developing depression symptoms [3,45]. Furthermore, depressive symptoms are higher among marginalized groups of people such as Aboriginal, immigrants and other minority women who have low resources and poor social support, which can place maternal and fetal health in jeopardy [5,46].
Limitations
As most longitudinal studies do, this study also experienced participants who were lost to follow-up, however, this was limited to 9%. The study comprised of self-reported data gathered through in-person interviews, therefore, there is a chance of recall bias. The study did not test the significance of mediating variable effects i.e., difference between total and direct effect. Despite these limitations, the key strengths of this study were a relatively large sample size and prospective nature of the data.
Conclusion
The longitudinal nature of the data allowed us to examine the underlying mechanisms with temporal precedence or in a causal pathway in the relationships between maternal depression or anxiety and major pregnancy complications. Although our findings may not be generalizable to all populations of perinatal women, the findings add to the empirical literature by reporting the moderating and mediating effects of risk factors in general, but more specifically the risk factors for pregnancy and birth outcomes. Clinicians may be better able to promote maternal and newborn wellness by identifying those women with anxiety and depression symptoms and the risk factors that increase poor pregnancy and birth outcomes to ensure timely access to treatment.
Acknowledgement
This research project was funded by Canadian Institutes of Health Research (Grant #IGP-77895). Sincere gratitude is expressed to the research team who collected the data and all of the women who participated in this study.
References
- Li J, Mao J, Du Y, Morris JL, Gong G, et al. (2012) Health-related quality of life among pregnant women with and without depression in Hubei, China. J Matern Child Health 16: 1355-1363.
- Golbasi Z, Kelleci M, Kisacik G, Cetin A (2010) Prevalence and correlates of depression in pregnancy among Turkish women. J Matern Child Health 14: 485-491.
- Rahman K, Bowen A, Muhajarine N (2014) Examining the factors that moderate and mediate the effects on depression during pregnancy and postpartum. J Preg Child Health 1: 1-8.
- Schwartz L, Bowen A, Muhajarine N (2015) The effects of episodic versus continuous and major versus mild depression and anxiety symptoms on pregnancy and labour complications. Arch Depress Anxiety 1: 010-018.
- Shah SMA, Bowen A, Afridi I, Nowshad G, Muhajarine N (2011) Prevalence of antenatal depression: Comparison between Pakistani and Canadian women. J Pak Med Assoc 61: 242-246.
- Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, et al. (2010) A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight and intrauterine growth restriction. Arch Gen Psych 67: 1012-1024.
- Faisal-Cury A, Menezes PR (2007) Prevalence of anxiety and depression during pregnancy in a private setting sample. Arch Womens Mental Health 10: 25-32.
- Bowen A, Stewart N, Baetz M, Muhajarine N (2009) Antenatal depression in socially high-risk women in Canada. J Epidemiol Comm Health 63: 414-416.
- Pearlstein T (2015) Depression during pregnancy. Best Pract Res Clin Obstet Gynae 29: 754-764.
- Becker M, Weinberger T, Chandy A, Schmukler S (2016) Depression during pregnancy and postpartum. Curr Psychiatry Rep 18: 32.
- Adewuya AO, Ola BA, Aloba OO, Dada AO, Fasoto OO (2007) Prevalence and correlates of depression in late pregnancy among Nigerian women. Depress Anxiety 24: 15-21.
- Schetter CD, Niles AN, Guardino CM, Khaled M, Kramer MS (2016) Demographic, medical and psychosocial predictors of pregnancy anxiety. Paediatr Perinat Epidemiol 30: 421-429.
- Simeone S, Lojo C, Garcia-Esteve L, Triunfo S, Crovetto F, et al. (2015) Psychological impact of first-trimester prevention for preeclampsia on anxiety. Prenat Diagn 35: 60-64.
- Inandi T, Bugdayci R, Dundar P, Sumer H, Sasmaz T (2005) Risk factors for depression in the first postnatal year: A Turkish study. Soc Psychiatry Psychiatr Epidemiol 40: 725-730.
- Toohey J (2012) Depression during pregnancy and postpartum. Clin Obstet Gynecol 55: 788-797.
- Weobong B, Ten-Asbroek AHA, Soremekun S, Manu AA, Owusu-Agyei S, et al. (2014) Association of antenatal depression with adverse consequences for the mother and newborn in rural ghana: Findings from the DON population-based cohort study. PloS One 9: e116333.
- Gaston A, Vamos CA (2013) Leisure-time physical activity patterns and correlates among pregnant women in Ontario, Canada. Matern Child Health J 17: 477-484.
- Pajulo M, Savonlahti E, Sourander A, Helenius H, Piha J (2001) Antenatal depression, substance dependency and social support. J Affect Disord 65: 9-17.
- Andersson L, Sundstrom-Poromaa I, Wulff M, Astrom M, Bixo M (2004) Neonatal outcome following maternal antenatal depression and anxiety: A population-based study. Am J Epidemiol 159: 872-881.
- Richiardi L, Bellocco R, Zugna D (2013) Mediation analysis in epidemiology: Methods, interpretation and bias. Int J Epidemiol 42: 1511-1519.
- Brittain K, Myer L, Koen N, Koopowitz S, Donald KA, et al. (2015) Risk factors for antenatal depression and associations with infant birth outcomes: Results from a South African birth cohort study. Paediatr Perinat Epidemiol 29: 505-551.
- Kurki T, Hiilesmaa V, Raitasalo R, Mattila H, Ylikorkala O (2000) Depression and anxiety in early pregnancy and risk for preeclampsia.Obstet Gynecol 95: 487-490.
- Cox JL, Holden J (2003) Perinatal mental health: A guide to the Edinburgh Postnatal Depression Scale (EPDS). RC Psych Publications, UK.
- Teissedre F, Chabrol H (2004) Detecting women at risk for postnatal depression using the Edinburgh Postnatal Depression Scale at 2 to 3 days postpartum. Can J Psychiatry 49: 51-54.
- Gibson J, McKenzieâ€McHarg K, Shakespeare J, Price J, Gray R (2009) A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand 119: 350-364.
- Engberg E, Stach-Lempinen B, Sahrakorpi N, Rönö K, Roine RP (2015) A cross-sectional study of antenatal depressive symptoms in women at high risk for gestational diabetes mellitus. J Psychosom Res 79: 646-650.
- Preti A, Cardascia L, Zen T, Pellizzari P, Marchetti M, et al. (2000) Obstetric complications in patients with depression-a population-based case-control study. J Affect Disord 61: 101-106.
- Staneva A, Bogossian F, Pritchard M, Wittkowski A (2015) The effects of maternal depression, anxiety and perceived stress during pregnancy on preterm birth: A systematic review. Women Birth 28: 179-193.
- Ding XX, Wu YL, Xu SJ, Zhu RP, Jia XM, et al. (2014) Maternal anxiety during pregnancy and adverse birth outcomes: A systematic review and meta-analysis of prospective cohort studies. J Affect Disord 159: 103-110.
- Baron RM, Kenny DA (1986) The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. J Pers Soc Psychol 51: 1173.
- MacKinnon DP, Dwyer JH (1993) Estimating mediated effects in prevention studies. Eval Rev 17: 144-158.
- Alder J, Fink N, Bitzer J, Hösli I, Holzgreve W (2007) Depression and anxiety during pregnancy: A risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Neon Med 20: 189-209.
- Dolatian M, Mahmoodi Z, Alavi-Majd H, Moafi F, Ghorbani M, et al. (2016) Psychosocial factors in pregnancy and birthweight: Path analysis. J Obstet Gynaecol Res 42: 822-830.
- Lilliecreutz C, Larén J, Sydsjö G, Josefsson A (2016) Effect of maternal stress during pregnancy on the risk for preterm birth. BMC Preg and Child 16: 5.
- Smith KF, Huber LRB, Issel LM, Warren-Findlow J (2015) The association between maternal depression during pregnancy and adverse birth outcomes: A retrospective cohort study of prams participants. J Community Health 40: 984-992.
- Kharaghani R, Geranmaye M, Janani L, Hantooshzade S, Arbabi M, et al. (2012) Preeclampsia and depression: A case-control study in Tehran. Arch Gynecol Obstet 286: 249-253.
- Alhusen JL, Lucea MB, Bullock L, Sharps P (2013) Intimate partner violence, substance use and adverse neonatal outcomes among urban women. J Pediatr 163: 471-476.
- Muhajarine N, D'Arcy C (1999) Physical abuse during pregnancy: Prevalence and risk factors. CMAJ 160: 1007-1011.
- Sharps PW, Laughon K, Giangrande SK (2007) Intimate partner violence and the childbearing year: Maternal and infant health consequences. Trauma Violence Abuse 8: 105-116.
- Daoud N, Urquia ML, O'Campo P, Heaman M, Janssen PA, et al. (2012) Prevalence of abuse and violence before, during and after pregnancy in a national sample of Canadian women. Am J Public Health 102: 1893-1901.
- Leone JM, Lane SD, Koumans EH, DeMott K, Wojtowycz MA, et al. (2010) Effects of intimate partner violence on pregnancy trauma and placental abruption. J Womens Health 19: 1501-1509.
- Alhusen JL, Ray E, Sharps P, Bullock L (2015) Intimate partner violence during pregnancy: Maternal and neonatal outcomes. J Womens Health 24: 100-106.
- Hill A, Pallitto C, McCleary-Sills J, Garcia-Moreno C (2016) A systematic review and meta-analysis of intimate partner violence during pregnancy and selected birth outcomes. Int J Gynaecol Obstet 133: 269-276.
- Leeners B, Stiller R, Block E, Gorres G, Rath W (2010) Pregnancy complications in women with childhood sexual abuse experiences. J Psychosom Res 69: 503-510.
- Cairney J, Boyle M, Offord DR, Racine Y (2003) Stress, social support and depression in single and married mothers. Soc Psych Psychiatr Epidemiol 38: 442-449
- Miszkurka M, Goulet L, Zunzunegui MV (2010) Contributions of immigration to depressive symptoms among pregnant women in Canada. Can J of Public Health 101: 358-364.
Citation: Rasul S, Bowen A, Muhajarine N (2017) Factors That Moderate or Mediate Pregnancy Complications in Women with Anxiety and Depression. J Preg Child Health 4: 360. DOI: 10.4172/2376-127X.1000360
Copyright: ©2017 Rasul S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5678
- [From(publication date): 0-2017 - Aug 16, 2024]
- Breakdown by view type
- HTML page views: 4899
- PDF downloads: 779