Factors Associated with Timely Initiation of Complementary Feeding among Children Aged 6-23 Months in Ethiopia: A Multilevel Analysis of 2019 Ethiopian Mini Demographic Health Survey
Received: 22-Aug-2022 / Manuscript No. JPCH-22-72518 / Editor assigned: 25-Aug-2022 / PreQC No. JPCH-22-72518 (PQ) / Reviewed: 08-Sep-2022 / QC No. JPCH-22-72518 / Revised: 16-Jan-2023 / Manuscript No. JPCH-22-72518 (R) / Published Date: 24-Jan-2023
Abstract
Timely initiation of complementary feeding is providing the baby with solid or semisolid foods in addition to breast milk at 6-8 months of age. Due to many reasons, this feeding is extremely low in middle income and developing countries. In the current study, we aimed to identify factors contributing to the recent dataset of the Ethiopian demographic health survey. We used cross sectional EMDHS 2019 for this analysis. We cleaned the data and 4,061 women under under-two years of children were identified. We applied multilevel binary logistic regression in Stata v. 15. Model comparison was based on log-likelihood ratio, deviance and other criteria. Data were presented using mean, percent, 95% CI and Adjusted Odds Ratio (AOR). The timely complementary feeding was 36.44% (34.93-37.92%). Factors like preceding birth intervals (AOR=1.97 95% CI: 1.62-1.39), primary education (AOR=2.26 95% CI: 1.40-3.62), secondary above education (AOR=1.62 95% CI: 1.10-2.38) and rich wealth index (AOR=1.25 95% CI: 1.03-1.52) were some of the associated factors. It is highly suggested that comprehensive intervention on maternal education, empowering mothers economically, equity access to health services and birth planning should be targeted because they are attributable to maternal education, wealth index, preceding birth interval, number of under five children and regional disparities throughout the country
Keywords: Complementary feeding, Multilevel, Children, Ethiopia
Abbreviations
DHS: Ethiopian Demographic Health Survey; EMDHS: Ethiopian Mini Demographic Health Survey; WHO: World Health Organization; SNNPR: South Nations Nationalities and Peoples Region; CI: Confidence Interval; AOR: Adjusted Odds Ratio; LL: Log Likelyhood; AIC: Akaike Information Criterion; BIC: Baye’s Information Criterion; UNICEF: United Nation Children’s Fund; ICC: Intra Cluster Correlation
Introduction
According to the World Health Organization (WHO), exclusive breastfeeding is no more enough for the child’s growth and development at and after the age of six months. Thus, the child should be directed to breast milk plus additional (complementary) feeding to fill the nutrient gap, which is known for 45% of child deaths mostly in low and middle income countries [1,2]. Studies define timely complementary feeding as giving the baby additional food combined with the mothers’ breast milk within the 6-8 months after birth [3-5]. The United Nations Children’s Fund (UNICEF) informs that families have been challenged by economic, political, market, social or cultural barriers to feeding their children affordably and safely in every corner of the world. Additionally, inappropriate complementary feeding affects 149 million children around the globe [6]. The magnitude of the problem is relatively higher in Sub Saharan countries including Ethiopia.
In the South Asian countries, the untimely initiation of complementary feeding ranged from 17 to 76% in Bangladesh and 61% in Pakistan followed by 43.6% in Nepal [7]. In Sub Saharan countries, the proportion of untimely initiation of complementary feeding is 31.7% in 2019 [8]. Similarly, a systematic review of literature in the Sub-Saharan region showed 44.19% of mothers do not start complementary feeding as per WHO recommendation time [9]. One study in Nigeria revealed that 62.5% of the mothers started complementary feeding within 3-5 months [10].
In Ethiopia, a study in the Maichew district showed around 40% of mothers do not know the exact time of initiating complementary feeding [11].
A study in Addis Ababa showed that 17% of mothers started complementary feeding earlier than the normal time [12]. Another study in Dessie showed that 13.1% and 21.8% of mothers started giving complementary feeding earlier and late respectively [13]. In Northwest Ethiopia, 47.2% of mothers also practiced untimely complementary feeding and 37% in Northeast Ethiopia [14,15]. The new evidence from a systematic review in 2020 in the country showed that 34.4% of the mothers do not start complementary feeding at the recommended time [16].
There are various factors identified as predictors of untimely complementary feeding. In South Asia, lack of complementary feeding knowledge, low maternal education, socio-economic status and cultural beliefs were some factors that contributed to low timely complementary feeding; while, income, lack of knowledge and incorrect advice were the influencers from another study [17]. A study conducted in Nigeria showed that orthodox maternity care, exclusive breastfeeding and absence of siblings were associated with timely initiation of complementary feeding [18]. In Ethiopia, women employment, husband education, birth preparedness, growth monitoring, knowledge of time to introduce complementary feeding and paternal support were some of the factors that influence the time to initiate complementary feeding [19-21]. In another study, maternal educational status, complementary feeding counseling and maternal knowledge were identified as affecting factors.
Many national and international studies show that remarkable number of mothers do not adhere to the World Health Organization (WHO) complementary feeding recommendations; however, there is limited information on the larger population (country level samples) for policy and decision makers in Ethiopia. Thus, the current study had the aim of identifying factors enforcing mothers for untimely complementary feeding to provide the most recent representative information for further policy decisions from the recent country level data using multilevel logistic regression that accounts regional differences.
Materials and Methods
Study setting and data source
Ethiopia has conducted two EMDHS recently. In the 2019 EMDHS, the data collection was a community based cross sectional carried out from March 21, 2019 to June 28, 2019. All the nine regional states of the country (Afar, Tigray, Amhara, Oromia, Somali, Southern Nations, Nationalities and People’s Region (SNNPR), Benishangul Gumuz, Gambella and Harari) and two city administrations (Addis Ababa and Dire Dawa) were included in the study.
The EMDHS data was used as a secondary data source for this study. A stratified two staged cluster sampling was taken as data source. Randomly, the Enumeration Areas (EA) was selected in the first stage and then households were selected in the second stage. In all selected households, height, weight measurements and all nutritional data were collected from children 0-59 months and 4,061 women aged 15-49 were interviewed face to face using the woman’s questionnaire [22]. The detail of the recorded data is now available from the measure program web address. We extracted a 4,061 weighted number of children who are living with their mothers for this analysis.
Study variables
Outcome variable: The outcome for this study was timely initiation of complementary feeding. Complementary feeding termed to be timely when the feeding initiated between 6 and 8 months while complementary feeding commenced before 6 months or beyond 8 months was described as untimely.
Independent variables
The explanatory variables are the socio-demographic of the family, maternal services and nutritional factors (Table 1).
| S.No | Variable | Description | Code |
|---|---|---|---|
| 1 | *Region | The 11 regional location of the households included in the study | 1=Tigray, 2=Afar, 3=Amhara, 4=Oromia, 5=Somali, 6=Benishangul-Gumuz, 7=SNNP, 8=Gambela, 9= Harari, 10=Addis Ababa, 11=Dire Dawa |
| 2 | *Place of residence | Type of place of residence | 1=Urban, 2=Rural |
| 3 | Less than 5 yr children | No. of children <5 yr in household | 1=0-1 Child, 2=2 Children, 3= ≥3 Children |
| 4 | Mother’s Education | Mother’s level of education achieved | 0=No education, 1=Primary, 2=Secondary, 3=Higher and above |
| 5 | Place of delivery | Place of delivery | 0=Home, 1=Health Sector |
| 6 | Breastfeeding | Breast feeding status | 0=Not breastfed, 1=Exclusive, 2=Breastfed+plain water, 3=Breastfed+non-milk liquid, 4=Breastfed+ complementary food |
| 7 | Wealth index | Wealth index of household | 0=Poor, 1=Medium, 2=Rich |
| 8 | Gender | Gender of child | 1=Male, 2=Female |
| 9 | Birth order | Birth order of child | 1=First order, 2=2nd, 3=3rd or greater |
| 10 | Current age | Current age of mother | 0=15-24 years, 1=25-34 years, 2=35-49 years |
| 11 | Birth interval | Preceding birth interval (months) | 0= ≤ 24 months, 1=25-35 months, 2= ≥ 36 months |
| 12 | Household head | Head of house hold | 1=Male, 2=Female |
| 13 | Vitamin A | Child received vitamin A | 0=No, 1=Yes |
| 14 | Contraception | Current use by method | 0=Traditional, 1=Modern |
| Note: *Community level factors | |||
Table 1: Coding and description of explanatory variables.
Data processing and analysis
Frequencies, weighted frequencies, mean standard deviations and percentages or proportions were applied to describe timely initiation of complementary feeding. We also calculated the mean Variance Inflation Factor (VIF) that became 1.23 and in the acceptable range. Sampling weight was applied to manage the representativeness of the survey and to account for sampling design when calculating standard errors.
We used multilevel mixed effects logistic regression model to analyze the data because DHS data has some structures. The data as it is violates the independency of the observations and the equal variance assumption of the traditional logistic regression model. In the current model, we fitted four models to estimate both fixed and random effect of the individual and community level variables. We used the null model, a model without any independent variable, to check the presence of the between cluster variability. Secondly, we included all individual level factors in the model (Model I). Additionally, Model II was fitted with only community level variables. Finally, the combined model (Model III) was done with both the individual and community level variables to identify factors associated with timely initiation of complementary feeding (net fixed and random effects). Intra class correlation coefficient.
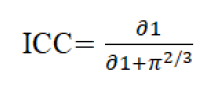
Where ∂1 is variance of null model and fixed number 3.29. Proportional change in variance.
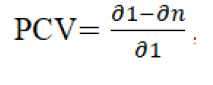
Where ∂1 null model variance and ∂n is variance of neighborhood in subsequent model; median odds ratio
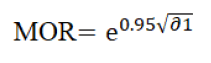
Where, ∂n is the variance of null model and deviance were used to compare models and identify best fitted model with AIC and BIC. We checked each variable for significance at p<0.20 and used p<0.05 for the final association indication. We cleaned the data as per the study criteria and analysed it in STATA v. 15.0 after weighting.
Results
We analyzed of 4,061 children’s initiation of complementary feeding time and found 36.44% (34.93%-37.92%), meaning more than 63% of families in Ethiopia initiate their children complementary feeding either earlier or later than the recommended 6-8 months. Participants from agrarian regions accounted for 87.81%. Nearly sixty percent (59.69%) of the mother were aged 25-34. Additionally, 50.10% of the mothers had 2 children under five years old, 61.98% of mothers were not learned, 48.85% of mothers were from poor wealth index families, 21.69% of preceding intervals were below 24 months and 58.32% of mothers gave birth at home (Table 2).
| Variable Regions | Unweighted (%) | Weighted (%) | Variable Age of mother | Unweighted (%) | Weighted (%) |
|---|---|---|---|---|---|
| Agrarian | 2,762 (66.22) | 3,566.53 (87.81) | 15-24 | 572 (13.71) | 570.20 (11.58) |
| Pastoralist | 992 (23.78) | 387.76 (9.55) | 25-34 | 2,514 (60.27) | 2,424.31 (59.69) |
| City administrations | 417 (10.00) | 107.12 (2.64) | ≥ 35 | 1,085 (26.01) | 1,166.90 (28.73) |
| Number of children <5 yr | Mother’s Education | ||||
| 1 | 1,276 (30.59) | 1,351.96 (33.29) | No education | 2,605 (62.46) | 2,517.12 (61.98) |
| 2 | 2,045 (49.03) | 2,034.90 (50.10) | Primary | 1,151 (27.60) | 1,233.25 (30.37) |
| ≥ 3 | 850 (20.38) | 674.55 (16.61) | Secondary and above | 415 (9.95) | 311.04 (7.66) |
| Birth interval | Wealth index | ||||
| ≤ 24 months | 966 (23.16) | 880.81 (21.69) | Poor | 2,282 (54.71) | 1,984.01 (48.85) |
| 25-35 months | 1,233 (29.56) | 1,135.64 (27.96) | Middle | 595 (14.27) | 760.37 (18.72) |
| ≥ 36 months | 1,972 (47.28) | 2,044.90 (50.35) | Rich | 1,294 (31.02) | 1,317 (32.43) |
| Breast feeding status | Place of delivery | ||||
| Not breastfed | 2,442 (58.55) | 2,264.93 (55.77) | Home | 2,329 (55.84) | 2,368.43 (58.32) |
| Exclusive breastfed | 840 (20.14) | 926.82 (22.82) | Health facility | 1,842 (44.16) | 1,692.98 (41.68) |
| Breastfed + other liquids | 98 (2.35) | 57.67 (1.42) | Child received vitamin A | ||
| Breastfed+complementary food | 791 (18.96) | 811.99 (19.99) | No | 1,358 (55.27) | 1,320.96 (55.82) |
| Yes | 1,099 (44.73) | 1,045.32 (44.18) | |||
Table 2: Factors associated with timely initiation of complementary feeding in Ethiopia, EMDHS 2019.
The analysis of factors associated with timely initiation of complementary feeding showed that variables like age of the mothers, maternal education, preceding birth interval, the number of children under five years old, gender of the household leader, wealth index were significant under the fixed effect model, while city administration the only random effect variable significant. Except for gender of the household leader, all those variables were also significant under the final model (mixed effect model. We interpreted variables from the last model here. Accordingly, mothers with age range of the 25-34 and the age ≥ 35 years had 40% and 53% reduced odds of starting their children complementary feeding at the recommended time with AOR of 0.60 (0.49-0.74 and 0.47 (0.37-0.60 respectively relative age 15-24 years. Conversely, mothers who reported preceding birth intervals greater than 36 months had 1.97 times more like to start complementary feeding timely with AOR of 1.97 (1.62-1.39) compared to less than 24 months. In contrast to this fact mothers who had 2 and more three under five children during the survey had higher odds of starting complementary feeding timely with AOR of 3.63 (3.03-4.36) and 4.12 (3.25-5.21) respectively. Maternal education of either primary or secondary and above is associated with higher odds of timely initiation of complementary feeding with AOR of 2.26 (1.40-3.62) and 1.62 (1.10-2.38) respectively. Respondents from the rich family wealth index had high odds of reporting timely complementary feeding with AOR of 1.25 (1.03-1.52). At community level, respondents from pastoralist regions had 33% reduced odds of starting complementary feeding on time with AOR of 0.77 (0.61-0.98); while, those from city administrations had higher odds of reporting timely complementary feeding with AOR of 1.47 (1.11-1.96) (Table 3).
| Variables | Model 0 | Model I | Model II | Model III |
|---|---|---|---|---|
| Age in 5 years group | ||||
| 15-24 | - | 1 | - | 1 |
| 25-34 | - | 0.62 (0.51-0.76)*** | - | 0.60 (0.49-0.74) *** |
| ≥ 35 | - | 0.49 (0.38-0.62)*** | - | 0.47 (0.37-0.60) *** |
| Education | ||||
| No education | - | 1 | - | 1 |
| Primary education | - | 2.39 (1.49-3.82)*** | - | 2.26 (1.40-3.62)*** |
| Secondary education and above | - | 1.78 (1.22-2.60)** | - | 1.62 (1.10-2.38)** |
| Preceding birth interval | ||||
| <24 months | 1 | - | ||
| 24-36 months | 1.04 (0.86-1.25) | 1.03 (0.85-1.24) | ||
| >36 months | 2.00 (1.65-2.43)*** | 1.97 (1.62-1.39)*** | ||
| Number of children <5 yr | ||||
| 1 | 1 | |||
| 2 | 3.63 (0.03-4.35)*** | 3.63 (3.03-4.36)*** | ||
| ≥ 3 | 3.99 (3.16-5.04)*** | 4.12 (3.25-5.21)*** | ||
| Gender of household leader | ||||
| Male | - | 1 | ||
| Female | - | 1.17 (1.02-1.47)* | 1.10 (1.07-1.68) | |
| Wealth index | ||||
| Poor | 1 | |||
| Middle | 1.02 (0.81-1.25) | 0.99 (0.79-1.23) | ||
| Rich | 1.25 (1.08-1.67)** | 1.25 (1.03-1.52)* | ||
| Region | ||||
| Agrarian | - | 1 | 1 | |
| Pastoralist | 0.91 (0.73-1.12) | 0.77 (0.61-0.98)* | ||
| City administrations | 1.52 (1.13-2.04)** | 1.47 (1.11-1.96)** | ||
| Note: *=indicates a significant difference of AOR. | ||||
Table 3: Multilevel analysis of timely initiation of complementary feeding among aged 6-23 months in Ethiopia, 2019 EMDHS.
Although the data is not highly affected by clusters as results from Table 4 shown, the model fitting with balancing the existing hierarchies is very good. The decreased ICC, AIC, BIC, the increased log likelihood ratio showed how model improved over the process. The 2% ICC can be only raid off by including further random effect variables table.
| Random effect model comparison | Model 0 | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|
| Community level Variance | 0.25 | 0.15 | 0.10 | 0.08 |
| Inter Cluster Correlation (ICC) | 0.066 | 0.04 | 0.03 | 0.02 |
| Log Likelihood Ratio (LLR) | -2729 | -2572 | -2722 | -2566 |
| Proportional Change in Variance (PCV) | Ref | 0.4 | 0.6 | 0.68 |
| Media Odds Ratio (MOR) | 1.60 | |||
| AIC | 5463 | 5171 | 5455 | 5163 |
| BIC | 5476 | 5254 | 5487 | 5258 |
Table 4: Model comparison and random effect distribution of timely initiation of complementary feeding among children of 6-23 months age in Ethiopia, 2019 EMDHS.
Discussion
From our analysis, only 36.44% (95% CI: 34.93%-37.92%) children were started their complementary feeding within the WHO recommended time, that means nearly 64% of the children began complementary feeding either before six months or later than eight months. The 64% untimely complementary feeding magnitude is less than 76% in Bangladesh, but consistent with the 61% in Pakistan and 62.5% in Nigeria. It is greater than 43.6% in Nepal, 44.19% in Sub Saharan region, 47.2% in Northwest Ethiopia, 37% in Northeast Ethiopia and 34.4% pooled prevalence in Ethiopia. This means, the finding is greater than the South Asian, regional and the country level average untimely proportions. The reason might be due to the overall decreasing timely complementary feeding and increased number of mothers using formula milk feeding which need serious considerations. Additionally, 50.10% of the mothers had two children aged below five years. One study showed that most mothers are young and had ≥ 7 children [23]. It is not a secret that 27.96% birth interval is around 35 months which mean, mother have plenty of time to have another baby before the fifth birthday of the preceding child when modern contraceptive proportion is also low. In other words, 61.98%of the mother had no education. This is supported by 62.8% of poor education in Nigeria and 54.0% in North Ethiopia but different from 30% in Northwest Ethiopia. The consistency might indicate the poor achievement in education both regionally and at country level bearing in mind that there are also areas in the country where maternal education is good. In addition to this, 48.85% of mothers were from poor wealth index families the evidence which is supported by many studies. Overall, from evidence, the economic status of people in the country is not good enough but supporting mother economically and in educational matters could worth a lot. The 58.32% of home deliveries might also need the same intervention as evidences directed toward the poor achievements in the country.
During multilevel modeling, the mixed effect model appeared with age of the mothers, maternal education, preceding birth interval, the number of children under five years old per woman and wealth index the fixed effect factors, while pastoralists and city administrations the random effect factors were significant. The age of the mothers that is greater than 24 years was inversely associated with timely initiation of complementary feeding in Ethiopia. One study also agreed that mothers of these ages usually begin complementary feeding very early, where another study stated age less than 20 year is associated with timely complementary feeding compared to the higher groups. As the age increase number of children increase and the focus of the mothers might be falling away. As global expectations, maternal education whether it is primary or higher, had independently predicted timely initiation of complementary feeding. This is also supported by the huge evidence from the literature. This means, maternal education is another independent predictor of timely initiation of complementary feeding that is why supporting mothers in education might worth much. As preceding birth interval increase above 36 months, the probability of mothers sticking to the recommended time of initiating complementary feeding increased. This is also supported by some studies in the country. It might mean, child spacing is something to focus on. However, it might also mean that, those mothers were educated, use family planning, economically enough and taking up service. Mothers with rich wealth index had good timely initiation of complementary feeding, the impression which is also supported by other studies. The consistency might be due the fact that mothers of lower economic level might struggle to find something to feed their baby. Mothers from pastoralists regions do not practice timely complementary feeding; while, mother from city administrations did well. The regional difference regarding complementary feeding is also immense form another study. The difference might be due to differences in equity distribution of health services, access and availability related matters. Despite the very important finding of this study, there were also some limitations that need to be considered. Disproportion of sampling, high missing in the data, secondary nature of the data and others were some of the problems which authors approached through weighting, reducing sample by missing and considering the time of data collection in the discussion were involved.
Conclusion
According our analysis, the timely initiation of complementary feeding in Ethiopia was very low. Mothers started complementary feeding either earlier or later than the recommended time. Factors like age of the mothers, maternal education, preceding birth interval, the number of children under five years old and wealth index, pastoralists and city administrations were found to be affected the achievements. It is highly suggested that comprehensive intervention on maternal education, empowering mothers economically, equity access to health services and birth planning should be targeted to get more dividend. Especial policy attention should go to the pastoralists regions where those problems were enormous.
Authors’ Contribution
GG has involved in conception, design, interpretation, writing methods and analysis; while, SS, TD and KG were involved in validation, drafting the manuscript and reviewing the manuscript.
Acknowledgements
The authors are grateful to measure DHS, ICF International Rockville, Maryland, USA for allowing us to use the 2016 EDHS data.
References
- World Health Organization (2000) Complementary feeding: Family foods for breastfed children. Department Nutrition Health Development.
- Manikam L, Sharmila A, Dharmaratnam A, Alexander EC, Kuah JY, et al. (2018) Systematic review of infant and young child complementary feeding practices in South Asian families: The Pakistan perspective. Public Health Nutr 21: 655-668.
[Crossref] [Google Scholar] [PubMed]
- Manikam L, Robinson A, Kuah JY, Vaidya HJ, Alexander EC, et al. (2017) A systematic review of complementary feeding practices in South Asian infants and young children: The Bangladesh perspective. BMC Nutr 3: 1-13.
[Crossref] [Google Scholar] [PubMed]
- Yeheyis T, Berhanie E, Yihun M, Workineh Y (2016) Timely initiation of complementary feeding and associated factors among children aged 6 to 12 months in Addis Ababa Ethiopia, 2015. Epidemiol Open Access 6: 4-12.
- Acharya D, Subedi R, Lee K, Yoo SJ, Gautam S, et al. (2018) Correlates of the timely initiation of complementary feeding among children aged 6-23 months in rupandehi district, Nepal. Children 5: 1-9.
[Crossref] [Google Scholar] [PubMed]
- Gebremedhin S (2019) Core and optional infant and young child feeding indicators in Sub Saharan Africa: A cross-sectional study. BMJ Open 9: e023238
[Crossref] [Google Scholar] [PubMed]
- Appiah F, Ahinkorah BO, Budu E, Oduro JK, Sambah F, et al. (2021) Maternal and child factors associated with timely initiation of breastfeeding in Sub Saharan Africa. Int Breastfeed J 16: 1-11.
[Crossref] [Google Scholar] [PubMed]
- Esan DT, Eniola O, Iwari A, Hussaini A, Adetunji AJ (2022) Complementary feeding pattern and its determinants among mothers in selected primary health centers in the urban metropolis of Ekiti State, Nigeria. Sci Rep 12: 1-9.
[Crossref] [Google Scholar] [PubMed]
- Reda EB, Teferra AS, Gebregziabher MG (2019) Time to initiate complementary feeding and associated factors among mothers with children aged 6-24 months in Tahtay Maichew district, northern Ethiopia. BMC Res Notes 12: 1-8.
[Crossref] [Google Scholar] [PubMed]
- Mohammed S, Getinet T, Solomon S, Jones AD (2018) Prevalence of initiation of complementary feeding at 6 months of age and associated factors among mothers of children aged 6-24 months in Addis Ababa, Ethiopia. BMC Nutr 4: 1-7.
[Crossref] [Google Scholar] [PubMed]
- Andualem A, Edmealem A, Tegegne B, Tilahun L, Damtie Y (2020) Timely initiation of complementary feeding and associated factors among mothers of children aged 6-24 months in Dessie Referral Hospital, Northeast Ethiopia, 2019. J Nutr Metab 2020.
[Crossref] [Google Scholar] [PubMed]
- Biks GA, Tariku A, Wassie MM, Derso T (2018) Mother’s Infant and Young Child Feeding (IYCF) knowledge improved timely initiation of complementary feeding of children aged 6-24 months in the rural population of northwest Ethiopia. BMC Res Notes 11: 1-7.
[Crossref] [Google Scholar] [PubMed]
- Sisay W, Edris M, Tariku A (2016) Determinants of timely initiation of complementary feeding among mothers with children aged 6-23 months in Lalibela District, Northeast Ethiopia, 2015. BMC Public Health 16: 1-9.
[Crossref] [Google Scholar] [PubMed]
- Habtewold TD, Mohammed SH, Tegegne BS (2020) Breast and complementary feeding in Ethiopia: new national evidence from systematic review and meta-analyses of studies in the past 10 years: reply. Eur J Nutr 59: 841-842.
[Crossref] [Google Scholar] [PubMed]
- Manikam L, Lingam R, Lever I, Alexander EC, Amadi C, et al. (2018) Complementary feeding practices for south asian young children living in high income countries: A systematic review. Nutrients 10: 1-22.
- Ogunlesi TA, Ayeni VA, Adekanmbi AF, Fetuga BM (2014) Determinants of timely initiation of complementary feeding among children aged 6-24 months in Sagamu, Nigeria. Niger J Clin Pract 17: 785-790.
[Crossref] [Google Scholar] [PubMed]
- Alemayehu Y, Ermeko T, Hussen A, Lette A, Abdulkadir A (2021) Timely initiation of complementary feeding practice among mothers and care givers of children age 6 to 24 months in Goba Town, Southeast Ethiopia. J Women’s Heal Care 10: 1-7.
[Crossref]
- Shumey A, Demissie M, Berhane Y (2013) Timely initiation of complementary feeding and associated factors among children aged 6 to 12 months in Northern Ethiopia: An institution based cross sectional study. BMC Public Health 13.
[Crossref] [Google Scholar] [PubMed]
- Agedew E, Demissie M (2014) Early initiation of complementary feeding and associated factors among 6 months to 2 years young children, in Kamba Woreda, South West Ethiopia: A community based cross-sectional study. J Nutr Food Sci :04.
- Kassa T, Meshesha B, Haji Y, Ebrahim J (2016) Appropriate complementary feeding practices and associated factors among mothers of children age 6-23 months in Southern Ethiopia, 2015. BMC Pediatr 16:1-10.
[Crossref] [Google Scholar] [PubMed]
- Semahegn A, Tesfaye G, Bogale A (2014) Complementary feeding practice of mothers and associated factors in Hiwot Fana specialized hospital, eastern Ethiopia. Pan Afr Med J 18: 1-11.
[Crossref] [Google Scholar] [PubMed]
- Gudeta AN, Andren Aronsson C, Balcha TT, Agardh D (2021) Complementary feeding habits in children under the age of 2 years living in the city of adama in the oromia region in central Ethiopia: traditional Ethiopian food study. Front Nutr 8: 1-7.
[Crossref] [Google Scholar] [PubMed]
- Shagaro SS, Mulugeta BT, Kale TD (2021) Complementary feeding practices and associated factors among mothers of children aged 6-23 months in Ethiopia: Secondary data analysis of Ethiopian mini demographic and health survey 2019. Arch Public Heal 79: 1-12.
[Crossref] [Google Scholar] [PubMed]
Citation: Gilano G, Sako S, Dileba T, Gilano K (2023) Factors Associated with Timely Initiation of Complementary Feeding among Children Aged 6-23 Months in Ethiopia: A Multilevel Analysis of 2019 Ethiopian Mini Demographic Health Survey. J Preg Child Health 10:579.
Copyright: © 2023 Gilano G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2347
- [From(publication date): 0-2023 - Dec 05, 2025]
- Breakdown by view type
- HTML page views: 1947
- PDF downloads: 400
