Factors Associated with Confirmed Tuberculosis Treatment Outcome: A Hospital Study Cohort in Dakar, Senegal
Received: 17-Sep-2019 / Accepted Date: 26-Sep-2019 / Published Date: 03-Oct-2019 DOI: 10.4172/2332-0877.1000409
Abstract
Context: In order to break the chain of tuberculosis transmission, all diagnosed cases must be followed until the treatment is complete. Several factors influence the treatment outcomes, particularly in hospitals where care is provided for patients with the most severe cases.
Methodology: The purpose of this retrospective cohort study was to analyze the evolution of the treatment outcomes from 2011 to 2015 and identify factors associated with unsuccessful TB treatment. Tuberculosis cases confirmed by bacteriology and/or by Xpert-MTB/Rif test, being treated in the Department of Infectious and Tropical Diseases at Fann University Hospital in Dakar, were included. The trend Ch2 test was used to measure the evolution of treatment outcomes from 2011 to 2015 and logistic regression for the identification of the factors associated with unsuccessful TB treatment.
Results: We collected 413 confirmed tuberculosis cases. The average age of patients was 38 ± 12 years and the sex ratio: 1.3. Most patients of the 46.4% cases were admitted to hospital. The average weight during the beginning of the treatment was 51 ± 10.8 kg. The isolated pulmonary TB represented 86.2%, followed by the multifocal TB 11.8%. Patients receiving retreatment were 8.2%. The HIV seroprevalence was 60.67%. Bacilloscopy confirmed tuberculosis in 75% of the cases and the Xpert-MTB/Rif test in 25%. From 2011 to 2015, the percentage of patients with successful TB treatment has increased from 47.4% to 69.3% (p=0.006). Lost to follow up patients have decreased from 18.4% to 7.4% (p=0.04). Unsuccessful TB treatment was associated to hospitalization at TB diagnosis (AOR=7.15; 95% CI: 4.23 – 12.10), low weight when starting the treatment (AOR=0.33; 95%CI: 0.14 – 0.77), and co-infection with HIV (AOR=2.07; 95% CI: 1.17 – 3.71).
Conclusion: Overall, progress has been made in monitoring patients who have been treated for tuberculosis. However, the favorable outcome percentage could be increased by improving the nutritional condition of patients and intensifying early screening and fighting against HIV infection.
Keywords: Tuberculosis; Confirmed; Treatment; Outcome
Keywords
Tuberculosis; Confirmed; Treatment; Outcome
Introduction
Tuberculosis is one of the causes of death in the world. The Global Plan to end tuberculosis on the period of 2016-2020 is to reach 90% of individuals who need TB treatment, and to achieve at least 90% treatment success [1]. These targets are particularly important for the smear-positive pulmonary tuberculosis cases which are contagious and are responsible for the dissemination of the disease. The diagnosis of these forms improved during these past years with liquid cultures, new LED fluorescent microscopy and the advent of Gen-Xpert/MTB which helps identify Mycobacterium tuberculosis and test susceptibility to rifampicine [2,3].
In Senegal, the incidence of tuberculosis estimated by WHO is 139 cases per 100, 000 habitants. Among the 13, 660 cases detected in the population in 2017, 88% were bacteriological Pulmonary tuberculosis [4]. The Screening, the application of directly observed treatment and the follow-up care of the diagnosed cases are provided at the operational level by the 80 tuberculosis treatment centers (CDT), including Fann’s department of infectious and tropical diseases (SMIT) of the national university hospital center (CHNU). Unlike the cases on care in health centers, the clinical presentations are more severe in hospitals. The purpose of this study was to analyze the evolution of treatment outcomes of confirmed tuberculosis cases from 2011 to 2015 and identify factors associated with unsuccessful TB treatment at a university hospital of Dakar in Senegal [5].
Methodology
Setting
We conducted this study in the Department of Infectious Diseases at Fann University Hospital in Dakar (Senegal). It has a Screening and Treatment Centre of TB since 1988. All diagnosed patients are registered and monitored for treatment outcomes according to the recommendations of the National Tuberculosis Control Program (NTP). The treatment is directly observed for the hospitalized patients and then after the follow-up care will be done on an outpatient basis after discharge from the hospital. The dispensing of anti-tuberculosis drug is provided by a state-certified nurse, under the supervision of a doctor in charge
Study design and population study
Our hospital-based retrospective cohort study included all the bacteriologically confirmed (by microscopy or Xpert MTB/RIF assay or both) tuberculosis cases treated from 2011 to 2015.
Case definitions: A case is defined According to previous TB treatment received by the patient. TB cases were classified as a new case (A patient who has never had treatment for TB or who has taken anti-tuberculosis drugs for less than 1 month) or a retreatment cases (relapse cases, Treatment after failure, Treatment after default).
Treatment regimen: In Senegal, irrespective of TB localization, we used the five anti-tuberculosis first line drugs and the regimen depend on case definition. For the new cases, weadministrated 2 months (Intensive phase) of rifampicin-isoniazid-pyrazinamide-ethambutol, followed by 4 months (Continuation phase) of rifampicin-isoniazid (2RHZE/4RH). Retreatment cases received for 2 months (intensive phase) rifampicin-isoniazid-pyrazinamide-ethambutol-streptomycin, followed by 6 months (Continuation phase) of rifampicin-isoniazidpyrazinamide- ethambutol (2 RHZES/6RHZE).
TB treatment outcomes
Cured: A pulmonary TB patient with bacteriologically confirmed TB at the beginning of treatment who was smear or culture negative in the last month of treatment and on at least one previous occasion.
Completed treatment: A TB patient who completed treatment without evidence of failure but with no record to show that sputum smear or culture results in the last month of treatment and on at least one previous occasion were negative, either because tests were not done or because results are unavailable.
Failure: A TB patient whose sputum smear or culture is positive at month 5 or later during treatment.
Died:A TB patient who dies for any reason during the treatment
Lost to follow-up: A TB patient whose treatment was interrupted for 2 consecutive months or more.
Transferred out:This includes cases “transferred out” to another treatment unit as well as cases for whom the treatment outcome is unknown to the reporting unit
Data Collection
Socio-demographic data (age, gender, residential district), clinical aspects (date of TB diagnosis, hospitalization or outpatient, weight at treatment initiation, form of TB (pulmonary TB, Extra-pulmonary TB and multifocal TB), type of TB confirmation (microscopy or Xpert MTB/RIF assay or both), HIV status (positive, negative or Unknown), treatment regimen (new cases/retreatment cases) and TB treatment outcomes were collected. Medical records, TB and hospital registers, NTP treatment cards were used to document the collected data.
Statistical Analysis
Data was analyzed using Epi-info 3.7.1 software and SAS Software version 9.3, Cary, NC, USA. Frequencies, means, standard deviations, were used to describe the population study. To identify factors associated with TB treatment outcome, we classified the patients in two groups. “Successful TB treatment” included cured or completed treatment and “Unsuccessful TB treatment” included treatment failure, lost to follow up, died or transferred out to another health facility. Firstly, we conducted univariate analysis. Association of unsuccessful treatment, epidemiological, clinical and biological features was identified using chi2 test (categorical variables) and Student test (Continuous variables). The logistic regression was used for multivariable analysis. Independent variables from the univariate analyses were entered into the multivariable model if significant at p<0.20 level. Odds ratios (OR) were reported with a 95% Confidence Interval. A p value<0.05 was considered statistically significant in multivariable analysis.
Ethical Considerations
The Head of the Department of Infectious Diseases approved this retrospective study. All data collected were anonymized prior to analysis.
Results
Characteristics study population
We included 413 confirmed tuberculosis cases of which 91.8% new cases. The average age was 38 ± 12 years and the sex ratio 1.3. More than three-quarters of the patients (70.2%) came from the urban and suburban districts of Dakar region (Centre, North, South, Pikine) (Tables 1 and 2).
| Variables | Number | Percent |
|---|---|---|
| Year of TB diagnosis | ||
| 2011 | 76 | 18,4 |
| 2012 | 70 | 17,0 |
| 2013 | 79 | 19,1 |
| 2014 | 93 | 22,5 |
| 2015 | 95 | 23,0 |
| Sex | ||
| Male | 235 | 57,0 |
| Female | 178 | 43,0 |
| Age group (years) | ||
| 15-44 | 292 | 70,7 |
| 45-60 | 93 | 22,5 |
| >60 | 28 | 6,8 |
| District residence | ||
| Urban districts/Dakar region | 264 | 64,2 |
| Sub-urban districts Dakar region | 132 | 32,1 |
| Others regions | 15 | 3,7 |
| Hospitalization | ||
| Yes | 191 | 46,2 |
| No | 222 | 53,8 |
| Weight at TB diagnosis (Kg) | ||
| 25-39 | 47 | 11,5 |
| 40-54 | 213 | 52,0 |
| 55-70 | 133 | 32,4 |
| >71 | 17 | 4,1 |
| Clinical presentation | ||
| Pulmonary only | 356 | 86,2 |
| Multifocal | 49 | 11,8 |
| Extra-pulmonary only | 8 | 2,0 |
| Treatment category | ||
| New cases | 382 | 91,8 |
| Retreatment cases | 31 | 9,2 |
| Confirmation of TB | ||
| Microscopy | 310 | 75,1 |
| Xpert MTB/RIF assay | 100 | 24,2 |
| Both | 3 | 0,7 |
| HIV status | ||
| Positive | 199 | 48,2 |
| Negative | 129 | 31,2 |
| Unknown | 85 | 8,5 |
| Outcome TB treatment | ||
| Cured | 187 | 45,3 |
| Completed treatment | 48 | 11,6 |
| Died | 72 | 17,4 |
| Transferred out | 57 | 13,9 |
| Lost to follow up | 48 | 11,6 |
| Treatment failure | 1 | 0,2 |
Table 1: Socio-demographic, clinical, and outcome description of study population.
| Variables | Number | Events*(n, %) | Crude OR (CI95%) | Ajusted OR (IC95%)** |
|---|---|---|---|---|
| Year of TB diagnosis | ||||
| 2011 | 76 | 40 (52,6) | 1 | 1 |
| 2012 | 70 | 30 (42,8) | 0,67 (0,35 – 1,29) | 0,74 (0,34 – 1,64) |
| 2013 | 79 | 43 (54,4) | 1,07 (0,57 – 2,02) | 0,74 (0,33 – 1,63) |
| 2014 | 93 | 36 (38,7) | 0,59 (0,31 – 1,05) | 0,38 (0,17 – 0,83) |
| 2015 | 95 | 29 (30,5) | 0,39 (0,21 – 0,74) | 0,20 (0,08 – 0,46) |
| Sex | ||||
| Male | 235 | 98 (41,7) | 1 | |
| Female | 178 | 80 (44,9) | 1,14 (0,77 – 1,69) | |
| Age group (years) | ||||
| 15 – 44 | 292 | 115 (39,4) | 1 | 1 |
| 45 – 60 | 93 | 50 (53,8) | 1,79 (1,18 – 2,86) | 1,43 (0,80 – 2,56) |
| >60 | 28 | 13 (46,4) | 1,33 (0,61 – 2,91) | 1,51 (0,57 – 3,97) |
| District residence | ||||
| Urbain districts/Dakar | 265 | 95 (36,0) | 1 | 1 |
| Sub-urbain districts/Dakar | 132 | 70 (53,0) | 2,00 (1,31-3,07) | 1,40 (0,82 – 2,39) |
| Other sregions | 125 | 12 (80,0) | 7,11 (1,96-25,84) | 4,29(0,92 – 19,98) |
| Hospitalization at TB diagnosis | ||||
| Outpatient | 221 | 47 (21,2) | 1 | 1 |
| Inpatient | 191 | 131 (68,5) | 8,08 (5,18 -12,60) | 7,18(4,25 – 12,13) |
| Weight at TB diagnosis (Kg) | ||||
| 25 – 39 | 47 | 28 (59,6) | 1 | 1 |
| 40 – 54 | 213 | 103 (48,4) | 0,63 (0,33-1,21) | 0,53 (0,24 – 1,16) |
| 55 – 70 | 133 | 41 (30,8) | 0,30 (0,15-0,60) | 0,34 (0,15 – 0,80) |
| >71 | 17 | 4(23,5) | 0,21 (0,06-0,74) | 0,26 (0,06 – 1,13) |
| Clinical presentation | ||||
| Pumonary only | 356 | 144 (40,4) | 1 | 1 |
| Extra-pulmonary only | 8 | 4 (50,0) | 1,47 (0,36-5,98) | 1,98(0,37 – 10,53) |
| Multifocal | 49 | 30 (61,2) | 2,32 (1,26-4,29) | 0,88 (0,41 – 1,83) |
| HIV statut | ||||
| Negative | 129 | 40(31,0) | 1 | 1 |
| Positive | 199 | 104(52,3) | 2,43 (1,53-3,89) | 2,01(1,17 – 3,60) |
| Unknow | 85 | 34(40,0) | 1,48 (0,83-2,63) | 1,34 (0,66 – 2,75) |
| Treatment category | ||||
| New cases | 382 | 158 (41,3) | 1 | 1 |
| Retreatment cases | 31 | 20(64,5) | 2,58 (1,20-5,53) | 1,51(0,61 – 3,77) |
Table 2: Factors associated with unsuccessful TB treatment outcome (n=413).
Among the 413 cases, 191 (46.4%) were hospitalized during the TB diagnosis. The average weight during the beginning of the antituberculosis treatment was of 51 kg ± 10.8 kg. The isolated pulmonary tuberculosis was the most frequent (86.2%), followed by the multifocal tuberculosis (11.8%). The lymph node (7.4%) and neuro-meningeal (5%) localizations were the predominant extra-pulmonary forms.
313 cases of TB were confirmed by microscopy and Gen-Xpert test was positive in 100 patients. No Rifampicin resistant was detected. Gen-xpert was predominantly positive for pulmonary specimens (96 cases), the cerebrospinal fluid (LCR) (10 cases; 9.7%) and the lymph node puncture fluid (8 cases; 7.7%). The HIV seroprevalence was 48.2%. The cotrimoxazole prescription rate among the TB/HIV coinfected patients was 88.9% and almost one third was on antiretroviral treatment (30.7%) during hospitalization.
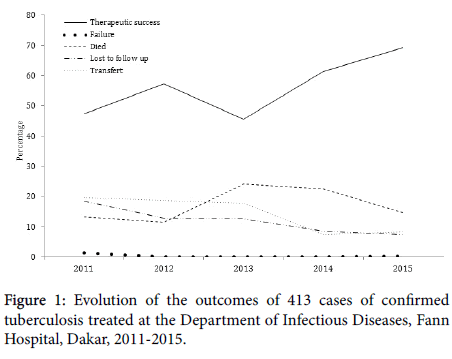
Tuberculosis treatment outcomes (Figure 1)
In our study, 235 cases (56.9%) had a successful TB response (cured or completed treatment). From 2011 to 2015, the percentage of patients increased significantly from 47.4% to 69.3% (p=0.006). The lethality was 17.4% and 11.6% of cases lost to follow up during TB treatment. In addition, the rate of patients lost to follow-up decreased progressively over the last 4 years from 18.4% to 7.4%, a drop of 61% (p=0.04). However, lethality did not progress (p=0.33).
Factors associated with unsuccessful TB treatment (Table 2)
By univariate analysis, the unsuccessful TB treatment was lower in 2015 in comparison with 2011 (crude OR=0.39; 95%CI: 0.21-0.74). Whereas, the treatment failure risk was increasing along with the age (45 – 60 years versus 15-44 years) (crude OR=1.79; 95%CI: 1.18 – 2.86). It was higher among patients residing in suburban area (crude OR=2.00; 95%CI: 1.31-3.07), and outside Dakar (crude OR=7.11; 95% CI: 1.96-25.84). The risk of unsuccessful TB treatment was decreasing when the weight was increasing during the beginning of TB treatment. By univariate analysis, the other factors associated with unsuccessful TB treatment were hospitalization during tuberculosis diagnosis (crude OR=8.08; 95%CI: 5,18-12.60), HIV infection (crude OR=2.43; 95%CI: 1.53-3.89), presence of a multifocal TB (crude OR=2.32; 95%CI: 1.26-4.29) and the previous TB treatment (crude OR=2.58; 95%IC: 1.20-5.53).
By multivariate analysis, the unsuccessful TB treatment was higher in 2011 in comparison with the years of 2014 (adjusted OR=0.38; 95%CI: 0.17-0.83), and 2015 (adjusted OR=0.20; 95%CI: 0.08-0.46), among the hospitalized patients at TB diagnosis (adjusted OR=7.18; 95%CI: 4.25 – 12.13) and in case of HIV infection (adjusted OR=2.01; 95%CI: 1.17-3.60). Moreover, the treatment failure risk was lower among patients with a weight of 55-70 kg during the beginning of the treatment in comparison with those with a weight between 25-39 kg (adjusted OR=0.34; 95%CI: 0.15-0.80).
Discussion
This study done at the hospital level in a Dakar environment confirms once again the importance of Gen-xpert in the tuberculosis diagnosis. About a quarter of the cases (24.9%) has been confirmed by means of its application. It was mainly positive among the pulmonary tests (93.2%). These data comply with the literature data. Steingart KR found again a sensibility (Se) of 89% [85%-92%] and a specificity of 99% [95%-99%] of Gen-Xpert for the pulmonary tuberculosis diagnosis with a difference according to the microscopy results (Se: 89% [85% – 92%] Microscopy (+) and Se: 67% [60% – 74%] Microscopy (-) [6]. However, the sensibility of Gen-Xpert is variable at the extra-pulmonary localizations: 50.9% in pleural fluid, 71.1% in the cerebrospinal fluid and 82.7% in the urine [7]. In our cases, it is mainly positive in the cerebrospinal fluid (9.7%) and the lymph node fluid (7.7%).
Concerning the outcome of patients, even if we have noticed a significant increase percentage of patients with successful TB treatment from 2011 to 2015 (47.4% to 69.3%, p=0.006), that rate remains low. These results are mainly related to the high prevalence of HIV infection (48.2%) and the high percentage of hospitalized patients (46.4%) in our cohort. The unsuccessful TB treatment was associated to hospitalization at TB diagnosis (AOR=7.15; 95%CI: 4.23 – 12.10) and co-infection with HIV (AOR=2.07; 95%CI: 1.17 – 3.71). These results are similar to those of Amante TD in Ethiopia (OR=2.5; 95%CI: 1.34 – 5.7) [8]. Excess mortality of co-infected patients has been clearly demonstrated. Most of the studies agree on the negative impact of HIV upon successful TB treatment among the tuberculosis patients [9,10] in relation to immuno-suppression presentation, the presence of other opportunistic infections and the complexity of the co-administration of anti-tuberculosis and antiretroviral treatment. Only one third of our patients were on antiretroviral treatment, this is due to the fact that some of them died, disappeared or were transferred out before being on treatment. In some cases, the application of antiretroviral therapy has not been notified to the nurse in charge of the treatment.
In our series, the proportion of lost to follow-up patients was high (11.6%). Comparable data were reported from Morocco by Hassani (10.3%) [11,12] and Diallo from Mali (17.4%) [13]. Previous history of tuberculosis, occurrence of side effects, family problems, and stigmatization has been reported as causes of treatment interruption. Continuous decline of the lost to follow-up patients rate (18.4% to 7.4%, p=0.04) noticed in our study due to the work of the social services department must be maintained. The National Tuberculosis Control Program is recommending that a patient should be sent to the health facilities close to the patient residence in order to lower the transport cost that may help to decrease the rate of the lost to followup patients.
By multivariate analysis, the unsuccessful TB treatment was more important in 2011 in comparison with the years of 2014 (AOR=0.38; 95%CI: 0.17 – 0.83) and 2015 (AOR=0.21; 95%CI: 0.09 – 0.49). This is comparable to the results of Fahrettin T [10] who had noticed a successful TB treatment increase from 73.8% between 1999 and 2002 to 83.6% between 2002-2004. In a study conducted in South Africa, the same trend was found again with a drop of 1.7% of treatment failures between 2003 and 2012 [14]. This is evidence of the efforts made during these last few years in the eradication of tuberculosis with the application of DOTS.
Indeed, this strategy aims to strengthen adherence to antituberculosis treatment. If it is effectively applied, it will help to prevent the occurrence of new multidrug-resistant cases.
The relation between successful TB treatment and gender has not been noticed. But, some studies had pointed out that correlation [15]. In Africa, it is recognized that women have more access to health care services but nevertheless their active lives can have a negative impact on the treatment adherence.
Contrary to the findings of Kigozi, South Africa Gen who had noticed a low failure rate in older patients (p<0.001) [14], difference in terms of age has not been found in your study.
A positive association has been found between unsuccessful TB treatment and low weight at the beginning of the anti-tuberculosis treatment (AOR=0.33; 95%CI: 0.14 – 0.77). Likewise, Lackey [16] had found that the rate of successful TB treatment was more frequent in patients with body mass index>18.5 kg/m2 (OR 2.08; 95%CI: 1.21-3.56). Many researches have shown that malnutrition is a factor of poor prognostic [17,18]. During HIV infection, malnutrition is mostly the secondary opportunistic cause of digestive infections such as the oropharyngeal candidiasis, the infectious diarrhea.
By multivariate analysis, there was not a correlation between successful TB treatment and treatment regime. On the other hand, researchers have reported that patients on treatment were more in treatment failure risk [19,20] and that might be related to the emergence of strains resistant to the treatment.
Conclusion
Although there is a significant increase in the rate of successful TB treatment for confirmed tuberculosis patients, improved is still needed to achieve the 90% successful treatment rate. The recommendation actions are early application of the antiretroviral therapy and the improvement of patient’s nutritional condition since the main two factors that influence the treatment and make the treatment unsuccessful are HIV infection and low weight during the beginning of the treatment.
References
- World Health Organization (2014) The End TB Strategy Genève, OMS 2014.
- Jabri H, Lakhdar N, Khattabi W, Afif H (2016) Les moyens diagnostiques de la tuberculose. Rev Pneumol Clin 72: 320-325
- Organization (2011) Rapid Implementation of the Xpert MTB/RIF Diagnostic Test, World Health Organization.
- World Health Organization (2016) Tuberculosis. Profile of country Senegal.
- World Health Organization (‎2010)‎ Treatment of tuberculosis: guidelines, 4th edn. Geneva.
- Steingart KR, Schiller I, Horne DJ, Pai M, Boehme CC, et al. (2014) Xpert® MTB/RIF assay for pulmonary tuberculosis and rifampicin resistance in adults. Cochrane Database Syst Rev : CD009593
- Kohli M, Schiller I, Dendukuri N, Dheda K, Denkinger CM, et al. (2018) MTB/RIF assay for extrapulmonary tuberculosis and rifampicin resistance. Cochrane Database Syst Rev 8: CD012768.
- Amante TD, Ahemed TA (2015) Risk factors for unsuccessful tuberculosis treatment outcome (failure, default and death) in public health institutions, Eastern Ethiopia. Pan Afr Med 20: 247
- Straetemans M, Straetemans M, Glaziou P, Bierrenbach AL, Sismanidis C, et al. (2011) Assessing tuberculosis case fatality ratio: A meta-analysis. Plos One 6: e20755.
- Fahrettin T, Senol K, Sedat A (2008) Factors associated with treatment success for tuberculosis : A Single center’s experience in Turkey. Jpn J Infect 61: 25-30
- Hassani L (2010) Les facteurs impliqueÌs dans l’abandon du traitement anti- bacillaire chez les patients atteints de tuberculose pulmonaire aÌ€ microscopie positive. Cas des preÌfectures Ain Chock – Hay Hassani – Nouaceur. ReÌgion du Grand Casablanca. MeÌm, INAS, Maroc; p: 86.
- Wohlleben J, Makhmudova M, Saidova F, Azamova S, Mergenthaler C, et al. (2017) Risk factors associated with loss to follow-up from tuberculosis treatment in Tajikistan: a case-control study. BMC Infect Dis 17: 543
- Diallo S, Dao S, DembeÌleÌ JP, Toloba Y, Kassambara H, et al (2008). Aspects eÌpideÌmiologiques de la tuberculose pulmonaire aÌ€ bacilloscopie positive au Mali pendant la deÌcennie 1995-2004. Mali MeÌdical 23: 25-29.
- Kigozi G, Heunis C, Chikobvu P, Botha S, Van Rensburg D, et al. (2017) Factors influencing treatment default among tuberculosis patients in a high burden province of South Africa. International Journal of Infectious Diseases 54: 95-102
- Pepper DJ, Marais S, Bhaijee F, Wilkinson RJ, De Azevedo V, et al. (2012) Assessment at antiretroviral clinics during TB treatment reduces loss to follow-up among HIV-infected patients. PLoS One 7: e37634.
- Lackey B, Seas C, Van der Stuyft P, Otero L (2015) Patient Characteristics Associated with Tuberculosis Treatment Default: A Cohort Study in High-Incidence Area of Lima, Peru. PLoS One 10 :e0128541.
- Waitt CJ, Squire SB (2011) Une revue systeÌmatique des facteurs de risque de deÌceÌ€s chez les adultes pendant et apreÌ€s le traitement de la tuberculose. Int J Tuberc Lung Dis 15: 871-885.
- Mfinanga SG, Kirenga BJ, Chanda DM, Mutayoba B, Mthiyane T, et al. (2014) Early versus delayed initiation of highly active antiretroviral therapy for HIV-positive adults with newly diagnosed pulmonary tuberculosis (TB-HAART): a prospective, international, randomised, placebo-controlled trial. Lancet Infect Dis 14: 563-571.
- Gninafon M, Tawo l, Kassa F, Monteiro GP, Zellweger JP, et al. (2004) Résultats du retraitement de la tuberculose en conditions de routine à Cotonou, Bénin. Int J Tuberc Lung Dis 8: 1242-1247
- Rakotonirina EJ, Razafimanampy AS, Mandrosovololona V, Rakotomanana-Razafintsalama H, Randriamarotia HWF, et al. (2011) Facteurs d’eÌchec au traitement antituberculeux aÌ€ Antananarivo : eÌtude cas-teÌmoins. La Revue MeÌdicale de Madagascar 1: 52-57
Citation: Déguénonvo LF, Cisse Diallo VMP, Mbaye KD, Déla Lawson AT, Lakhe NA, et al. (2019) Factors Associated with Confirmed Tuberculosis Treatment Outcome: A Hospital Study Cohort in Dakar, Senegal. J Infect Dis Ther 7: 409. DOI: 10.4172/2332-0877.1000409
Copyright: © 2019 Déguénonvo LF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2693
- [From(publication date): 0-2019 - Apr 27, 2025]
- Breakdown by view type
- HTML page views: 1916
- PDF downloads: 777