Review Article Open Access
Facilitators and Barriers to Exclusive Breastfeeding in Thailand: A Narrative Review
Thiwawan Thepha1*, Debbie Marais2, Jacqueline Bell3 and Somjit Muangpin11Department of Midwifery, Khon Kaen University, Thailand
2Warwick Medical School, University of Warwick, UK
3College of Life Sciences and Medicine, Polwarth Building, University of Aberdeen, Foresterhill, Aberdeen, UK
- *Corresponding Author:
- Thiwawan Thepha
RN, MNS, Lecturer, Department of Midwifery
Khon Kaen University, Thailand
Tel: +66 43 202 407
Fax: + 66 43 348 301
E-mail: r02tt14@abdn.ac.uk
Received date: February 09, 2017; Accepted date: February 22, 2017; Published date: February 28, 2017
Citation: Thepha T, Marais D, Bell J, Muangpin S (2017) Facilitators and Barriers to Exclusive Breastfeeding in Thailand: A Narrative Review. J Comm Pub Health Nurs 3:160. doi:10.4172/2471-9846.1000160
Copyright: © 2017 Thepha T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community & Public Health Nursing
Abstract
The six months exclusive breastfeeding rate in Thailand has decreased from 15.1 % in 2009 to 12.3 % in 2013. This narrative review aimed to identify facilitators and barriers to exclusive breastfeeding in Thailand. Medline, CINAHL, Embase, Google Scholar and the Thai Journal Online were searched using the terms exclusive breastfeeding and Thailand between 2001 to the end of September 2016. Inclusion criteria were that articles focused on facilitators and barriers of exclusive breastfeeding, specifically relating to Thailand. Narrative data extraction was conducted and data were analyzed thematically. Five themes were identified: mother factor, family support, situation and social context, infant factor, and healthcare (professionals and service). The themes described for Thailand in this study concur with international findings. Identifying specific practical interventions based on these themes, and in support of exclusive breastfeeding in Thailand, is now a priority.
Keywords
Facilitator and barriers to exclusive breastfeeding; Breastfeeding; Thailand; Narrative review; Nursing
Introduction
There is a wealth of evidence confirming that breastfeeding presents short and long term advantages for infants, mothers and, interestingly, the world. For infants, breast milk contains all the essential nutrients which stimulate optimal physiological and psychological growth and development [1-4]. In the short term, the incidence of childhood infections among breastfed children, such as diarrhea, respiratory infection, and other common childhood illnesses, tends to be lower due to the immunoglobulins present in breastmilk [5]. The incidence of childhood leukemia, the risk of being overweight or obese is also reduced [4,6]. A benefit of breastfeeding in oral health outcomes, the reduction of malocclusion has been found [7]. For long term benefits, otitis media in children up to the age of 2 years can be prevented by breastfeeding and in all breastfeeding is estimated to have saved the lives of more than 820,000 children under the age of 5 [4,8]. There is also evidence suggesting that the bonding between infants and mothers could be increased by breastfeeding [9]. Benefits to the mothers arise as a result of oxytocin and prolactin release, reducing the risk of postpartum hemorrhage, in addition to promoting uterine involution [10,11]. Additionally, breastfeeding can reduce the mother’s risk of certain illnesses, including ovarian cancer, type 2 diabetes, obesity, hypertension, heart disease, maternal depression, and mortality rate from breast cancer [1,4,10-16]. Longer periods of amenorrhea, which can lead to birth spacing, are associated with breastfeeding [13,17]. Breastfeeding has also been found to help women restore their body shape after delivery [4]. Not only health outcomes, but improvements in gender equality (in the workplace), money-saving, and fulfilling the mother’s potential are other obvious benefits [18,19]. For worldwide benefits, breastmilk is recognized as a natural and renewable food; and the ecological footprint of feeding infants is minimized [20]. In terms of global spending, breastfeeding can save US$ 302 billion annually [20].
Exclusive breastfeeding (EBF) is defined as infant feeding comprising only breast milk and not including water or other foods, although medicines, vitamin syrup or oral dehydration solution are permitted in case of medical necessity [21,22]. Internationally, since 2001, the World Health Organization (WHO) has recommended exclusive breastfeeding for six months and continued breastfeeding for up to two years [23,24]. The World Health Assembly set a global target for six months EBF at 50% by 2025 [25]. In 2015, the United Nations reported that breastfeeding is linked to the eight sustainable development goals i.e. poverty, hunger, health, education, gender equality, and sustainable consumption [19]. In response to this, the Thai Ministry of Public Health (MOPH) recently raised the national breastfeeding initiation goal to 60% by 2015 [26]. According to the 11th National Economic and Social Development Plan of Thailand 2012–2016, the goal for EBF for at least six months has been set at 30% and is set to be 50% amid the 12th National Economic and Social Development Plan of Thailand 2017–2021 [27,28]. It can be clearly seen that, from both an international and Thai perspective, 6-month EBF is an important issue with international pressure on countries to achieve this goal.
Globally, WHO reported that the six months EBF rate was just 36% [29] in 2014. At the regional level, the six months EBF rates for Europe, Africa, and the Eastern Mediterranean were 25%, 36% and 40%, respectively [29]. Nearly 50 % of the countries in the Asia-Pacific region have a six months EBF rate greater than 40% [30]. In Southeast Asia, the six months EBF rate in Cambodia, Indonesia and the Philippines are 74%, 42% and 34% respectively [31]. In term of economic patterns, the six months EBF rates in high income countries tend to be lower than those in low and middle income countries (e.g. in the United States of America and the United Kingdom were 19% and 1 %; see Table 1). High income countries’ six months EBF rates tend to be below 20% [31]. In contrast, many of the six months EBF rates in low and middle income countries are close to, or have already achieved the 50% WHO goal, ranging from 28% in China to as high as 89% in Korea [31]. Nowadays, the world breastfeeding trends initiative (WBTi) is a worldwide tool to assess the strengths and weaknesses of national policies and programmes concerned with EBF [32]. Some countries in Asia, such as Sri Lanka, Vietnam, and Philippines were reported as grade B, and others, including Taiwan and Thailand, were reported as grade C, indicating weakness regarding EBF [32,33].
| Country (year reported) | EBF rate for 6 months (%) |
|---|---|
| United States of America (2014) | 19 |
| United Kingdom (2014) | 1 |
| Uganda (2011) | 63 |
| Sudan (2010) | 41 |
| Pakistan (2012) | 38 |
| China (2008) | 28 |
| Korea (2009) | 89 |
| Indonesia (2012) | 42 |
| Cambodia (2010) | 74 |
| Philippines (2008) | 34 |
Table 1: International EBF rates for six months, EBF=Exclusive Breastfeeding.
In Thailand, the six months EBF rate was reported as 14.5% in 2005 [34] and increased slightly to 15.1% in 2009 [35] (Table 2). In 2013 however, reported six months EBF rates had dropped to 12.3% due to the decrease in rates in the Northeast region [36]. It is important to note that the six months EBF rates vary considerably at the regional level. In 2009, the six months EBF rates for the Northeast, South, North, and Central regions were 26.9, 10.4, 9.4 and 6.1% respectively, and the lowest percentage was found in Bangkok, at 1.7% [35]. In the 2013 national survey, the six months EBF rates in Bangkok, Central, North and South regions had increased [36]. In contrast, the six months EBF rate in Northeast Thailand was significantly lower, dropping from 26.9% in 2009 to 13.8% in 2013 which is of grave concern. It is also worth noting that over the same period, the percentage of Thai infants receiving breast milk 24 hours post delivery fell from 84% in 2009 to 46.3% in 2013 [35-37]. This indicates that there seem to be fewer women initiating breastfeeding, as well as fewer continuing for the full six months.
Over the past 25 years, there have been many initiatives aiming to increase the EBF rate in Thailand. The first national breastfeeding strategy in Thailand was initiated in 1989, and at that time the goal was EBF for four months [38]. In 2002, the 9th National Economic and Social Development Plan of Thailand 2002–2006 set the goal of EBF for six months to 30% in response to the WHO target [39]. In order to improve the EBF rate in Thailand, the Baby-Friendly Hospital Initiative (BFHI) has been promoted since 1997 and most Thai hospitals (more than 792 hospitals) have reached Baby Friendly status by following the 10 steps to successful breastfeeding [38]. The Family Love Bonding project, initiated by His Royal Highness, Crown Prince Maha Vajiralongkorn, is a large project in Thailand involving more than 90% of government hospitals which includes improving EBF rates as one of its strategies [40]. Furthermore, the Ministry of Public Health (MOPH) in Thailand announced “The Thailand Code of Marketing of Foods for Infants & Young Children and Related Products 2008, which implements the WHO International Code of Marketing of Breastmilk Substitutes [41]. Paid maternity leave for 90 days was initiated [42]., and medical benefits, delivery care and newborn nursing expenses, are supported by the social security fund [42]. Not only government organizations, but also non-government organizations are running EBF projects. UNICEF has many campaigns to report the EBF situation in Thailand, designed to stimulate EBF nationally, for example, the “powdered milk = risk” campaign [43]. The Thai Breastfeeding Center Foundation is an organization that supports EBF and has conducted various breastfeeding community projects, including introducing breastfeeding areas in work places, arranging EBF conferences for healthcare professionals, producing newsletters and articles, and, in 2014, setting the breastfeeding slogan: “Breastfeeding: A winning goal - for life” [40,41].
| EBF at least 6 months Rate (%) | |||||||
|---|---|---|---|---|---|---|---|
| Year | Whole Kingdom | Bangkok | Central | North | Northeast | South | Author |
| 2009 | 15.1 | 1.7 | 6.1 | 9.4 | 26.9 | 10.4 | NSO Thailand, 2010 |
| 2013 | 12.3 | 8.2 | 7.9 | 19.6 | 13.8 | 12.2 | NSO Thailand, 2013 |
Table 2: 6 months EBF rate in Thailand and its regions, EB=Exclusive Breastfeeding, NSO Thailand=National Statistical Office Thailand.
In order to improve the six months EBF rate in the worst affected region of Thailand and contribute towards achieving the goal set by the MOPH for the Kingdom of Thailand, it is important to determine the facilitators and barriers to exclusive breastfeeding for Thai mothers. This information will be useful for policy planning that aims to have an impact on six months EBF rates in the Northeast of Thailand, by enabling the prioritization of the identified factors. The aim of this study was therefore, to review relevant literature and identify facilitators and barriers to EBF in Thailand.
Materials and Methods
A comprehensive review of literature was conducted using a systematic searching approach. The following data bases were searched: Medline, CINAHL, Embase, Google Scholar and the Thai Journal Online between the first week of January 2001 and the fourth week of September 2016. The search strategy included broad search terms in two blocks related to EBF and Thailand, and focused the results by linking them with the relevant Boolean terms [Table 3]. Titles and abstracts were screened for inclusion. All study designs, all languages, populations including women, men, mothers, grandmothers and health care professionals, type of publication including article, report, thesis and conference papers were included. Studies were excluded if they did not focus on barriers and facilitators of EBF or if they were not conducted in Thailand. Regular meetings with the supervision team were held to verify emerging findings. Narrative data extraction was conducted, and data were analyzed thematically to identify facilitators and barriers to EBF in Thailand.
Results
General characteristics
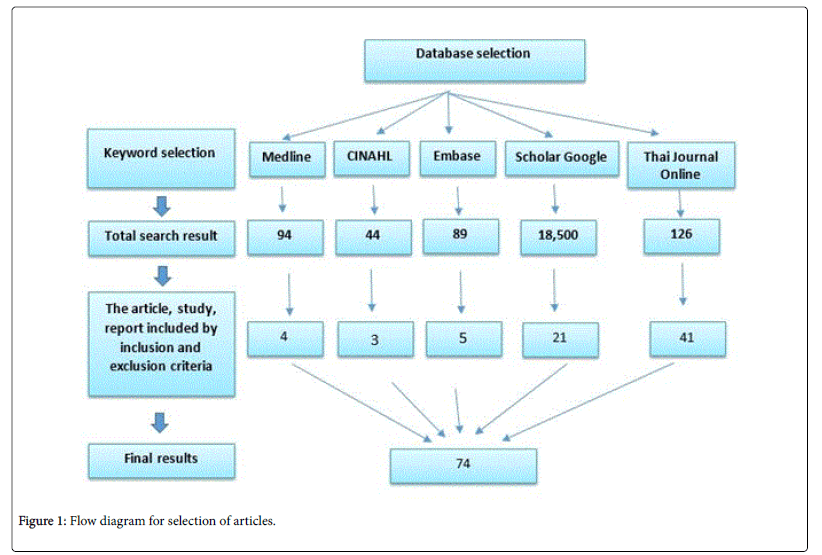
The systematic search of literature identified 18,853 relevant studies across the five databases (Figure 1), with the majority being in Google Scholar and the Thai Journal Online. In total, 74 studies complied with the inclusion and exclusion criteria; the main reason for exclusion was that the focus was not on facilitators and barriers of EBF, but most often on the promotion of EBF. In Google Scholar only the first 10 pages of results were screened.
| Keywords | Exclusive breastfeeding | Thailand |
|---|---|---|
| Sub-Keyword | 6 months breastfeeding | Northeast Thailand |
| Breastfeeding exclusive | Northern Thailand | |
| Breast feeding | Southern Thailand | |
| Central of Thailand | ||
| Eastern Thailand | ||
| Western Thailand |
Table 3: Keywords use in article search.
The selected studies had a good geographical spread with 29 from Central Thailand, five from Southern Thailand, six from Northern Thailand, one from Eastern Thailand, one from Western Thailand, 16 from North-eastern Thailand and 16 that did not specify a region. Of the studies, 55 were journal articles, 11 were reports, six were theses, and two was a conference paper. The studies were mostly published between 2015 and 2016 [n=8] and 2010 - 2014 [n=47], with the remainder being published earlier (2005-2009 [n=14], 2001-2004 [n=5], respectively). The majority of the studies, 83.78% (62 studies) were quantitative, with seven studies were qualitative and only five studies were mixed methods.
Facilitators and barriers
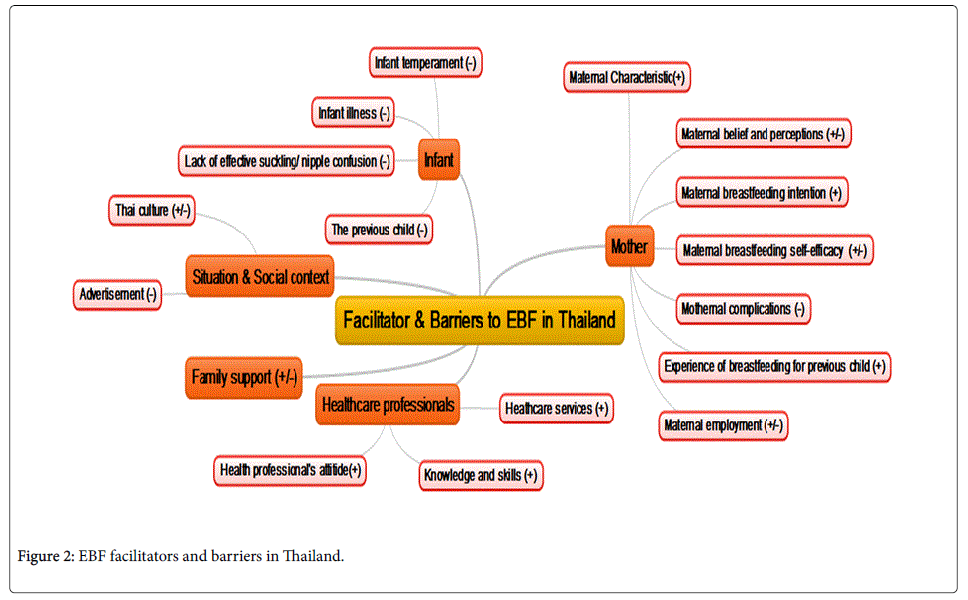
A facilitator is a factor that supports or has positive influence or effect on EBF, whereas a barrier is a factor that obstructs or has a negative influence or effect on EBF. Several facilitators and barriers to EBF in Thailand were identified and divided into five themes as follows: mother factors, infant factors, health professional and health care system factors, family factors, and situation and social context factors (Figure 2).
Mother factor
As a result of the review, the mother factor is divided into seven groups: maternal characteristics, maternal belief and perceptions, maternal breastfeeding intention, maternal breastfeeding self-efficacy, maternal complications, experience of breastfeeding for previous child, and maternal employment.
Maternal characteristics
Maternal characteristics include: age, marital status, economic status, education level, and knowledge regarding EBF. According to cognitive theory, responsible behavior is correlated with age [44], which may explain the finding of this review that mothers who are older are more likely to experience success with EBF. Many studies showed that mothers who are older than 25 years are more likely to succeed with EBF[18,45-49], whereas teenage mothers are less likely to use EBF[9,18,46,50]. Some studies in Thailand found that being married leads to more successful EBF than being single [18,46]. Mothers with a high economic status displayed longer breastfeeding duration than mothers with a lower economic status [51]. The education level of the mother was found to be positively linked to EBF, with educated mothers breastfeeding for longer [45,52]. Lastly, many studies showed that when a mother knows about the advantages of breast milk, this can strengthen her intention to breastfeed, and in addition may increase the duration of breastfeeding [18,48,52-58]. Furthermore, studies showed that knowing how to express and store breast milk can improve breastfeeding confidence [49,52,53,59,60]. In contrast, a lack of knowledge concerning breastfeeding can present an obstacle [18,61-64].
Maternal belief and perception
These factors include believing in their own capabilities, positive and negative attitude towards breastfeeding. Mothers who believe in their own capabilities are more likely to be successful with breastfeeding [18,50,52]. Nine studies reported that a mother’s positive attitude/perception towards breastfeeding can lead to a longer duration of EBF [18,45,48,52,54-56,65,66]. In contrast, some studies found that negative attitudes towards EBF are often reported, such as perceiving that breastfeeding is complicated, that providing other supplementary food will improve the child’s nutrition, that breast milk is not nutritionally complete or adequate for their babies, that breast milk could result in neonatal hyperbilirubinemia or that breastfeeding results in an undesirable body shape (breast shape). In addition, mothers may feel shame when breastfeeding or expressing milk in public areas, or believe breast milk is not suitable for an infant for the whole of the first six months [9,18,52,67,68]. Some mothers also seem to have a negative perception with regard to the amount of breast milk produced and may report “insufficient milk supply”[9,46,67-69].
Maternal breastfeeding intention
The review showed that a mother’s intention to succeed with EBF was positively related to the duration of EBF [46,47,50,53,65,70, 71].
Maternal breastfeeding self-efficacy
High self-efficacy can lead to high performance [48,60,72-74]. A study by Poungkaew showed that mothers with a high score of selfefficacy intended to continue with EBF for longer than mothers who had a low score [75]. Furthermore, Nualjam et al. found that mothers with high levels of self-efficacy were able to overcome difficulties encountered in breastfeeding, whereas ‘first time’ mothers in particular, may lack confidence in providing breast milk [18].
Maternal complications
Physical conditions in the mother, such as inverted, retracted or flat nipples, breast pain, postpartum depression, smoking and drug addiction were reported as influential barriers to EBF [18,46,67,76-78]. Moreover, mothers who had a caesarean section were more likely to report difficulty breastfeeding initially or “having to give formula milk” [69].
Experience of breastfeeding for previous child
Several studies reported that the experience of a mother, for example, experience of breastfeeding a previous child or not having any problems with breastfeeding during the first month, can be supportive to EBF [18,45,52,53].
Maternal employment
Several studies found that working mothers tend to breastfeed for shorter periods because of difficulty in maintaining lactation, partly due to the stress and conflict involved in combining breastfeeding with work [47,62,76,77]. Furthermore, studies also revealed that mothers who work away from home in different provinces find it particularly inconvenient to breastfeed or provide breast milk [9,18,52,61,67]. Some studies reported that short periods of maternity leave (i.e the three months legal minimum) can be a barrier to EBF [37,69,71,79-81]. The work place was identified as another obstacle to EBF because it is often not suitable for breastfeeding, with some work places not providing a breastfeeding area or refrigerators to store breast milk, and mothers feeling insecure pumping or feeding at work, as well as a lack of support from employers and colleagues [9,18,63,68]. Work characteristics may also negatively affect EBF duration, especially for shift workers [18,63,68]. In contrast, three studies showed that workplace support for breastfeeding, including developing a workplace breastfeeding support model for lactating mothers and a breastfeeding support campaign, can increase the EBF rate [82-84].
Family
In Thailand, family can be both a facilitator and a barrier. 10 studies reported that the family can be a positive factor supporting EBF, (i.e. grandmother, grandfather, and especially the husband) [47,48,53,54,60,63,64,66,68,85-87]. Wangsawat and colleagues found that the father’s knowledge about breastfeeding and his intention to support EBF has a positive relationship with the mother’s intention to EBF for 6 months [57]. However, lack of family support was also identified as a barrier which can lead to a short duration of EBF because most working mothers need someone to take care of their child and reduce the burden of housework [18,62,68].
Situation and social context
Thai traditional culture can be seen to have positive and negative impact on EBF. In term of positive impact, “Ka Nam Nom” is a term which refers the value of breastmilk [58]. Thai people believe that infants can grow effectively as a result of breast milk intake; therefore this culture acknowledges as the value of breast milk and, at wedding ceremonies, the groom is required to give property to the bride’s parents equal to the value of breastmilk [58]. Moreover, Thai citizens believe that, breast milk is produced from maternal blood circulation. Some Thai mothers breastfeed because they know that their breast milk comes from their own blood [58]. “Yuu Deaun” is a traditional practice in Northern Thailand, whereby, over the course of a one month period, new mothers must stay at home and reduce their activity [58]. Moreover, certain foods such as ginger which stimulated the volume of breastmilk are served at this time and some foods are prohibited [88]. If the infant needs to be admitted to hospital, mothers who are on the “Yuu Deaun” period cannot visit their child, which can be a barrier to EBF [58]. On the other hand, as result of reducing activities, mothers spend time with their infants and high breastfeeding rates are associated with the period of “Yuu Deaun” [58]. Other studies report that grandparents can present an obstacle to EBF as they sometimes provide other sustenance, such as water, rice, and fruit to the infant [18,66,67,69,89]. In addition, the advertising of formula milk in Thailand [9,18] and the provision of formula milk while infants are in hospital have been shown to negatively impact EBF [50,52].
Infant
The infant was found to present a barrier in some studies. The lack of effective suckling and nipple confusion could lead to problems [18,46,47], and several studies reported that infants’ temperaments could be a barrier to EBF [67,76,90,91]. Also early illnesses, especially those involving a hospital admission were reported as further barriers to EBF [18,46,55,56,62,67,92]. Interestingly, having had previous children was reported as a barrier as well as a facilitator, especially among mothers who had given formula milk to previous healthy children [9].
Healthcare professional and health care system factor
A positive attitude among health care professionals was identified as a facilitator of EBF [18]. The knowledge and skills of health care professionals regarding EBF were also been reported to have a positive impact on EBF rates [18]. Moreover, supportive health care services, including a 6 month post-natal check, 24 hour counselling, hotlines, home visits, telephone follow up, nurse support, breastfeeding guidelines, education programmes, breastfeeding promotion programmes and good access to healthcare in the antenatal and postpartum periods were reported as facilitators of EBF [45,50,61,68,73,74,81-83,87,93-112].
Discussion
The review identified various facilitators and barriers to EBF in Thailand. Facilitators of EBF related to the mother factor were, being older [>25 years], married, with a high income and a reasonable level of education. Mother’s breastfeeding knowledge, such as knowing the advantages of breastfeeding and being aware of how to express and store breast milk, were also identified as facilitators of EBF. These findings are corroborated by various studies in other parts of the world [3,113,114]. Similarly, in the South East Asian region, a study conducted in Laos found that mothers older than 35 years tended to continue EBF for a year, although in contrast, those with low economic status were more likely to continue to breastfeed [115]. In Malaysia, Tan found that not working was also a facilitator to EBF [116]. Further facilitators related to the mother identified in the review include her having a high level of confidence, positive attitudes, a strong intention to breastfeed and a good experience with a previous child; these are also corroborated by similar findings in other countries [116,117].
Barriers related to maternal factors identified in the review included being a teenage mother, doing manual labor, working away from home and a lack of breastfeeding knowledge, which are similar to findings in Laos, India, Vietnam and Zimbabwe [114,115,118,119]. Additional barriers related to the mother were being a first time mother, her physical condition (such as nipple problems and breast pain) and negative attitudes to breastfeeding. Other studies in various countries and regions [Pakistan, Zimbabwe, United Arab Emirates, Ghana, Uganda, West Africa and China] have identified insufficient breast milk supply reported as a barrier to 6 months EBF by mothers [113,114,117,120-124]. Breast conditions have been reported as a barrier in other studies conducted in the United Arab Emirates, Pakistan, Africa, and South America [113,117,121,125,126]. Short maternity leave, shift work and a lack of workplace support were reported as barriers in the review, which is consistent with findings in other countries [113,119,127].
Family can be both a facilitator and a barrier. Support from family members (i.e. grandparents or the husband) was shown to have a positive impact on EBF, and this has been found in other studies [114,116,121,122,128,129]. Lack of family support was also identified as barrier in a study in India [130].
The Thai culture can present both facilitators and barriers. The findings revealed that culturally, “Ka Nam Nom” can stimulate the initiation of breastfeeding. “Yuu Deaun” is identified as both a facilitator and a barrier. In addition, Thai grandmothers trying to feed infants water, rice, and fruit can negatively impact on EBF duration. Similar traditional behaviors have also been reported in the Middle East, Southern Africa, East Africa, China and Brazil [113,123,128,131]. In Zimbabwe, water as well as herbal concoctions, are given to children with the belief that they could improve their health [114]. These cultural habits are not only ascribed to grandmothers, but also to mothers [121].
Infant-related factors found to affect EBF include the infant’s temperament, illness, hospital admission, lack of effective suckling, nipple confusion and negative previous experiences, which have all been reported as barriers to EBF. These finding are corroborated by studies in other countries [132,133]. In India, persistent crying in infants was found to be a barrier to EBF and, in Iran, low birth weight was reported to lead to a low rate of breastfeeding [132,133]. Tan found that having a full-term infant can be a facilitator to EBF [116].
Other facilitators to EBF in Thailand are good knowledge and skills among health care professionals and accessible health care services, which has been found in other studies [115,117,134]. In the USA, the knowledge of nurses has been shown to influence breastfeeding and in contrast a lack of continuity of care with regard to breastfeeding can affect the duration of EBF [134]. In Pakistan, antenatal counselling of mothers was found to significantly increase the breastfeeding rate [117]. A study in Laos showed that mothers who joined an antenatal service experienced early breastfeeding initiation [115].
Strengths and Limitations
The main strength of the study is that the review sought to include all relevant literature from Thailand using a comprehensive search strategy. Some grey literature was also included to ensure that as many findings as possible were captured, even if they were unpublished. Many of the reports were not identified by indexed databases but by searching local, publicly accessible literature. The inclusion of articles and reports written in Thai is a further strength. A limitation of the study is that the relevant studies were not assessed in terms of the quality of the study designs, and bias was not assessed.
Conclusion
This review aimed to identify the facilitators and barriers to EBF in Thailand. Mother factors, family support, situation and social context, infant, and health care professionals have emerged as important influences on EBF in Thailand, many of which are similar to findings in other countries, but some being unique to Thailand. It is hoped that health professionals involved in promoting, protecting and supporting breastfeeding in Thailand, and possibly countries within the region, will be able to utilize the findings of this study as a basis for further or comparative research. The identified facilitators and barriers may serve as a framework to engage stakeholders in the planning of interventions and policies to improve EBF rates in Thailand and surrounding countries where the cultures are similar. As very little qualitative research was identified, it is recommended that more such research should be conducted to investigate the perceptions of all stakeholders in identifying the best interventions to improve EBF rates in Thailand and the surrounding countries.
Acknowledgement
This article is derived from the dissertation requirements for a PhD in Nursing at the University of Aberdeen.
References
- Semrau K, Kuhn L, Brooks RD, Cabral H, Sinkala M, et al. (2011) Exclusive breastfeeding, maternal HIV disease and the risk of clinical breast pathology in HIV-infected, breastfeeding women. Am J Obstet Gynecol 205: e1-e8.
- Tamiru D, Belachew T, Loha E, Mohammed S (2012) Sub-optimal breastfeeding of infants during the first six months and associated factors in rural communities of Jimma Arjo Woreda, Southwest Ethiopia. BMC Public Health 12: 363.
- Thakur S, Roy S, Pual K, Khannam M, Khatun W, et al. (2012) Effect of nutrition education on exclusive breastfeeding for nutritional outcome of low birth weight babies. Eur J Clin Nutr 66: 376-381.
- Victora CG, Bahl R, Barros AJ, França GV, Horton S, et al. (2016) Breastfeeding in the 21st century: Epidemiology, mechanisms and lifelong effect. Lancet 387: 475-490.
- Horta BL, Victora CG (2013) Short-term effects of breastfeeding: A systematic review of the benifits of breastfeeding on diarhoea and pneumonia mortality. WHO, Geneva.
- Bowatte G, Tham R, Allen KJ, Tan DJ, et al. (2015) Breastfeeding and childhood acute otitis media: A systematic review and meta-analysis. Acta Paediatr 104: 85-95.
- Bowatte G, Tham R, Allen KJ, Tan DJ, et al. (2015) Breastfeeding and childhood acute otitis media: A systematic review and meta-analysis. Acta Paediatr 104: 85-95.
- Amitay EL, Keinan-Boker L (2015) Breastfeeding and childhood leukemia incidence: A meta-analysis and systematic review. JAMA Pediatr 169: e151025.
- Thophothai T, Thaijinda C, Seartgaikul N, Phuthasri V, Bunthumchareung K, et al. (2013) The study of perception of exclusive breastfeeding promotion and powdered advertisement with knowledge, attitude and decision of mother and relative, Thailand.
- Peres KG, Cascaes AM, Nascimento GG, Victora CG (2015) Effect of breastfeeding on malocclusions: A systematic review and meta-analysis. Acta Paediatr 104: 54-61.
- Stuebe AM, Schwarz EB (2010) The risks and benefits of infant feeding practices for women and their children. J Perinatol 30: 155-162.
- York E, Hoban E (2013) Infant feeding intentions among first time pregnant women in urban Melbourne, Australia. Midwifery 29: 787-793.
- Liu B, Jorm L, Banks E (2010) Parity, breastfeeding and the subsequent risk of maternal type 2 diabetes. Diabetes Care 33: 1239-1241.
- Chowdhury R, Sinha B, Sankar MJ, Taneja S, Bhandari N, et al. (2015) Breastfeeding and maternal health outcomes: A systematic review and meta-analysis. Acta Pædiatr 104: 96-113.
- Aune D, Norat T, Romundstad P, Vatten LJ (2014) Breastfeeding and the maternal risk of type 2 diabetes: A systematic review and does-response meta analysis of chort studies. Nutr Metab Cardiovasc Dis 24: 107-115.
- Dias CC, Figueiredo B (2015) Breastfeeding and depression: A systematic review of the literature. J Affect Disord 171: 142-154.
- Bobrow KL, Quigley MA, Green J, Reeves GK, Beral V (2013) Persistent effects of women's parity and breastfeeding patterns on their body mass index: Results fromthe million women study. Int J Obes 37: 712-717.
- Nualjam P, Phumthritikun P, Muttawangkul C, Kumrot W, ChunchaChreun K, et al. (2013) Factors affected to behavior and during time for breastfeeding of Pasi Charoen persons, Thailand.
- Kramer MS, Kakuma R (2012) Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev 8: CD003517.
- United Nations (2015) Transforming our world: The 2030 agenda for sustainable development, New York.
- Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, et al. (2016) Why invest, and what it will take to improve breastfeeding practices? Lancet 387: 491-504.
- Binns CW, Fraser ML, Lee AH, Scott J (2009) Defining exclusive breastfeeding in Australia. J Paediatr Child Health 45: 174-180.
- WHO (2013) Exclusive breastfeeding. Nutrition.
- World Health Oranization (2013) WHO recommendations on postnatal care of the mother and newborn. Maternal, newborn, child and adolescent health.
- World Health Oranization (2001) Global strategy for infant and young child feeding: The optimal duration of exclusive breastfeeding.
- World Health Oranization (2015) Dissemination of WHO guidelines and recommendations on micronutrients: Policy, practice and service delivery issues.
- MCOT (2013) Exclusive breastfeeding campaign intensified in Thailand, Thailand.
- National Economic and Social Development Board (2012) 11th national economic and social development plan of Thailand A.D.2012-2016, Thailand.
- Srliaranai S (2016) 12th National Economic and Social Development Plan of Thailand 2017��?2021: Framework, Thailand.
- World Health Oranization (2014) Exclusive breastfeeding under 6 months: Data by WHO region.
- World Health Oranization (2012) Health at a glance: Asia/Pacific 2012. OECD.
- World Health Oranization (2014) Exclusive breastfeeding under 6 months: Data by country.
- IBFAN (2015) The world breastfeeding trends initiative (WBTi): Thailand 2015, Thailand.
- Department of Health (2006) Annual report 2005, Thailand.
- IBFAN (2015) World breastfeeding trends initiative (WBTi) tracking.
- 36. National Statistical Office Thailand, UNICEF, MOPH, NHSO, THPF, IHPP (2013) Multiple indicator cluster survey: MICS4, Thailand.
- National Statistical Office Thailand, MOPH, UNFPA (2009) The 2009 reproductive health survey, Thailand.
- . National Statistical Office Thailand, UNICEF, MOPH, NHSO, THPF, IHPP (2013) Multiple indicator cluster survey: MICS4, Thailand.
- Plewma P (2013) Prevalence and factors influencing exclusive breast-feeding in Rajavithi hospital. J Med Assoc Thai 96: s94-s99.
- Ministry of Social Development and Human Security (2014) The family relationship project, Thailand.
- Hangchaovanich Y, Voramongkol N (2006) Breastfeeding promotion in Thailand. J Med Assoc Thai 89: S173- S177.
- Thai breastfeeding center foundation (2014) Breastfeeding, Thailand.
- National Economic and Social Development Board (2002) 9th national economic and social development plan of Thailand A.D.2002-2006, Thailand.
- IBFAN (2012) Report on the situation of infant and young child feeding in Thailand, Thailand.
- Chuprapan P, Thiangthum W, Pichayapinyo P (2014) Factors influencing exclusive breastfeeding within a 6 months period among mother in south central region of Thailand. Proceeding of Graduate research conference.
- Youngwanichsetha S (2013) Factors related to exclusive breastfeeding among postpartum Thai women with a history of gestational diabetes mellitus. J Reprod Infant Psychol 31: 208-217.
- UNICEF (2014) UNICEF, partners launch ��?powdered milk=risk� campaign, New York.
- Botwinick J (1967) Cognitive processes in maturity and old age. Springer, USA.
- Nuampa S, Sinsuksai N, Phahuwatanakorn W, Chanprapaph P (2013) Personal factors, first feeding time and nurse support in predicting successful exclusive breastfeeding at discharge in mothers with cesarean section. J Nurs Sci 31.
- Joungpanish P, Threeratuntikarn V, Thanakitjareung T, Koavathana N (2011) The influent factors of breastfeeding for 6 months of mother at Soung Nung District, Thailand.
- Chusilp K, Bangsainoi K (2011) Sustainability of exclusive breastfeeding for 6 months and infant health outcomes in baby-friendly hospitals. Proceeding of the 16th Annual International Meeting of the Academy of Breastfeeding Medicine. Miami, United States.
- Apivantana C, Houngthai S (2011) The influent factors of exclusive breastfeeding for 6 months, Thailand.
- Wongphinit U, Sinsuksai N, Yusamran C (2016) Personal factors, social support and effective suckling at discharge in predicting exclusive breastfeeding at one month among first-time mothers. J Royal Thai Army Nurs 17: 88-95.
- Mekkamol K, Deejapo J, Netgrajang C (2013) Effect of breastfeeding promotion based on family-centered care on knowledge, attitude of mothers and families, and exclusive breastfeeding rate for 6 months. Journal of Phrapokklao Nursing College 24.
- Promsaka W (2005) Evaluation of breast feeding promotion process in health promoting hospital regional health promotion center 6, Thailand.
- Suijam R, Tongsai J, Tongyum S (2009) The influent factors of the successful of exclusive breastfeeding for six months, Thailand.
- Wangsawat T, Kaleang N, Phibal A, Jaisomkom R, Hayeese W (2014) Factors influencing intention to exclusive breastfeeding for 6 months of mothers in Naradhiwat Province. Nursing Journal 41.
- Chanapai S, Sinsuksai N, Thananowan N, Phahuwatanakorn W (2014) Knowledge, attitude, self-efficacy, spousal and nurse support predicting 6 weeks exclusive breastfeeding. J Nurs Sci 32.
- Chaiyavattana M (2007) The factor that influence to exclusive breastfeeding for 6 months at region health promotion center 4 Rachaburi, Thailand.
- Wungkum A, Thaiyapirom N, Jintrawet U (2011) Factors related to continued breast feeding among mothers with preterm infants. Nursing Journal 38.
- Paiprasirt S (2005) The effective of exclusive breastfeeding integration to exclusive breastfeeding rate for 6 month at Nakornsawan. Thailand Journal of Health Promotion 28.
- Yimyam S (2003) Breastfeeding practice among employed Thai women: A cultural perspective. Thai J Nurs Res 7.
- Puapornpong P, Raungrongmorakot K, Hamontri S, Ketsuwan S, Wongin S (2016) Latch score and exclusive breastfeeding during the first six months postpartum. Journal of Medicine and Health Sciences 23.
- Yan L, Lijuan K, Masanaka H (2002) Breast-feeding in Bangkok, Thailand: Current status, maternal knowledge, attitude and social support. Pediatr Int 41: 648-654.
- Rutsameejam P, Khompayuk J, Thanasombut K (2009) The development program of continuing care to promote breast feeding in Primigravida: A case study at Hua-Chiew hospital. Journal of The Royal Thai Army Nurses 10.
- Phosasavat N (2012) The factor that affect exclusive breast feeding only at least 6 months of postpartum mother in Kummaung, Kalasin province, Thailand.
- Rodchumphu T (2012) Breastfeeding situation in public health inspection region 10 and 12. Journal of Region Health Centre 6 khonkaen, Thailand.
- Bunjun J, Phathuviwatana P, Choawacharean P, Chusil K (2011) Development of service for promoting sustainable breastfeeding. Journal of Nurse's Association of Thailand, North-Eastern Division 29:14-24.
- Tangsuksan P, Ratinthorn A (2011) Experiences and contextual factors related to exclusive breastfeeding in full-time working mothers. Journal of Nursing Science 29.
- Suwannobol N, Wacharasin C, Deoisres W (2015) The problems and needs of breastfeeding promotion among adolescent mothers: A case study of Dankhunthot hospital. Journal of Nursing and Health Care 33.
- Barnes BS, Perngparn U (2013) Exclusive breastfeeding experiences among mothers in Bangkok, Thailand: Findings from a mixed-methods study. Journal of Health Research 27: 19-25.
- Weiner B (1995) Judgments of responsibility: A foundation for a theory of social conduct. The guilford press, NewYork.
- Kimphitak A, Lagampan S, Thiangtham W (2011) The effects of a breastfeeding self-efficacy intervention in first-time mothers. J Public Health 41.
- Budsaengdee B, Kantaruksa K, Chareonsanti J (2013) Effects of Self-efficacy promotion on success in exclusive breastfeeding among cesarean section mothers. Nursing Journal 40.
- Poungkaew N (2005) Effects of self-efficacy promoting program on breastfeeding behaviors and duration among first-time working mothers, Thailand.
- Laisiriruangrai P, Wiriyasirivaj B, Phaloprakarn C, Manusirivithaya S (2008) Prevalence of exclusive breastfeeding at 3, 4 and 6 months in Bangkok Metropolitan Administration Medical college and Vajira hospital. J Med Assoc Thai 91: 962-967.
- Bandura A (1977) Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 84: 191-215.
- Puapornpong P, Manolertthewan W, Raungrongmorakot K, Ketsuwan S, Wongin S (2009) Factors effecting on breastfeeding success in infants up to 6 months of age in Nakhon Nayok province. Journal of Medicine and Health Sciences 16.
- Raweepakawat T (2013) The result of frenulotomy on breast feeding difficulty due to tongue tie: follow up 6 months at Health Promotion Hospital Region I Bangkok. Thammasat Medical Journal 13.
- Photaworn P, Pensuwan A, Sriyannalak N (2013) Breastfeeding among teenage mothers in Muang Songkhla municipality. Nursing Journal of the Ministry of Public Health 23.
- Aikawa T, Pavadhgul P, Chongsuwat R, Sawasdivorn S, Boonshuyar C (2012) Maternal return to paid work and breastfeeding practices in Bangkok, Thialand. Asia Pac J Public Health 27: NP1253- NP1262.
- Yimyam S, Thapphansan P, Chumphan S (2012) Development of ways of promoting breastfeeding in workplaces. Thai Journal of Nursing Council 27.
- Pathumwiwatana P, Tongsukho S, Naratippakorn T, Pradubwong S, Chusilp K (2010) The promotion of exclusive breastfeeding in infants with complete cleft lip and palate during the first 6 months after childbirth at Srinagarind Hospital, Khon Kaen province, Thailand. J Med Assoc Thai 93: S71-S77.
- Bunlikitkul T (2013) Promoting full-time working mothers outside the home to continue breastfeeding exclusively. Thai Red Cross Nursing Journal 6.
- Suriyakun A (2005) The effects of home visit to perception of breast feeding and family support towards exclusive breastfeeding. Khon Kaen university, Thailand.
- Pichianwilai W, Chanthapreeda N (2014) The effect of a planned behavior program on exclusive breastfeeding behavior among working mothers. Journal of Nursing Science and Health 37.
- Yimyam S, Hanpa W (2014) Developing a workplace breast feeding support model for employed lactating mothers. Midwifery 30: 720-724.
- Chisuwan C, Prasopkittikun T, Sangperm P, Payakkaraung S (2012) Predictive power of support from husbands, grandmothers and nurses on duration of exclusive breastfeeding. Journal of Nursing Science 30.
- Srisawat S, Vichitsukon K, Prasopkittikun T (2013) Effect of promoting grandmothers��? role in providing breastfeeding support for First-time mothers. Journal of Nursing Science 31.
- Paritakul P, Ruangrongmorakot K, Laosooksathit W, Suksamarnwong M, Puapornpong P (2016) The effect of ginger on breast milk volume in the early postpartum period: A randomized, double-blind controlled trial. Breastfeed Med 11: 361-365.
- Kamolkhon V (2009) The factors affecting the at least 6 months feeding only by milk of postnatal mother in Nong Bua health centre, Nongkungsri district, Kalasin province. Research and Development Health System Journal 2: 16-25.
- Khobkhun J, Saritsumbut P, Khurirungputjai N (2003) Factors influencing duration of exclusive breast-feeding. Changmai university, Thailand.
- Baisuwan S, Jirapaet V (2011) Selected factors associated with breast feeding promotion behavior of staff nurse. Journal of Nursing science Chulalongkorn University 23.
- Kanhadilok S (2013) Breastfeeding influencing factors in Thai adolescent mothers, Thailand.
- Phahuwatanakorn W, Soothampitag M (2013) Comparison of breastfeeding problems during early postpartum between mothers with exclusive breastfeeding and mothers with non-exclusive breastfeeding at 1 Month. Journal of Nursing Science 31.
- Thavonvattana S, Sawasdivorn S, Buhsabun W (2011) Support program increases exclusive breastfeeding rate in hospital personnel at Queen Sirikit National Institute of Child Health (QSNICH). Proceeding of the 16th Annual International Meeting of the Academy of breastfeeding medicine.
- Thammachote P, Lawantrakul J (2011) The effects of breastfeeding-promoting program within 48 h post cesarean section on mother's breastfeeding behavior and infant's breastfeeding suckling behavior at Songklanagarind hospitae. Songklanagarind Journal of Nursing 31.
- Ratisunthorn J (2014) Effects of empowerment program on breastfeeding behavior and duration of exclusive breastfeeding among adolescent mothers. Kuakarun Journal of Nursing 21.
- Thussanasupap B, Lapvongwatana p, Kalampakorn S, Lynn D (2016) Effects of the community--based breastfeeding promotion program for Working Mothers: A quasi-experimental study. Pac Rim Int J Nurs Res Thail 20: 196-209.
- Pathumwiwatana P, Jaturat N, Thinkhamrop J, Chusilp K (2013) Developmental program:educating families to support the mother in breastfeeding in the maternity ward Srinagarind Hospital, Faculty of Medicine, Khon Kaen University. Srinagarind Medical Journal 28.
- Rotjananirankit N, Naromrum K (2012) The effect of clinical nursing practice guideline on breastfeeding promotion. Thai J Nurs 61.
- Budsaengdee B (2014) Self- efficacy promotion on success in exclusive breast feeding among cesarean section mother. Thai Red Cross Nursing Journal 7.
- Panyim K, Kantaruksa K (2012) Effectiveness of implementing best practice guidelines for breastfeeding promotion, Phobphra hospital, Tak province. Nursing Journal 39.
- Paiboonbunpot N (2015) The effects of breastfeeding promotion program towards knowledge attitude and skill on breastfeeding among postpartum mothers. Journal of Nursing Science and Health 38.
- Yantaporn C, Rattasumpun P, Pakdevong N (2012) Effects of enhancing self-efficacy program on nurses��? self-efficacy and breastfeeding promotion behavior. Journal of Nursing and Health Care 30.
- Yuangthong S, Sawatphanit W, Deoisres W (2012) The effect of breastfeeding promoting program for first-time postpartum mothers on breastfeeding duration and behaviors. The Public health Journal of Burpha University 7.
- Boonjan J, Pathumwiwatana P, Chouwajaroen P, Chusilp K (2011) Development of services for promoting sustainable breastfeeding. Journal of Nursing and Health Care 29.
- Puapornpong P, Raungrongmorakot K, Hamontri S, Ketsuwan S, Wongin S (2015) Comparison of exclusive breastfeeding rate at six months postpartum between hospital personnel and general women. Journal of Medicine and Health Sciences 22.
- Sinthukot P, Jirapaet V (2014) Effects of breastfeeding empowerment program on maternal self-efficacy, maternal milk supply and change of body. Journal of Nursing Science Chulalongkorn University 26.
- Yimyam S. (2013) Breastfeeding promotion among outside employed mothers. Nursing Journal 40.
- Thongpanya K (2009) Breastfeeding promotion project for family. Khon Kaen university, Thailand.
- Visanpun P (2008) The result of breastfeeding promotion program to the exclusive breastfeeding rate and duration of mother who are working woman. Mahidol university, Thailand.
- Kupratakul J, Taneepanichskul S, Voramongkol N, Phupong V (2010) A randomized controlled trial of knowledge sharing practice with empowerment strategies in pregnant women to improve exclusive breastfeeding during the first six months postpartum. J Med Assoc Thai 93: 1009-1018.
- Ngerncham S, Laohapensang M, Wongvisutdhi T, Ritjaroen Y, Painpichan N, et al. (2013) Lingual frenulum and effect on breastfeeding in Thai newborn infants. Paediatr Int Child Health 33.
- Radwan H (2013) Patterns and determinants of breasrfeeding and complementaty feeding practices of Emirati Mothers in the United Arab Emirates. BMC Public Health 13: 1-11.
- Nduna T, Marais D, Wyk VB (2015) An explorative qualitative study of experiences and challenges to exclusive breastfeeding among mothers in rural Zimbabwe. Infant Child and Adolescent Nutrition 7: 69-76.
- Kounnavong S, Gorstein PS, Akkhavong K, Palaniappan U, Berdaga V, et al. (2013) Key determinants of optimal breastfeeding practices in Laos. Food and Nutrition Sciences 4: 61-70.
- Tan LK (2011) Factors associated with exclusive breastfeeding among infants under six months of age in peninsular Malaysia. Int Breastfeed J 6.
- Ahmad M, Sughra U, Kalsoom U, Imran M, Hadi U (2012) Effect of antenatal counselling on exclusive breastfeeding. J Ayub Med Coll Abbottabad 24: 116-118.
- Kim DT, Chapman SR (2013) Knowledge, attitude and practice about exclusive breastfeeding among women in chililab in Chi Linh Town, Hai Duong province,Vietnam. Journal of Health Research 27: 39-44.
- Bansal CP (2013) Breastfeeding- why are we still failing? National President, Indian Academy of Pediatrics 50: 993-994.
- Ali S, Ali FS, Imam MA, Ayub S, Billoo GA (2011) Perception and practices of breastfeeding of infants 0-6 months in an urban and a semi-urban community in Pakistan: A cross-sectional study. J Pak Med Assoc 61: 99-104.
- Desai A, Mbuya NNM, Chigumira A, Chasekwa B, Humphrey HJ, Moulton HL, et al. (2014) Traditional oral remedies and perceived breast milk insufficiency are major barriers to exclusive breastfeeding in rural Zimbabwe. J Nutr 144: 1113-1119.
- Otoo GE, Lartey AA, Pérez-Escamilla R (2009) Perceived incentives and barriers to exclusive breastfeeding among Periurban Ghanaian women. Journal of Human Lactation 25: 34-41.
- Nankunda J, Tumwine J, Soltvedt A, Semiyaga N, Ndeezi G, et al. (2006) Community based peer counsellors for support of exclusive breastfeeding: experiences from rural Uganda. Int Breastfeed J 1:19.
- Xu F, Binns C, Zheng S, Wang Y, Zhao Y, et al. (2007) Determinants of exclusive breastfeeding duration in Xinjiang, PR China. Asia Pac J Clin Nutr 16: 316-321.
- Murray S, Tredoux S, Viljoen L, Herselman MG, Marais D (2008) Consumer testing of the preliminary paediatric food-based dietary guidelines (PFBDG) among mothers with infants younger than 6 months in selected urban and rural areas in the Western Cape. South Afr J Clin Nutr 21.
- Guerrero ML, Morrow RC, Calva JJ, Ortega-Gallegos H, Weller SC, et al. (1999) Rapid ethnographic assessment of breastfeeding practices in periurban Mexico City. Bull World Health Organ 77: 323-330.
- Chen CY, Wu CY, Chie CW (2006) Effects of work-related factors on the breastfeeding behavior of working mothers in a Taiwanese semiconductor manufacturer: A cross-sectional survey. BMC Public Health 6: 160.
- Fjeld E, Siziya S, Katepa-Bwalya M, Kankasa C, Moland KM, et al. (2008) No sister, the breast alone is not enough for my baby' a qualitative assessment of potentials and barriers in the promotion of exclusive breastfeeding in southern Zambia. Int Breastfeed J 3: 1-12.
- Kamudoni P, Maleta K, Shi Z, De-Paoli M, Holmboe-Ottesen G (2010) Breastfeeding perceptions in communities in Mangochi district in Malawi. ActaPædiatrica 99: 367-372.
- Bansal CP (2013) Breastfeeding- why are we still failing? National President, Indian Academy of Pediatrics 50: 993-994.
- Kermani MR, Nedaeifard L, Tehrani AM, Nateghi RM, Fazeli SA (2012) Pattern of breastfeeding in infants conceived by assisted reproductive techniques at royal institute from birth to 6 months in Tehran-Iran. J Family Reprod Health 3: 105-109.
- Alemayehu T, Haider J, Habte D (2009) Determinants of exclusive breastfeeding practices in Ethiopia. Ethiopian Journal of Health Development 23: 12-18.
Relevant Topics
- Chronic Disease Management
- Community Based Nursing
- Community Health Assessment
- Community Health Nursing Care
- Community Nursing
- Community Nursing Care
- Community Nursing Diagnosis
- Community Nursing Intervention
- Core Functions Of Public Health Nursing
- Epidemiology
- Epidemiology in community nursing
- Health education
- Health Equity
- Health Promotion
- History Of Public Health Nursing
- Nursing Public Health
- Public Health Nursing
- Risk Factors And Burnout And Public Health Nursing
- Risk Factors and Burnout and Public Health Nursing
Recommended Journals
- Epidemiology journal
- Global Journal of Nursing & Forensic Studies
- Global Nursing & Forensic Studies Journal
- global journal of nursing & forensic studies
- journal of community medicine& health education
- journal of community medicine& health education
- Palliative Care & Medicine journal
- journal of pregnancy and child health
Article Tools
Article Usage
- Total views: 11626
- [From(publication date):
February-2017 - Dec 11, 2024] - Breakdown by view type
- HTML page views : 10452
- PDF downloads : 1174