Research Article Open Access
Exploring Patterns in Referrals to Combat Stress for Uk Veterans with Mental Health Difficulties between 1994 and 2014
Murphy D1,2,*, Weijers B3, Palmer E4, Busuttil W5
1Lecturer in Clinical Psychology, Combat Stress, Leatherhead, UK
2King’s Centre for Military Health Research, Department of Psychological Medicine, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
3Senior Data Analyst, Combat Stress, Leatherhead, UK
4Research Assistant, Combat Stress, Leatherhead, UK
5Clinical Director, Combat Stress, Leatherhead, UK
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
Little is known about the patterns of help-seeking in UK veterans with mental health difficulties. The aim of this study was to explore referral patterns to Combat Stress over a 20 year period. Combat Stress is a national mental health charity that offers support to UK ex-service personnel. Data was extracted from an electronic patient database system that included information on referrals to Combat Stress between 1994 and 2014. Data included time since leaving the Forces, area of deployment and whether participants engaged in clinical services. A fourfold increase in the number of referrals received each year over the duration of the study period was observed. Ex-service personnel who had served in Northern Ireland made up the largest proportion of helpseekers. In recent years significant increases in referrals from veterans from Iraq and Afghanistan were noted. Over the study period the time it took for participants to seek help after they left the services reduced by a half. There has been a recent sharp increase in veterans seeking support for mental health difficulties. This may reflect a period effect with individuals more willing to seek help sooner now than in the past. For example, veterans from Iraq and Afghanistan are seeking help more quickly than veterans from previous conflicts. The data presented within this paper suggests that there will continue to be an increase in the numbers of veterans seeking support for mental health difficulties over the coming years.
Keywords
PTSD, Military, Veterans, Ex-service personnel, Referral rates, Help-seeking
INTRODUCTION
Following the operational duties in Iraq and Afghanistan since 2003 there has been an increase in the amount of research monitoring the mental health of military personnel (Sundin et al., 2014; Riddle et al., 2007; Hoge, Auchterlonie, & Milliken, 2006; Hoge et al., 2004; Hotopf et al., 2006; Iversen et al., 2009; Fear et al., 2010). As a result of an ongoing epidemiological study of military personnel in the UK we now have a clearer picture of the prevalence rates of mental health difficulties within this population. These studies reported consistent rates over two waves of data collection of common mental health difficulties to be approximately 20% and post-traumatic stress disorder (PTSD) to be 4% (Fear et al., 2010; Hotopf et al., 2006).
What is known?
The UK Armed Forces has a turnover of approximately 10% each year meaning that large numbers of individuals who will have served during these conflicts will now have left and become veterans (Defence Analytical Services Agency, 2008). In the UK a veteran is defined as an individual who served at least one day in the UK Armed Forces (Dandeker, Iversen, Ross, & Wessely, 2006). It has been estimated that there are 3.8 million veterans living in the UK but that this number is expected to decline in the coming years as veterans from World War Two pass away (Woodhead et al., 2009). Analysis of the 2007 UK Adult Psychiatric Morbidity study reported no significant differences in the mental health of veterans compared to non-veterans in the UK (Woodhead et al., 2011). However, analyses comparing still serving military personnel and the general working population observed that military personnel were twice as likely to report common mental health difficulties (Goodwin et al., 2015). Further, veterans have been shown to have experienced higher levels of both childhood adversity and trauma in adulthood than nonveterans (Woodhead et al., 2011).
Whilst research in the UK has focused on epidemiological surveys to understand representative population data of military personnel, less is known about the rates of help-seeking for mental health difficulties within veteran populations (Iversen et al., 2011; Iversen et al., 2010). Differences in prevalence rates of mental health difficulties between help-seeking veterans and the wider veteran population have been noted. For example, as mentioned above rates of depression and PTSD in the veteran population have been observed to be 20% and 4% respectively (Fear et al., 2010), compared to 80% and 73% within a help-seeking population (Murphy, Palmer, Busuttil, & Oddy, 2015). Research studies have reported significant time intervals between veterans leaving the military and seeking help for military-related trauma with on average 11 years passing between leaving the military and seeking support (Murphy et al., 2015; van Hoorn et al., 2013). In addition, it has been observed that only approximately 20% of veterans with a mental health difficulty seek support (Iversen et al., 2010). Such a disparity between mental health difficulties and help-seeking implies a large number of veterans who may require treatment are not receiving it, highlighting a need to further explore patterns of help-seeking.
Aims
The aim of this paper was to explore the changing nature of referrals to Combat Stress (CS) over the last two decades. In particular, to explore if there has been an increase in rates of ex-service personnel seeking help, whether there have been changes in the time interval between leaving the Forces and seeking help and to elucidate which deployments help-seekers had served on over this time period. This is the first study of its kind in the UK to explore patterns of referrals for veterans with mental difficulties over a significant period of time.
METHODS
Data Access Point
Combat Stress was established in 1919 after the end of the First World War to support veterans who were experiencing mental health difficulties. Today it is the UK’s largest charity providing clinical mental health services to veterans, and since 2011 has been funded by the NHS to provide a national specialist PTSD clinical service (Murphy et al., 2015). The charity offers national support through community outreach teams and specialist treatment for PTSD at three residential treatment centres across the UK. Referrals to CS can come from a variety of sources including self-referrals, from other charities and via the NHS (for instance via GPs or community mental health teams).
Participants
For this paper we created a dataset that included unique contacts from veterans between 1994 and 2014. In the case of a veteran being referred to CS several times over this period of time we defined a unique contact as the first time a veteran was referred and subsequent referrals were excluded from the dataset. Following a referral to CS, veterans were assessed to ascertain their level of clinical need and whether they wished to engage with CS. Where there was evidence of a mental health difficulty and the veterans chose to engage with CS they were deemed active and offered clinical services.
Measures
Data included within the electronic patient records system included referral dates, demographics, whether individuals became active with CS after their initial assessment, information on where individuals had deployed during their military careers and when they had left the military. A new variable was constructed that recorded length of time between leaving the Armed Forces and seeking help from CS.
Analysis
A dataset was derived by doing data extracts from CS’s patient records system. As part of this veterans were assigned a code to signify their first year of contact, which deployments they had served on and when they had left the military. These variables were then used during the analysis. The analysis for this paper consisted of using plots to explore changes in the patterns of referrals over the 20 year period and answer the research questions set out for this study. The first stage of the analysis was to plot the number of unique referrals to CS by year between 1994 and 2014. For subsequent analyses we restricted the dataset to only those individuals who choose to engage with CS. The reason for this was because the aim of the above analysis was to provide information on referral rates whilst the next stage of the analysis was to explore different patterns within those veterans that were assessed as having a mental health difficulty and then engaged with the clinical services offered by CS.
The number of participants who became active each year between 1994 and 2014 stratified by area of deployment was plotted. It was decided to restrict the analysis to only individuals who had deployed to Northern Ireland, the Falklands War, the 1991 Gulf War, the peace-keeping operations to the Balkans, operations to Iraq since 2003 and operations to Afghanistan since 2001. This was to ensure that any conflicts with numbers too low to be analysed or any non-deployed personnel were not included in this analysis. It is important to note that participants could have deployed to several operations. Where this occurred they were included in both operations. Following this the average number of years that had passed between participants leaving the military and seeking help from CS for each year between 1994 and 2014 was plotted. The final stage of the analysis was to repeat this but stratified by area of operational deployment. All analyses were conducted using Stata 13 (StataCorp, College Station, TX).
Ethical approval
Ethical approval for this project was granted by the CS ethics committee.
RESULTS
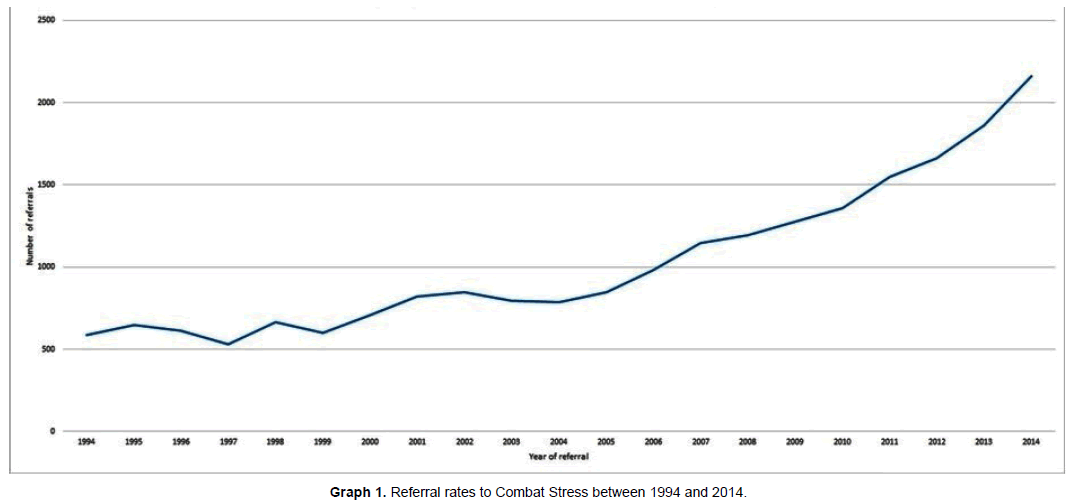
In total there were 21,651 unique referrals to CS between 1994 and 2014. Of these 13,746 individuals became active and engaged in clinical services with CS. Graph 1 reported the number of referrals each year over the two decade data collection period. An increase in numbers of referrals to CS was observed over this time period. For example in 1994, 588 referrals were received compared to 788 in 2004 and 2,163 in 2014. The slope of the graph suggests that referral rates steadily increased until 2005 and then started to rise more rapidly following this date. In general, no differences in terms of socio-demographic characteristics and areas of deployment were observed between the different CS sites across the UK.
The vast majority of the sample was male (98%) and this remained consisted over the course of the study period. The mean age of individuals within the study was 44.1 years old. There was some evidence that the mean age that veterans was seeking help was reducing over period of the study from 53.8 years in 1994 to 42.2 years in 2014. In total 53% of the sample were single (this includes those who were widowed) and this rate had increased from 41% in 1994 to 53% by 2014. Similarly, changes in employment status were noted with 29% of veterans employed in 1994, increasing to 53% in 2014 (overall rate was 45%). The mean length of service was 10.4 years and this remained roughly consistent over the study period. The mean numbers of deployments individuals had served was 1.58 and there is a suggestion of a modest increase in this over the 20 years, from 1.12 deployments for individuals referred in 1994 increasing to 1.76 deployments for those referred in 2014.
Graph 2 shows the theatre of deployment of participants who became active in CS's clinical services over the data collection time period. Veterans who had deployed to peace-keeping duties to Northern Ireland were the largest group and the numbers being referred who have deployed to Northern Ireland have increased over time. Different patterns of referrals were observed between individuals who had deployed to either Iraq since 2003 or Afghanistan. The slope of the Iraq veterans showed a steady increase from 2003 onwards at the beginning of the conflict. In contrast, the slope of veterans deployed to Afghanistan appeared to remain relatively low from the beginning of the conflict in 2001 until 2008. Subsequently, the rate of Afghanistan veterans being referred to CS has increased and overtook those from Iraq in 2011. The reported increase equates to 104 individuals in 2010, 219 in 2012 and 443 in 2014. More modest increases over time were observed in the number of veterans deployed to the Falklands War and the 1991 Gulf War. Interestingly, there appears to be a steady rise in those deployed to all six of the different operational deployments with the largest increases in the last few years being veterans from Afghanistan and Iraq. It is important to note the difference in numbers may reflect the differences between the total numbers of military personnel involved in each conflict. For example, Northern Ireland veterans make up the largest proportion of referrals as these deployments involved the largest number of military personnel over the longest period of time.
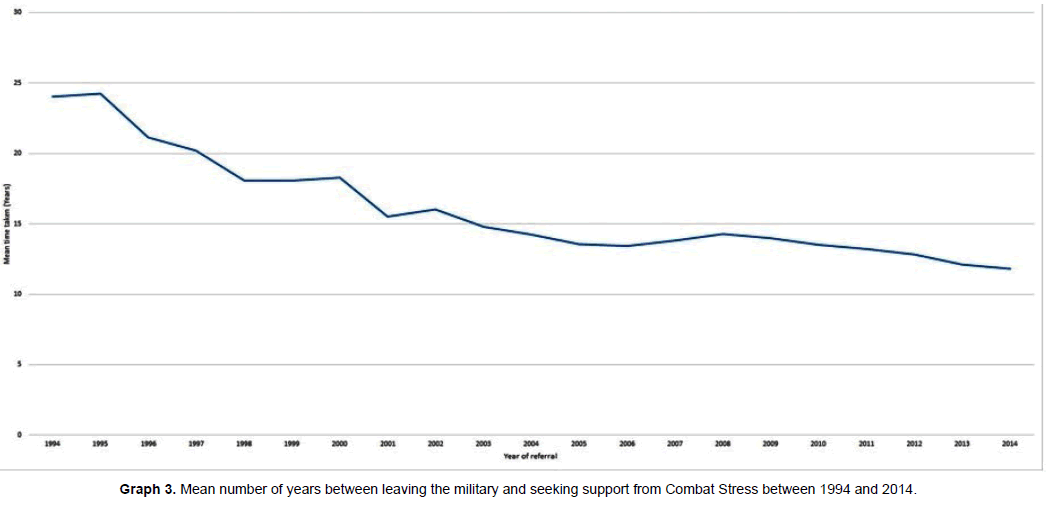
Graph 3 shows that as time has passed there has been a decrease in the number of years between individuals leaving service and seeking help. In 1994 the average time interval between leaving service and seeking help for service-related mental health difficulties within this population was 24.0 years. By 2004 this had reduced to 14.3 years and by 2014 to 11.8 years. This analysis was repeated but stratified by area of deployment in Table 1. The data in table one show marked differences in the time it took for participants to seek help. For example, individuals who had deployed to Northern Ireland and the Falkland War took the longest times to seek help whilst veterans from Afghanistan and Iraq have sought help much sooner. There seems to a general trend that veterans of more recent operations have sought help sooner than their peers from previous conflicts. For example, deployments to Falklands War, and in general to Northern Ireland, took place longer ago than operations to the 1991 Gulf war or the mid 1990s operations during the Balkans conflict and the conflicts in Iraq and Afghanistan that began in 2003 and 2001 respectively, and as mentioned above, veterans from these more recent conflicts are seeking support more quickly.
| Area of deployment | Number of ever active veterans | Mean number of years |
|---|---|---|
| Afghanistan since 2001 | 1470 | 2.0 |
| Iraq since 2003 | 2198 | 3.3 |
| Balkans conflict | 1985 | 5.8 |
| 1991 Gulf War | 1618 | 8.7 |
| Falklands War | 1242 | 14.9 |
| Operations to Northern Ireland | 6707 | 13.3 |
Table 1: Mean number of years between leaving the UK military and being referred.
DISCUSSION
The main findings from this study are that the number of veterans seeking help for mental health difficulties appears to have dramatically increased over the last two decades. There appears to be evidence of a period effect with veterans accessing services more quickly now than in the past.
The data presented demonstrate that the number of new referrals each year to CS have increased nearly fourfold between 1994 and 2014. Veterans who had deployed to Northern Ireland make up the largest proportion of help-seeking veterans. This is perhaps not surprising given that deployments to Northern Ireland would have had the largest commitment of military personnel. Whilst data is not available it has been estimated that during the 1970’s approximately 21,000 UK troops were deploying to Northern Ireland each year. This figure reduced during the 1980’s and is estimated to have been around 10,000 troops each year. In contrast approximately 53,450 UK military personnel have been estimated to have deployed during the 1991 Gulf war (Ministry of Defence, 2000), 150,000 from the start of the conflict in Iraq in 2003 until May 2011 and 139,000 from the start of the conflict in Afghanistan until October 2014 (Defence Analytical Services Agency, 2015). These figures give an estimate of the relative sizes of the veteran populations to each of these conflicts. The data shows that in recent years there has been an increase in number of veterans seeking help who had deployed to Iraq since 2003 and Afghanistan since 2001. A steady increase in referrals of Iraq veterans was observed starting from the beginning of operational duties in 2003. This contrasts with referrals from Afghanistan which were low for the first five years of the conflict and then increased sharply around 2009. Referrals for veterans who had been on operations to Afghanistan have increased sharply and they are now the second largest group seeking support from CS.
Differences in referral patterns
The differences in fatality rates between these operations could be hypothesised to explain some of the reasons behind the referral patterns. The number of British service personnel killed in Iraq was substantial from the beginning of the conflict, whilst fatality rates were low in Afghanistan between 2001 and 2005 (between zero and three service personnel killed each year) and then increased to 39 individuals in 2006 and peaked at 108 individuals in 2009 (Ministry of Defence, 2015b; Ministry of Defence, 2015a). Previous research of historical conflicts have demonstrated a clear link between the number of service personnel killed during a conflict and rates of mental illness (Jones & Wessely, 2001).
Differences between UK and US rates of mental health difficulties
Evidence has been presented that suggests a trend of increasing rates of help-seeking from UK veterans with mental health difficulties. This raises the question, does this imply there has been an increase in prevalence rates of mental health difficulties within the population? Studies of US service personnel deployed to Iraq and Afghanistan have suggested a trend to increased rates of PTSD as time since deployment has increased (Hoge et al., 2007; Hoge et al., 2004; Bliese et al., 2007; Cabrera et al., 2007; Vasterling, Proctor, & Friedman, 2010). However, a different pattern has emerged in the UK. As mentioned above, an ongoing epidemiological survey of serving and ex-serving UK military personnel has reported that there has not been an increase in rates of mental health difficulties when the authors reported findings from the first wave in 2006 and the second wave in 2010. The above study was setup in 2003 following the invasion of Iraq which means that limited data exists on rates of mental health difficulties within veterans that were on operations prior to this. Taking the above evidence, and focusing on just the UK veterans in our sample who had deployed to Afghanistan and Iraq, it could be suggested that the increase in referral rates to CS is not an increase in prevalence rates of mental health difficulties in the UK veteran population, but rather an increased awareness of services or an increased willingness for those with difficulties to access services.
Explanations for increases in rates of help-seeking
Increased reporting about PTSD by the media (Coggins, 2013) and initiatives from mental health organisations could have increased awareness of services. Since 2007 CS has significantly increased its awareness campaigns to discuss the issue of PTSD for veterans and available treatment options. For example, in 2007 CS launched a media campaign directed at veterans from the Falklands conflict and subsequently, as reported within the current study, saw an increase in Falkland’s war veterans seeking support from 59 in 2006 to 94 in 2007.
The current study has reported that the time it takes veterans to seek help has reduced from 24.0 years to 11.8 years between 1994 and 2014. In particular, it appears that veterans from the more recent conflicts; for example the operations to Afghanistan and Iraq, are accessing services sooner than their peers from previous deployments. As mentioned above, over the last decade there has been an increase in media reporting about the possible impact of deployment on veterans' mental health and awareness campaigns by service charities and mental health organisations about the importance of seeking support for difficulties which may explain some of the positive reduction in the amount of time it takes veterans to seek support. In addition, there have been a number of initiatives by the UK Defence Mental Health Services to promote help-seeking and tackle stigma within active members of the British military. For example, these included introducing a period of decompression for personnel that were returning from tours of Iraq or Afghanistan. Decompression involved military personnel stopping off in Cyprus for two days after the end of deployment to give them time to adjust before returning home. Decompression activities included a focus on increasing awareness and reducing stigma about mental health (Hughes et al., 2008; Burdett et al., 2011). Further, Trauma Risk Management (commonly referred to as TRiM) has been introduced across the military services, an initiative with the aim of tackling stigma and promoting help-seeking for mental health difficulties through peer support (Greenberg et al., 2010). These initiatives could have contributed to an increase in awareness of help available and gone some way to tackling stigma-related barriers to seeking help.
The role of stigma in the Armed Forces
There is evidence to suggest that during World War Two stigmatising beliefs towards mental health were encouraged. For example the term ‘lack of moral fibre’ was used to discourage members of the Royal Air Force to refuse to take part in operations (Jones, 2006). Whilst views have clearly changed towards mental illness, studies have demonstrated the continuing presence of stigma. It has been observed that military leaders viewed soldiers with mental health difficulties more negatively than those without (Porter & Johnson, 1994) or that leaving deployment due to mental illness greatly increased the chances of leaving the military via an early discharge (Jones et al., 2010).
The relationship of stigma in the Armed Forces is complicated by the military culture that places an emphasis on psychological resilience (Rona et al., 2004; Vogt, 2011). For example, it has been observed that soldiers are more likely to attend appointments for physical health problems than appointments for mental health difficulties (French, 2005). Given the suggestions above about the impact of stigma, it is positive that the current paper reports increased numbers of veterans seem to be accessing support, and that they are doing so sooner than their peers from previous generations.
Similarities with the general public
An increase in referrals to mental health services without an accompanying increase, or only modest increase, in rates of mental illness has also been noted with the general public in England.
Results from the Adult Psychiatric Morbidity Household surveys over a similar time period have observed only modest increases in the prevalence rates of mental health difficulties within the general public in England. For example, observed rates of individuals who meet criteria for at least one common mental health disorder were 15.5% in 1993, 17.5% in 2000 and 17.6% in 2007 (Jenkins et al., 1997; Singleton et al., 2001; McManus et al., 2009). Whilst restricted to 2005 onwards, data has been reported by NHS England that demonstrates a year on year increase in the numbers of individuals who have accessed mental health services in England (NHS England, 2015). For example 1,149,472 individuals accessed support in 2005 and this increased to 1,727,641 by 2014 (NHS England, 2015). Taken together this could also suggest that whilst the rates of mental illness have only increased modestly, there has been a greater increase in the number of individuals accessing support, reflecting a similar trend as found in the current study in the general population.
LIMITATIONS
This study has a number of limitations that need to be considered. Information on diagnosis was not recorded in the electronic patient records system that CS used over this time period. As such, whilst the referral data provides information on the numbers seeking support for mental health difficulties we have been unable to comment on the severity or range of mental health presentations individuals were referred for. Information of diagnosis is now collected and this will allow us to conduct future analyses to explore patterns of referrals in more detail. The sample for this study was drawn from participants who had sought support from CS. No information was available about veteran referral patterns to the NHS over this time period and no information was recorded on whether individuals had accessed other services for support prior to CS. As such, whilst the current study provides insights into the changing rates of referral patterns to CS, the conclusions drawn from the data may not generalise to the wider help-seeking veteran population. Replicating this study for other national veterans charities that provide different types of care (for example those supporting welfare needs) would allow us to build up a more detailed picture of the changing needs of veterans, beyond mental health.
CONCLUSIONS
This study represents an important step in understanding the changing nature of help-seeking in UK veterans over the last 20 years and may provide valuable information for understanding the services that may be needed by veterans in the future. Overall veterans from Northern Ireland continue to make up the largest proportion of help-seekers. The results of this study show that there has been an increase in demand for support for mental health difficulties from CS with a sharp increase in the numbers veterans from the conflicts in Iraq and Afghanistan being referred in recent years. The data suggests a period effect with individuals being referred more quickly now that in the past. Whilst this trend was apparent for all veterans, it was particularly apparent in veterans from Iraq and Afghanistan who appear to be seeking support more quickly than peers from previous deployments. The data presented within this paper suggests that over the coming years there will continue to be an upward trend in the numbers of UK veterans seeking support for mental health difficulties which may need careful planning for. UK veterans appear to be seeking support sooner now than in the past which provides evidence for the success of anti-stigma campaigns. This implies that the UK Armed Forces and veterans’ charities should continue to support existing, and evolve new, strategies to encourage this difficult to engage population to seeking help mental health difficulties. However, given the limitations of this study, more information is needed about referral rates of veterans to the NHS and other mental health organisations before firm conclusions can be drawn.
References
- Bliese, P.D., Wright, K.M., Adler, A., Thomas, J., & Hoge, C. (2007). Timing of postcombat mental health assessment. Psychiatric Services, 4, 141-148
- Burdett, H., Jones, N., Fear, N. T., Wessely, S., & Greenberg, N. (2011). Early psychosocial intervention following operational deployment: analysis of a free text questionnaire response. Military Medicine, 176(6), 620-625
- Cabrera, O., Hoge, C., Bliese, P.D., Castro, C., & Messer, S.C. (2007). Childhood adversity and combat as predictors of depression and post-traumatic stress disorder in deployed troops. American Journal of Preventive Medicine, 33, 77-82
- Coggins, J. (2013). The agonizing face of war: Soldiers with PTSD make disturbing masks to express their feelings of horror and frustration. The Daily Mail. Retrieved from http://www.dailymail.co.uk/news/article-2331265/The-scars-battle-Soldiers-suffering-PTSD-make-chilling-face-masks-feelings.html
- Dandeker, C., Iversen, A., Ross, J., & Wessely, S. (2006). "What is a veteran?". Armed Forces and Society, 32, 161-177
- Defence Analytical Services Agency. (2008). DASA Outflow Statistics
- Defence Analytical Services Agency. (2015). Freedom of information requestion: military commitment on Op Telic and Op Herricj London: Ministry of Defence
- Fear, N.T., Jones M., Murphy, D., Hull, L., Iversen, A., Coker, B. et al. (2010). What are the consequences of deployment to Iraq and Afghanistan on the mental health of the UK armed forces? A cohort study. Lancet, 375(9728), 1783-1797
- French, C. (2005). Post discharge mentoring for vulnerable service leavers London: Ministry of Defence
- Goodwin, L., Wessely, S., Hotopf, M., Jones, N., Greenberg, N., Rona, R. et al. (2015). Are common mental disorders more prevalent in the UK serving military compared to the general working population? Psychological Medicine, 21, 1-11
- Greenberg, N., Langston, V., Everitt, B., Iversen, A., Fear, N.T., Jones, N. et al. (2010). A cluster randomized controlled trial to determine the efficacy of Trauma Risk Management (TRiM) in a military population. Journal of Traumatic Stress.22(1)()(pp 11-19), 2009.Date of Publication: 2009., 23(4), 430-436
- Hoge, C., Terhakopian, A., Castro, C., Messer, S.C., & Engel, C.C. (2007). Association of posttraumatic stress disorder with somatic symptoms, health case visits, and absenteeism among Iraq war veterans. American Journal of Psychiatry, 164, 150-153
- Hoge, C.W., Auchterlonie, J.L., & Milliken, C.S. (2006). Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. Journal of the American Medical Association, 295(9), 1023-1032
- Hoge, C.W., Castro, C.A., Messer, S.C., McGurk, D., Cotting, D.I., & Koffman, R.L. (2004). Combat Duty in Iraq and Afghanistan, Mental Health Problems, and Barriers to Care. The New England Journal of Medicine, Vol.351(1), 13-22
- Hotopf, M., Hull, L., Fear, N.T., Browne, T., Horn, O., Iversen, A. et al. (2006). The health of UK military personnel who deployed to the 2003 Iraq war: a cohort study. Lancet, 367(9524), 1731-1741
- Hughes, J.H., Earnshaw, M., Greenberg, N., Eldridge, R., Fear, N.T., French, C. et al. (2008). Use of psychological decompression in military operational environments. Military Medicine, 173(6), 534-538
- Iversen, A.C., van, S.L., Hughes, J.H., Browne, T., Greenberg, N., Hotopf, M. et al. (2010). Help-seeking and receipt of treatment among UK service personnel. British Journal of Psychiatry., 197(3), 149-155
- Iversen, A.C., van, S.L., Hughes, J.H., Browne, T., Hull, L., Hall, J. et al. (2009). The prevalence of common mental disorders and PTSD in the UK military: using data from a clinical interview-based study. BMC psychiatry.9 (pp 68), 2009
- Iversen, A.C., van, S.L., Hughes, J.H., Greenberg, N., Hotopf, M., Rona, R.J., et al. (2011). The stigma of mental health problems and other barriers to care in the UK Armed Forces. BMC Health Services Research, 11, 31
- Jenkins, R., Lewis, G., Bebbington, P., Brugha, T., Farrell, M., Gill, B., et al. (1997). The National Psychiatric Morbidity Surveys of Great Britain initial findings from the Household Survey. Psychological Medicine, 27, 775-789
- Jones, E. (2006). 'LMF': The use of psychiatric stigma in the Royal Air Force during the Second World War. The Journal of Military History, 70, 439-458
- Jones, E., & Wessely, S. (2001). Psychiatric battle casualties: an intra- and interwar comparison. British Journal of Psychiatry, 178, 242-247
- Jones, N., Fear, N.T., Jones, M., Wessely, S., & Greenberg, N. (2010). Long-Term Military Work Outcomes in Soldiers Who Become Mental Health Casualties When Deployed on Operations. Psychiatry, 73(4), 352-364
- McManus, S., Meltzer, H., Brugha, T., Bebbington, P., & Jenkins, R. (2009). Adult psychiatric morbidity in England, 2007: Results of a household survey London, UK: The Health & Social Care Information Centre, Social Care Statistics
- Ministry of Defence. (2015a). British fatalities: operations in Iraq. MOD, UK. Retrieved from https://www.gov.uk/government/fields-of-operation/iraq
- Ministry of Defence. (2015b). Op Herrick casualty and fatality tables: up to 2015. MOD, UK. Retrieved from https://www.gov.uk/government/statistics/op-herrick-casualty-and-fatality-tables-2015
- Ministry of Defence. (2000). 1990/1991 Gulf Conflict London: Ministry of Defence
- Murphy, D., Hodgman, G., Carson, C., Spencer-Harper, L., Hinton, M., Wessely, S. et al. (2015). Mental health and functional impairment outcomes following a six week intensive treatment programme for UK military veterans with post traumatic stress disorder (PTSD): a naturalistic study to explore dropout and health outcomes at follow-up. BMJ Open, 5
- Murphy, D., Palmer, E., Busuttil, W., & Oddy, M. (2015). Exploring the prevalence of traumatic brain injury (TBI) and associations between TBI and mental health difficulties within UK veterans accessing support for mental health difficulties. In prep
- NHS England. (2015). MHMDS: Mental Health Minimum Dataset: online statistics 2005/2014. Health and Social Information Centre Mental Health Minimum Data Set Annual Returns. Retrieved from http://www.mhmdsonline.ic.nhs.uk/
- Porter, T.L., & Johnson, W.B. (1994). Psychiatric stigma in the military. Military Medicine.159(9):602-5
- Riddle, J.R., Smith, T.C., Smith, B., Corbeil, T.E., Engel, C.C., Wells, T.S. et al. (2007). Millennium Cohort: The 2001-2003 baseline prevalence of mental disorders in the U.S. military. Journal of Clinical Epidemiology, 60(2), 192-201
- Rona, R.J., Jones, M., French, C., Hooper, R., & Wessely, S. (2004). Screening for physical and psychological illness in the British Armed Forces: I: The acceptability of the programme. Journal of Medical Screening, 11(3), 148-152
- Singleton, N., Bumpstead, R., O'Brien, M., Lee, A., & Meltzer, H. (2001). Psychiatric morbidity among adults living in private households, 2000 London, UK: Social Survey Division of the Office for National Statistics
- Sundin, J., Herrell, R., Hoge, C., Fear, N., Adler, A., Greenberg, N. et al. (2014). Mental health outcomes in US and UK military personnel returning from Iraq. The British Journal of Psychiatry.
- van Hoorn, L., Jones, N., Busuttil, W., Fear, N., Wessely, S., Hunt, E. et al. (2013). Iraq and Afghanistan veteran presentations to Combat Stress since 2003. Occupational Psychiatry, 63(3), 238-241
- Vasterling, J.J., Proctor, S.P., & Friedman, M.J. (2010). PTSD symptom increases in Iraq-deployed soldiers: comparison with nondeployed soldiers and associations with baseline symptoms, deployment experiences, and postdeployment stress. Journal of Traumatic Stress.22(1)()(pp 11-19), 2009.Date of Publication: 2009., 23, 41-51
- Vogt, D. (2011). Mental health-related beliefs as a barrier to service use for military personnel and veterans: A review. Psychiatric Services, 62(2), 135-142
- Woodhead, C., Rona, R., Iversen, A., MacManus, D., Hotopf, M., Dean, K. et al. (2011). Mental health and health service use among post-national service veterans: results from the 2007 Adult Psychiatric Morbidity Survey of England. Psychological Medicine, 41(363), 372. Woodhead, C., Sloggett, A., Bray, I., Bradbury, J., McManus, S., Meltzer, H. et al. (2009). An estimate of the veteran population in England: based on data from the 2007 Adult Psychiatric Morbidity Survey. Population Trends, 138, 50-54.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 14289
- [From(publication date):
September-2015 - Jul 11, 2025] - Breakdown by view type
- HTML page views : 9591
- PDF downloads : 4698