Exploration on the Clinical Effect of Different Autotransfusion Methods on Patients with Femoral Shaft Fracture Surgery
Received: 02-Sep-2021 / Accepted Date: 13-Sep-2021 / Published Date: 20-Oct-2021 DOI: 10.4172/1165-158X.1000213
Abstract
Objective: To explore the clinical effect of predeposit, salvage and hemodilution autotransfusion on patients with Femoral Shaft Fractdure (FSF) surgery. Methods: Selected FSF patients were randomly divided into 3 groups: intraoperative blood salvage autotransfusion group, preoperative hemodilution autohemotransfusion group and predeposit autotransfusion. After the operation for 5 days, body temperature, heart rate, blood platelet (PLT) and Hemoglobin (Hb) of patients were determined; the concentrations of EPO and G-MSF in the 3 groups were calculated by ELISA assay; the content of CD14+ monocytes were calculated by FCM assay. The growth time and condition of the patient’s callus were determined at the 30th, 45th and 60th days after operation. Cox regression analysis was used to analyze the correlation between EP0, G-MSF, CD14+ mononuclear content, callus growth and autotransfusion methods.
Results: There were no statistically significant differences in body temperature and heart rate between the 3 groups (P >0.05). PLT and Hb in Predeposit group were markedly increased compared to that in Salvage group and Hemodilution group. The concentrations of EPO and G-MSF in Predeposit group were markedly increased compared to that in Salvage group and Hemodilution group. The content of CD14+ monocytes in Predeposit group was significantly higher compared to that in Salvage group and Hemodilution group. Predeposit autotransfusion promotes callus growth more quickly. The concentration of EP0 and G-MSF were positively correlated with callus growth in the three groups, and the content of CD14+ monocytes was not correlated in any of the three groups.
Conclusion: Predeposit autotransfusion promoted the recovery of FSF patients after operation more quickly compared to salvage autotransfusion and hemodilution autotransfusion.
Keywords: Femoral Shaft Fractdure (FSF), Autotransfusion, Predeposit, Salvage, Hemodilution
Introduction
Femoral Shaft Fracture (FSF) is a common disease in orthopedic trauma [1]. With the development of society and the development of transportation industry, the incidence of FSF has increased [2]. Blood loss in patients with FSF is common, not only in the operative and postoperative stages, but also in the early stage after the fracture [3]. Acute blood loss can lead to hemorrhagic anemia. Anemia is an independent risk factor for adverse outcomes in patients with FSF, including an increased risk of death 3 months after surgery and an increased risk of death 1 year after surgery. In addition, anemia is also detrimental to the early postoperative functional activities of patients, and even indirectly affects the treatment effect of surgery [4]. Transfusion is a common method to treat anemia in patients with FSF. There are some restricting factors in clinical blood transfusion [3,5]. Blood supply is insufficient in some countries, costs a lot and also has a bad effect on patients.
Anemia and blood transfusion were associated with adverse outcomes [6]. Researchers continue to explore the best methods to improve patients’ clinical outcomes. In recent years, due to the spread of blood transfusion diseases, especially hepatitis and AIDS after transfusion, autotransfusion has risen to an important position [7]. Autotransfusion is a simple, effective and safe way of transfusion, which is easy to be popularized in clinic [8]. Autotransfusion includes 3 kinds of way: predeposit, salvage and hemodilution. Salvage autotransfusion is a blood transfusion method in which the blood from intraoperative bleeding or postoperative wound drainage is recycled, anticoagulant, filtered, washed and concentrated by the blood recovery device and then returned to the patient. Predeposit autotransfusion is to collect the patient’s own blood for preservation, and then give it back to the patient when the patient needs blood transfusion, so as to ensure the use of blood for treatment. Hemodilution autotransfusion is to reduce the concentration of blood cells in unit volume of blood by supplementing crystal fluid or colloidal fluid after anesthesia and before surgery [9,10]. In the case of the same amount of blood loss, the loss of blood cells is significantly reduced. The researchers believe that the main effects of postoperative blood transfusion on the body are immunosuppression, inflammatory effect and bone marrow hematopoiesis.
This study focused on the transfusion of patients with FSF after surgery. The clinical recovery characteristics of patients were compared by three methods: predeposit transfusion, salvage transfusion and hemodilution transfusion, including the recovery time of vital signs was stable, and callus growth at 30, 45 and 60 days after the operation site. In addition, hematopoietic related factors EPO and G-MSF of the patients were analyzed, and the proportion of CD14+ monocytes in the patients was analyzed.
Materials and Methods
Patients and grouping
A total of 60 patients with FSF requiring surgery were collected from Shandong Provincial Hospital during April, 2008 to May, 2010. The inclusion criteria for FSF patients were: patients undergoing elective orthopedic surgery; ASAⅠ-Ⅱ grade; male; age from 20 to 50 years old; the estimated operative blood loss was >600ml; preoperative hemoglobin (Hb) ≥ 110g/L, hematocrit (Hct) ≥ 35% and platelet (PLT) count ≥ 100 × 109/L. The exclusion criteria were: patient who was suffering from malignant tumor, abnormal blood coagulation before operation, accompanied by cerebrovascular disease, venous thrombosis of lower limbs before operation, abnormal function of heart, liver, kidney, lung and other important organ systems.
The selected 60 FSF patients were randomly divided into three groups: Predeposit, Salvage and Hemodilution group. After surgery for 3-7 days, measurements or blood analysis are taken to assess the patient’s physical recovery (body temperature, heart rate, platelet count and hemoglobin count); levels of erythropoietin (EPO), granulocytemacrophage colony-stimulating factor (GM-CSF) in the patient’s blood were determined by ELISA; levels of CD14+ monocytes in the blood of the patients were analyzed by flow cytometry. Follow-up visits were conducted 30, 45 and 60 days after the operation to analyze the growth time and condition of callus.
Enzyme-Linked Immunosorbent Assay (ELISA)
Due to the availability of material, the levels of EPO and G-MSF were measured by ELISA in undiluted plasma samples. Commercially available ELISA kits for EPO and G-MSF (BD Biosciences, San Jose, CA) were applied based on the manufacturers’ instructions. Results were read at an optical density of 450 nm using a Spectra Max Plus plate reader (Molecular Devices, Sunnyvale, CA). Measurements were performed in duplicate, and p-values were computed using the twosided Student t-test (p <0.05).
Flow Cytometry (FCM)
The content of CD14+ monocytes in blood of patients was determined by FCM. A tube was taken as the control by adding CD14- FITC and Mouse-IgG1-APC, and the other tube was added CD14-FITC and TLR2-APC. After mixing, tubes were stored at 4ºC for 20 minutes in dark, and then 2 ml erythrocyte lysate was added, shaked well and let them stand at room temperature for 10 minutes. Lysate was centrifuged at 1500 r/min for 7 min and the sediment was washed by PBS. At last, PBS was added and the solution was mixed fully. BD FACSA via flow cytometry was used for detection. The relative content of CD14+ was expressed by mean fluorescence index.
Statistical analysis
Logistic multi-factor regression analysis was used to analyze the correlation between EP0, G-MSF, content of CD14+ mononuclear cells, callus growth and blood transfusion mode. All statistical tests were two-sided, and statistical significance was defined as p <0.05.
Results
Autotransfusion methods affect body recovery of patients
The observed indicators for patient’s physical recovery, including body temperature, heart rate, blood platelet (PLT) and hemoglobin (Hb), were determined after the operation for 5 days. As Table 1 showed there were no statistically significant differences in body temperature and heart rate between groups (P >0.05). PLT and Hb in Predeposit group were markedly increased compared to that in Salvage group and Hemodilution group (P <0.05). Those indicated Predeposit autotransfusion was the most conducive to the recovery of various indicators.
| Method | Temperature (°C) | Heart rate (bpm) | PLT (× 109/L) | Hb (g/L) |
|---|---|---|---|---|
| Salvage | 36.90 | 91.23 | 146.36 | 96.04 |
| Hemodilution | 36.84 | 91.62 | 145.24 | 98.52 |
| Predeposit | 36.87 | 90.02 | 154.88 | 107.34 |
Table 1: Observed indicators of patients in 3 groups after operation for 5 days
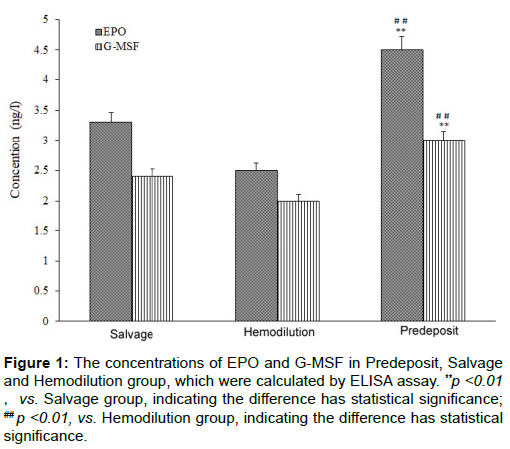
Predeposit autotransfusion increases the content of EPO and G-MSF
The concentrations of EPO and G-MSF in Predeposit, Salvage and Hemodilution group were calculated by ELISA assay. Results were showed in Figure 1. As shown, the concentrations of EPO and G-MSF in Predeposit group were markedly increased compared to that in Salvage group and Hemodilution group (P <0.01). Moreover, there had no significant differences of EPO and G-MSF concentrations between Salvage group and Hemodilution group (P >0.05).
Figure 1: The concentrations of EPO and G-MSF in Predeposit, Salvage and Hemodilution group, which were calculated by ELISA assay. **p <0.01,vs. Salvage group, indicating the difference has statistical significance; ## p <0.01, vs. Hemodilution group, indicating the difference has statistical significance.
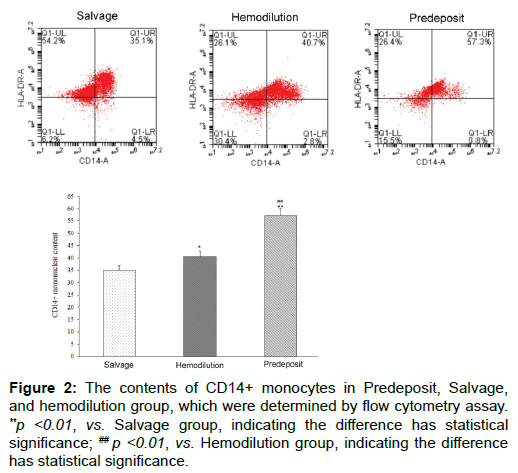
Determination on content of CD14+ monocytes
The content of CD14+ monocytes in Predeposit, Salvage and Hemodilution group were calculated by FCM assay. As Figure 2 showed, the content of CD14+ monocytes in Salvage group was 35.1%, in Hemodilution group was 40.7% and in Predeposit group was 57.3%. The differences of content between Hemodilution group and Predeposit group, Salvage group and Predeposit group were statistically significant (P <0.01). The difference between Hemodilution group and Salvage group was not statistically significant (P >0.05).
Figure 2: The contents of CD14+ monocytes in Predeposit, Salvage, and hemodilution group, which were determined by flow cytometry assay. **p <0.01, vs. Salvage group, indicating the difference has statistical
significance; ## p <0.01, vs. Hemodilution group, indicating the difference has statistical significance.
Predeposit transfusion promotes callus growth more
The growth time and condition of the patient’s callus were determined at the 30th, 45th and 60th days after operation. Results were showed in Table 2. As shown, the callus in Salvage group and Hemodilution group at the 30th was 0 mm, while the callus in Predeposit group was 2-3 mm. At the 45th days, callus in Salvage group, Hemodilution group and Predeposit group was 2-5, 2-4 and 3-6 mm, respectively. At the 60th days, callus in Salvage group, Hemodilution group and Predeposit group was 5-8, 5-6 and 6-10 mm, respectively. Those indicated Predeposit transfusion promotes callus growth more quickly.
| Method | 30 days | 45 days | 60 days |
|---|---|---|---|
| Salvage | 0 | 2-5 mm | 5-8 mm |
| Hemodilution | 0 | 2-4 mm | 5-6 mm |
| Predeposit | 2-3 mm | 3-6 mm | 6-10 mm |
Table 2: Growth time and condition of the patient’s callus in 3 groups.
Correlation analysis
Logistic multi-factor regression analysis was used to analyze the correlation between EP0, G-MSF, CD14+ mononuclear content, callus growth and transfusion methods, so as to evaluate the advantages and disadvantages of the three transfusion methods. Results were showed in Tables 3 and 4. As shown, the concentration of EPO and G-MSF were positively correlated with callus growth in the three groups, and they had a significant relationship with Predeposit transfusion. In addition, the content of CD14+ monocytes was not correlated in any of the three groups.
| Method | Χ2 | P value | OR | 95% CI |
|---|---|---|---|---|
| EPO | 4.975 | 0.001 | 0.315 | [1.023, 3.152] |
| G-MSF | 5.064 | 0.022 | 1.217 | [1.082, 3.534] |
Table 3: Relevance between EPO, G-MSF and callus growth.
| Method | Χ2 | P value | OR | 95% CI |
|---|---|---|---|---|
| EPO | 3.278 | 0.015 | 1.954 | [1.080, 3.489] |
| G-MSF | 4.272 | 0.021 | 2.573 | [1.286, 6.830] |
| CD14+ | 0.521 | 0.106 | 0.956 | [0.628, 1.854] |
Table 4: Relevance between EPO, G-MSF, CD14+ mononuclear content and transfusion methods.
Discussion
In recent years, the increasing number of orthopedic surgery patients further increased the demand for blood. At present, allogeneic transfusion is mainly used to supplement patients’ blood in orthopedic surgery, but allogeneic transfusion should consider the situation of blood-borne diseases and shortage of blood resources [11]. Autotransfusion can not only avoid the side effect of allogeneic transfusion and eliminate the risk of disease transmission, but also stimulate the hematopoietic function of bone marrow, so that the hematopoietic speed of patients after surgery is accelerated [12,13]. Autotransfusion not only alleviates the shortage of blood source, but also saves the medical expenses of patients, which is a safe and effective method [14]. Hemodilution transfusion can solve the problem of blood supply for patients with rare blood type [15]. Salvage transfusion can supply fully compatible blood of the same type.
Our study showed PLT and Hb in Predeposit group were markedly increased compared to that in Salvage group and Hemodilution group, which indicated Predeposit transfusion, was the most conducive to the recovery of various indicators. Platelets contain a variety of autologous growth factors, including Platelet-Derived Growth Factor (PDGF), Insulin-Like Growth Factor (IGF), as well as growth factor for hepatocytes [16]. Hypoxemia has been recognized as a risk factor for bone loss [17]. It predicts long-term survival in dialysis patients [18]. Then, we calculated the concentrations of EPO and G-MSF in Predeposit, Salvage and Hemodilution group by ELISA assay. Results showed concentrations of EPO and G-MSF in Predeposit group were markedly increased compared to that in Salvage group and Hemodilution group. EPO is a hormone that stimulates the production of new red blood cells [19]. It can regulate the proliferation and differentiation of erythroid cells [20]. It is tissue-protective in preclinical models of ischemic, traumatic, toxic, and inflammatory injuries [21]. It has been demonstrated to stimulate fracture healing [22]. GM-CSF is a powerful growth and differentiation factor which acts on hematopoietic progenitor cells and also activates differentiated granulocytes and macrophages [23]. It can govern the functions of granulocyte and macrophage lineage populations at all stages of maturation [24]. Results of FCM showed the content of CD14+ monocytes in Storage group was markedly higher than that in Salvage and Hemodilution group. Human CD14+ monocytes can differentiate into monocytederived macrophages (MDMs) or dendritic cells (MoDCs) upon suitable stimulation [25]. Moreover, our study also found Predeposit autotransfusion promotes callus growth more quickly compared to salvage and hemodilution autotransfusion. Fracture healing presents a sequence of three major stages: inflammation and granulation tissue formation, callus formation and remodeling [26]. Callus formation and growth are an essential part of secondary fracture healing [27]. Cox regression analysis also showed the concentration of EP0 and G-MSF were positively correlated with callus growth in the three groups, and they had a significant relationship with Predeposit autotransfusion.
Conclusion
In conclusion, predeposit autotransfusion promoted the recovery of FSF patients after operation more quickly compared to salvage autotransfusion and hemodilution autotransfusion, which indicated predeposit autotransfusion was more suitable to FSF patients.
Acknowledgement
This work is supported by Key Disciplines Group Construction Project of Pudong Health Bureau of Shanghai (No. PWZxq2017-10) and National Natural Science Foundation of China (No. 81870147). We would like to acknowledge the reviewers for their helpful comments on this paper.
Interest of Conflict
All of the authors have no conflict of interest in this research.
Ethics, Consent and Permissions
Ethical approval was given by the Shanghai Gongli Hospital, the Naval Military Medical University and written informed consent was obtained from all patients.
References
- Park-Wyllie, L.Y., Mamdani , M. M., Juurlink , D. N., Hawker, G. A., Gunraj, N., Austin, P. C., et al. Bisphosphonate use and the risk of subtrochanteric or femoral shaft fractures in older women. JAMA., 2011;305(8): 783-789
- Weiss, R.J., Montgomery, S. M., Al Dabbagh, Z., & Karl-Ake, J. National data of 6409 Swedish inpatients with femoral shaft fractures: Stable incidence between 1998 and 2004. Injury., 2009;40(3): 304-308
- Kobbe, P., Micansky , F., Lichte, P., Sellei, R. M., Pfeifer, R., Dombroski, D., et al. Increased morbidity and mortality after bilateral femoral shaft fractures: Myth or reality in the era of damage control Injury., 2013;44(2): 221-225
- Haghighi, M., Ettehad, H., Mardani-Kivi , M., Mirbolook, A., Nabi, B. N., Moghaddam, R., et al. Does tranexamic acid reduce bleeding during femoral fracture operation? Arch Bone Jt Surg., 2017;5(2): 103-108
- Gadegone, W.M., & Salphale, Y.S. Short proximal femoral nail fixation for trochanteric fractures. J Orthop Surg., 2010;18(1): 39-44
- Bateman, S.T., Lacroix, J., Boven, K., Forbes, P., Barton, R., Thomas, N. J., et al. Anemia, blood loss, and blood transfusions in North American children in the intensive care unit. Am J Respir Crit Care Med., 2008;178(1): 26-33
- Baumann, C., Lamesic, G., Weiss, M., Cushing, M. M., & Haas, T. Evaluation of the minimum volume of salvage blood required for the successful use of two different autotransfusion devices. Paediatr Anaesth., 2015;25(3): 258-264
- Robinson, L. Systems and methods for salvaging red blood cells for autotransfusion. nGoogle Patents., 2015.
- Biesel, W. Method and apparatus for processing intra-or postoperative blood loss for autotransfusion. Google Patents., 2001.
- De Vroege, R., Wildevuur, W. R., Muradin, J. A. G., Graves, D., & van Oeveren, W. Washing of stored red blood cells by an autotransfusion device before transfusion. Vox Sang., 2007;92(2): 130-135
- Kanda, M., Kobayashi, D., Tanaka, C., Iwata, N., Yamada, S., Fujii, T., et al., Adverse prognostic impact of perioperative allogeneic transfusion on patients with stage II/III gastric cancer. Gastric Cancer., 2016;19(1): 255-263
- Huang, X. Comparison of effects of allogeneic blood transfusion and hemodiluted autotransfusion on cellular immune function in patients undergoing cesarean section. Chinese J Anesthesiol., 2016;36(2): 199-202
- Ji, W., Lin, X., Zhang, R., Tang, P., Mo, J., Teng, X., et al. Application of postoperative autotransfusion in total joint arthroplasty reduces allogeneic blood requirements: a meta-analysis of randomized controlled trials. BMC Musculoskelet Disord., 2017;18(1): 378
- Catmull, S.P., & Ashurst, J.V. Autotransfusion, in StatPearls [Internet]. nStatPearls Publishing., 2019.
- Jilmaâ€Stohlawetz, P., Wreford-Bush, T., Mills, F., Davidson, F., Kursten, F. W., Jilma, B., et al., Falseâ€positive pregnancy test after transfusion of solvent/detergentâ€treated plasma. Transfusion., 2017;57(12): 2965-2968
- Weibrich, G., Hansen, T., Kleis, W., Buch, R., & Hitzler, W. E. Effect of platelet concentration in platelet-rich plasma on peri-implant bone regeneration. Bone., 2004;34(4): 665-671
- Cesari, M., Pahor, M., Lauretani, F., Penninx, B., W., H., J., Bartali, B., Russo, R., et al., Bone density and hemoglobin levels in older persons: results from the InCHIANTI study. Osteoporos Int., 2005;16(6): 691-699
- Avram, M. M., Blaustein, D., Fein, P. A., Goel, N., Chattopadhyay, J., & Mittman, N. Hemoglobin predicts long-term survival in dialysis patients: A 15-year single-center longitudinal study and a correlation trend between prealbumin and hemoglobin: Management of comorbidities in kidney disease in the 21st century: Anemia and bone disease. Kidney Int Suppl., 2003;64: S6-S11
- Lasne, F., & de Ceaurriz, J. Recombinant erythropoietin in urine. Nature., 2000;405(6787): 635-635
- Jaquet, K., Krause, K., Tawakol-Khodai, M., Geidel, S., & Karl-Heinz, K. Erythropoietin and VEGF exhibit equal angiogenic potential. Microvas Res., 2002;64(2): 326-333
- Brines, M., Grasso, G., Fiordaliso, F., Sfacteria, A., Ghezzi, P., Fratelli, M., et al., Erythropoietin mediates tissue protection through an erythropoietin and common β-subunit heteroreceptor. Proc Natl Acad Sci., 2004;101(41): 14907-14912
- Garcia, P., Speidel, V., Scheuer, C., Laschke, M. W., Holstein, J. H., Histing, T. et al., Low dose erythropoietin stimulates bone healing in mice. J Orthop Res., 2011;29(2): 165-172
- Uchida, K., Beck, D. C., Yamamoto, T., Pierre-Yves, B., Abe, S., Staudt, M. K., et al., GM-CSF autoantibodies and neutrophil dysfunction in pulmonary alveolar proteinosis. N Engl J Med., 2007;356(6): 567-579
- Hamilton, J.A., GM-CSF in inflammation and autoimmunity. Trends Immunol., 2002;23(8): 403-408
- Lin, Y.F., Horng-Mo, L., Sy-Jye, L., & Yu-Hui, T. The essentiality of PKCα and PKCβI translocation for CD14+ monocyte differentiation towards macrophages and dendritic cells, respectively. J Cell Biochem., 2007;102(2): 429-441
- Rozen, N., Lewinson, D., Bick, T., Jacob, Z. C., Stein, H., & Soudry, M. Fracture repair: Modulation of fracture-callus and mechanical properties by sequential application of IL-6 following PTH 1–34 or PTH 28–48. Bone., 2007;41(3): 437-445
- Eastaugh-Waring, S., Joslin, C. C., Hardy, J. R. W., & Cunningham, J. L. Quantification of fracture healing from radiographs using the maximum callus index. Clin Orthop Relat Res., 2009;467(8): 1986-1991
Citation: Wang H, Yin D, Wang J, Li Z, Xu J (2021) Exploration on the Clinical Effect of Different Autotransfusion Methods on Patients with Femoral Shaft Fracture Surgery. Cell Mol Biol 67: 213. DOI: 10.4172/1165-158X.1000213
Copyright: © 2021 Wang H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1833
- [From(publication date): 0-2021 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 1246
- PDF downloads: 587