Research Article Open Access
Exercise Intervention for Osteoporosis Prevention in Postmenopausal Women: A Systematic Review
Mishaal Al Khaldi*Senior Physical therapist, King Fahad Specialist Hospital, Dammam, Eastern Province, Saudi Arabia
- *Corresponding Author:
- Dr. Mishaal Al khaldi
Senior Physical therapist
King Fahad Specialist Hospital
Dammam, Eastern Province, Saudi Arabia
Tel: 00966555404862
E-mail: Mishaal.Alkhaldi1@hotmail.co.uk
Received date: November 11, 2016; Accepted date: December 19, 2016; Published date: December 26, 2016
Citation: Al Khaldi M (2016) Exercise Intervention for Osteoporosis Prevention in Postmenopausal Women: A Systematic Review. J Nov Physiother 7:323. doi: 10.4172/2165-7025.1000323
Copyright: © 2016 Al Khaldi M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
A varied exercise regimen is widely used to prevent osteoporosis in postmenopausal women, yet little is known about the most effective types of exercise, their frequency of use and the results of combining exercise with calcium and vitamin D. The aim of this review dissertation was to systematically review the evidence of the effectiveness of different types of exercise on bone mineral density in order to prevent osteoporosis in postmenopausal women.
A wide search was conducted to identify all the potential relevant randomised controlled trials using both electronic databases MEDLINE, CINAHL, PEDro, AMED, SPORTDiscus and ScienceDirect) and a manual search. The included trials were rated for risk of bias using the Jadad scale.
From an initial list of 524 potentially relevant studies, 27 randomised controlled trials of preventive exercise of osteoporosis in postmenopausal women with Bone Mineral Density (BMD) as an outcome measure were discussed in this review. A considerable number of the available trials had small sample size, high risk of bias, lack of long term follow-up.
The results suggest weight-bearing exercises are effective regardless of their duration, with or without calcium and vitamin D; non-weight bearing exercises might be effective but over a prolonged period of time and with calcium and vitamin D added. A combination of these exercises had positive effects on BMD when combined with HRT. Further, RCTs with a long-term follow up, a low risk of bias and larger sample sizes are needed in the future.
Keywords
Exercise; Post menopause; Osteoporosis; BMD
Background
Definition and incidence
A report on the current management of postmenopausal women with osteoporosis in the UK stated that over two million people in the UK alone are affected by osteoporosis, which is more than twice the number of people who suffer from dementia, one of the most common diseases in elderly. Annually, 300,000 people suffer fragility fractures and more than 70,000 of these occur at the hip joint causing disability, independency and, in some cases, can be a cause of death. Approximately 1,150 people die every month in the United Kingdom following a hip fracture.
According to the World Health Organization (WHO), osteoporosis is a condition characterized by a decrease of bone mass and morphology disorder, which consequently increases the susceptibility of bones to fracture [1]. This excessive loss of bone mass usually appears with increasing age [2] but, unfortunately, it often remains undiagnosed until a fracture occurs, which is why it has been called “a silent disease” [3].
Fragility bone fractures frequently occur at the same sites, mainly the spine, hip and wrist. Accordingly, osteoporosis is usually associated with functional impairments [4], which in turn reduces the quality of life [5]. Changes of bone structure due to this disease usually occur in bone microarchitecture, bone remodeling and the mineralization of micro-cracks [6].
Osteoporosis can be classified into either primary or secondary. The former is defined as a decrease of bone mass due to aging or hormonal changes, e.g. menopause. Secondary osteoporosis is caused by chronic medical conditions that contribute to bone remodelling, e.g. malignancy or gastrointestinal disease.
Pathogenesis
Bone strength arises from the integration of two main characteristics: bone density and bone quality. Bone homeostasis is a continuous process throughout life, which largely depends on the balance of the mechanical and biochemical environments. This process involves osteoblasts (“bone formation cells”) and osteoclasts (“bone absorption cells”), and these two stages must be balanced. Osteoporosis is caused when the reabsorption rate is higher than the formation rate, which might also be associated with incremental bone turnover. Bone loss begins after a person reaches their forties and, in the case of women, it increases more after the menopause (Table 1) [7].
Signs and symptoms
An early sign of osteoporosis is osteopenia, which is a condition where Bone Mineral Density (BMD) is lower than normal (between 1 and 2.5 Standard deviation is below the mean value for young people). Treating osteopenia may prevent the development of osteoporosis [8]. Fractures are one of the most significant signs of osteoporosis [9] and they usually happen as a result of a decrease in BMD, muscle strength and a balance disturbance as a consequence of osteoporosis.
Health-related quality of life has been shown to be decreasing with osteoporosis [10]. In fact, a study [11] observed that women with osteoporosis even without fractures have a lower quality of life than women who are healthy. This is basically due to its different impacts e.g., depression, impaired physical activity, chronic pain, poor wellbeing.
In some cases, patients with osteoporosis complain of a reduction in mobility, cramps and muscle weakness, joints and bone ache, a decrease in body height, frequent fractures and sometimes spontaneous fractures.
Risk factors of osteoporosis
Risk factors of osteoporosis can potentially change, but weight is frequently considered to be a relevant factor as obesity is usually accompanied with bone loss [12]. A second important factor is alcohol consumption Hannan et al. [12] determined in a study that elderly women who consume over 3oz and over 7oz of alcohol per week develop more severe bone loss at the trochanter site than women who consume less alcohol (0 to 1 oz/week).
Smoking has been shown to deter growth of osteoblasts and is a great risk factor of osteoporosis. It also plays a role in accelerating the menopause and decreasing body weight, which both contribute to bone loss. A greater level of bone loss in elderly women and men who smoke was noted compared to non-smokers in a Rotterdam study.
Nutrition is essential in maintaining good health and preventing disease, and a diet with sufficient levels of calcium and/or magnesium, phosphorus, iron, zinc, boron, copper, fluoride and vitamins “A, E and K” all help sustain good bone health [13]. The influence of nutrition may affect the bone health in several mechanisms, for example, by changing the rate of metabolism, affecting bone structure, paracrine and/or endocrine system [14]. Also, deficiency of vitamin D may lead to bone loss, high bone turnover and fractures [15].
Patients with Disability and mental retardation may develop low BMD due to low mobility. Some risk factors cannot be changed, such as advanced age or gender. Women are three times more prone to developing osteoporosis than men, due to their lower peak bone mass and the hormonal changes experienced during menopause. A deficiency of oestrogen can occur after natural menopause or an oophorectomy. A family history of osteoporosis may also increase the risk of developing osteoporosis. Ethnicity has also been described as an influencing factor, for example Europeans and Asians show a higher incidence of osteoporosis.
Impact of osteoporosis
Martin et al. [16] highlight some impacts that are known to be associated with osteoporosis, such as height loss, postural changes like kyphosis, and an increased difficulty of engaging in daily life activities [16].
Fractures are considered to be a serious consequence of osteoporosis and may have considerable implications; for example, there may be intolerable pain long-term complications, depression and low self-esteem due to the difficulty patients face in performing the tasks of daily living, any one of these factors, or a combination, can cause a decreased score on the Quality of Life (QoL) [11].
Diagnosis
Unfortunately, osteoporosis has no clear clinical manifestations [17] but bone fragility with fractures often leads to the diagnosis, and among those, vertebral compression fractures are common [17]. A wide range of techniques can be used to diagnose osteoporosis. The most commonly used technique and current gold standard is dualenergy x-ray absorptiometry, which will be discussed, among other approaches, in the following subsection [18].
Dual-energy x-ray absorptiometry (DXA): DXA has been known to be used to follow up patients with bone density loss and it is able to precisely measure BMD changes. A number of advantages of DXA are reported which are: its ability to predict the risk of fracture, short scan time and low radiation dose [19]. Binkley et al. [20] note some disadvantages including the fact that it cannot provide information about bone architectures and the effect of bone size on BMD [20].
Conventional radiography: Osteoporosis can be detected by normal radiography, but it has low sensitivity, so this is usually best carried out by observing certain features of osteoporosis such as deformities of the vertebrae caused by osteoporosis [21].
Calcaneal quantitative ultrasound (QUS): There is a rising interest in QUS as a bone loss screening tool for many reasons. Patients are not exposed to radiation and it has a low cost [22]. It is predicted to be commonly used to diagnose osteoporosis in the future (Table 2).
| Randomisation | Appropriate randomisation | Doubleblinding | Appropriate blinding | Withdrawals / dropouts | Total | |
| Weight-bearing | ||||||
| Preisinger et al.[46] | 1 | 0 | 0 | 0 | 0 | 1/5 |
| Prince et al.[56] | 1 | 1 | 0 | 0 | 0 | 2/5 |
| Going et al.[45] | 1 | 0 | 0 | 0 | 1 | 2/5 |
| Chan et al.[54] | 1 | 0 | 0 | 0 | 1 | 2/5 |
| Wu et al.[57] | 1 | 0 | 0 | 0 | 1 | 2/5 |
| Sakai et al.[55] | 1 | 0 | 0 | 0 | 1 | 2/5 |
| Non-weight bearing | ||||||
| Pruitt et al.[60] | 1 | 0 | 0 | 0 | 1 | 2/5 |
| Bemben et al.[42] | 1 | 0 | 0 | 0 | 0 | 1/5 |
| Kerr et al.[77] | 1 | 0 | 0 | 0 | 1 | 2/5 |
| Chilibeck et al.[47] | 1 | 0 | 0 | 0 | 1 | 2/5 |
| Cussler et al.[50] | 1 | 1 | 0 | 0 | 0 | 2/5 |
| Brentano | 1 | 0 | 0 | 0 | 0 | 1/5 |
| Bocalini et al.[59] | 1 | 0 | 0 | 0 | 1 | 2/5 |
| Chuin et al.[67] | 1 | 0 | 0 | 0 | 0 | 1/5 |
| Combination | ||||||
| Metcalfe et al.[49] | 1 | 0 | 0 | 0 | 1 | 2/5 |
| Milliken et al.[51] | 1 | 0 | 0 | 0 | 0 | 1/5 |
| Englund et al.[62] | 1 | 0 | 0 | 0 | 0 | 1/5 |
| Chubak et al.[48] | 1 | 1 | 0 | 0 | 0 | 2/5 |
| Korpelainen et al.[63] | 1 | 0 | 0 | 0 | 1 | 2/5 |
| Bolton et al. [53] |
1 | 1 | 0 | 0 | 1 | 3/5 |
| Chillibeck et al.[61] | 1 | 1 | 1 | 1 | 1 | 5/5 |
| WBV | ||||||
| Rubin et al.[69] | 1 | 1 | 1 | 1 | 0 | 4/5 |
| Verschueren et al.[66] | 1 | 1 | 0 | 0 | 0 | 2/5 |
| Beck and Norling.[64] | 1 | 0 | 0 | 0 | 1 | 2/5 |
| Von Stengel et al.[79] | 1 | 1 | 0 | 0 | 1 | 3/5 |
| Slatkovska et al.[65] | 1 | 1 | 0 | 0 | 1 | 3/5 |
Table 2: Risk of bias assessment.
Quantitative computed tomography (QCT): QCT has the ability to detect changes in trabecular and cortical bones, but it has a high cost and requires large-scale equipment which makes it impractical to use.
Prevention and treatment
The prevention and treatment of osteoporosis often needs various interventions. A pharmacological approach is common, as the medication to treat osteoporosis often works on the inhibition of bone reabsorption to maintain the Bone mineral density (BMD) e.g. oestrogen, calcitonin and bisphosphonates [23].
Although medication can help to maintain BMD, not all approaches are suitable for all people [8] and some medication has been reported to have severe side effects, for example, Hormonal Replacement Therapy (HRT). HRT has been widely used and evidently inhibits bone turnover and increases BMD [24]. A primary prevention trial of postmenopausal hormones, however, showed an increased risk of Coronary Heart Disease (CHD), breast cancer and pulmonary embolism in women who received oestrogen/progestin HRT.
Bisphosphonates have been reported to decrease the incidences of hip and spine fractures by 50% in postmenopausal women. However, they are not always recommended additionally as they might cause negative effects. A study of Bisphosphonates, was reported that it they may cause esophagitis, uveitis and myalgia [25].
Aside from medical approaches, the prevention of fractures caused by fragility has become a goal for intervention programmes in postmenopausal women with a special emphasis on exercise interventions. Physiotherapy should be one element of any osteoporosis prevention and treatment guideline [26]. During the last few decades physiotherapeutic intervention to prevent and treat osteoporosis has been focusing on either maintaining bone mass or reducing the risk of falls. Different approaches are used, for example, group exercises, hydrotherapy, body awareness and training [27]. Many of these techniques aim to strengthen bones by reducing disturbance in bone metabolism and to increase muscle power, and consequently eliminate pain and improve bone structure [27].
In terms of pain, several electrotherapy techniques have been used to influence the pain receptors and to eliminate pain where possible, e.g. direct current, low-frequency stimulation current , thermal techniques including short-wave thermic, ultrasound, red light, light thermic [27].
Exercises have been the most recommended technique used by physiotherapists following various case-control and observational studies. The mechanism of the exercises relies on systematic effects on the body by enhancing muscle strength, balance and body coordination [27].
Exercise helps prevent falls, by maintaining or increasing BMD, which in turn strengthens muscles and enhances balance. Also, it has the ability to influence the quality of life by modifying risk factors of falls, overcoming disabilities and perform daily living activity [28].
Introductions to the Dissertation
Existing evidence base
Weight-bearing exercises have been specifically recommended to prevent and manage osteoporosis in post-menopausal women. However, these guidelines do not specify the optimum mode of weight bearing exercises. On the other hand, some studies which did not meet the inclusion criteria for this review assessed the effects of weight-bearing training [29] and weight lifting [30]. This set of research shows that exercise is effective in improving muscle strength, but that no effect was found on BMD. These differing results might be due to a number of factors, for example, exercise responses are different for different people and can draw on many factors such as gender, age, and bone strength and oestrogen level. Also, the type and intensity of the given exercise may affect the benefits of the exercise [31].
Some trials have suggested that there are possible positive effects of resistance training on BMD [32-34]. Some strengthening exercises rely on a claim that states voluntary force exerted by muscles exposes great loads on the bones [35,36]. Resistance exercises have also been reported to maintain BMD [37] and shield bones against risk factors for fragile fractures in postmenopausal women with sedentary lifestyles.
A few trials have studied the effects of a combination of weightbearing and other types of exercise, e.g., strengthening [38]. They showed that a yearlong combined training programme has a positive effect on total hip BMD in postmenopausal women (45-65 years) with forearm fracture and low bone mass.
Martyn-St and Carroll [39] constructed a meta-systematic review and a meta-analysis to determine the efficacy of progressive highintensity resistance training on the BMD of postmenopausal women. Some subjects were already receiving hormone replacement therapy (HRT) and it was evident that resistance training is effective to maintain BMD at the LS (Lumbar Spine).
Lastly, Howe et al. [40] reviewed the literature to determine the effectiveness of exercises in general in the prevention of bone loss and fractures in postmenopausal women. Healthy subjects with previous fractures were considered in the inclusion criteria. It was found that it is still unclear as to what constitutes an optimal exercise programme to prevent osteoporosis.
In conclusion, still some controversies over the effectiveness of different exercise types in the prevention of osteoporosis and no optimum duration or frequency have been defined, therefore this dissertation will be a systematic review to identify suitable evidence to clarify these aspects.
Development altering the dissertation
Originally, this dissertation aimed to identify all the studies which discuss the effectiveness of weight-bearing exercise on preventing osteoporosis in postmenopausal women. After reviewing the literature, weight-bearing exercise is evident to be effective in the prevention of osteoporosis. The research question was revised after an a priori search to the following:
For postmenopausal women, do different types of exercises (weight bearing, non-weight bearing, a combination or whole body vibration) have different effects on Bone Mineral Density (BMD)?
Aims and hypotheses of the dissertation
The literature review indicates that most studies discuss the role of weight-bearing exercises to decrease bone fragility in women, as they are more prone to developing osteoporosis due to the hormonal changes following menopause.
Some reviews discuss exercise as a treatment of osteoporosis in postmenopausal women, some of which included exercises for both prevention and treatment of osteoporosis. No systematic review was found to compare different types of exercise regimens with postmenopausal women in the prevention of osteoporosis, therefore this systematic review was performed to evaluate the trials that assessed different exercise approaches to prevent osteoporosis in this population (postmenopausal women). Furthermore, as side aims this review attempted to determine the effective frequency of exercise per week, as well as the result of adding calcium and/or vitamin D to a regimen.
Methodology
Study design and search strategy
This is a systematic review of the evidence regarding different types of exercise regimens, the optimum frequency and duration of exercise and the provision of medical supplementation on BMD in postmenopausal women.
A comprehensive search was made to identify all the relevant trials using electronic databases. A manual search of journals was also conducted: Bone and Calcified Tissue International, Journal of Bone and Mineral Metabolism, Journal of Bone and Mineral Research, Osteoporosis International and Medicine and Science in Sports and Exercise.
The search was restricted to English- language articles due to the restriction of time and budget, and to avoid the possibility of bias during translation.
Electronic search: An electronic search was performed and the following databases were used to identify the potentially relevant articles: CINAHL from January 1995 to January 2013; AMED from 1995 to current. All searches were conducted in March 2013.The search history is summarised in Appendix 1.
Manual search: All available topic-related journals were checked (see Appendix 1). Titles and abstracts of the possibly relevant articles were screened to determine their eligibility (from January 1995 to 2013) on the official journal websites. Additionally, hand searching was continued in order to find more relevant articles by examining the references of each. Endnote web was used to remove the duplicates and for referencing.
Trials selection
Potential relevant articles identified in the search were assessed by the author for eligibility in this review according to the inclusion and exclusion criteria.
Non-randomized trials, or those which used a quasi-random assignment, were excluded, as they tend to have more bias [41]. Case series and case reports were not included due to the lack of comparability, absence of control data and because results usually cannot be generalized to a larger population.
Only peer-reviewed, full papers were included. Unpublished dissertations and theses, abstracts and conference papers were not included because of the dearth of data, plus an inability to find full data from the authors and the time and cost involved in retrieving such material.
Participants: Participants were healthy postmenopausal women without osteoporosis, regardless age, time since menopause, women either had a natural post-menopause or after a hysterectomy and/ or oophorectomy (surgical menopause). Women with diagnosed osteopenia were also considered, since treatment of osteopenia may prevent osteoporosis [8].
Trials were excluded if participants showed one of the following criteria
1) Subjects with osteoporosis or fractures due to bone loss;
2) Studies that included men;
3) Studies that included pre-menopausal women or both pre- and postmenopausal women;
4) Studies that included animals;
5) If all women in the sample were under hormone replacement therapy (HRT), i.e., no effect of exercise without HRT was tested;
6) Women in the control group were performing exercise effecting BMD;
7) Patients with breast cancer where the osteoporosis was caused by chemotherapy that affected bone formation, and not related to aging. (See appendix II).
Interventions: Included were any exercise interventions targeting BMD, including non-weight bearing exercise, e.g. resistance training, weight-bearing exercise or a combination of both weight-bearing and non-weight-bearing exercise, as well as vibration were considered.The exercise intervention duration had to be at least 6 months. Because it is known that the bone remodelling cycle is 4-6 months [42] this was the minimum duration of the included studies in this review.
If more than one intervention or a combination of medication with exercise was used (other than calcium) e.g. HRT or bisphosphonates, the exercise effect without medication had to be clearly assessed (See Appendix III).
Comparison: The review included RCTs of comparisons of the intervention against controls with no intervention, or against sham intervention e.g. stretching or exercise that does not have an impact on the primary study endpoints i.e. low intensity exercise not to affect BMD consequently; studies with controls participating in any intervention affecting BMD were excluded.
Trials with and without blinding were included. The studies had to present data at least two times, at baseline and after conclusion of the intervention, to assess immediate effects of the intervention.
Outcomes: The primary and only outcome in this review was described as the change in the Bone Mineral Density (BMD g/cm2). It may also be referred to as areal bone mineral density, which indicates the BMD for a certain body area, e.g. femur (Everyone Healthy, no date). BMD had to be measured by dual x-ray absorptiometry DXA (gold standard). Higgens and Green [41] claim that a restriction of outcome is not recommended, but the majority of the trials used BMD as the main outcome measure. BMD was specifically selected as an outcome measure for this review because it is the central element of any agreed definition of osteoporosis.
Trials that did not measure BMD, or used only quantitative computed tomography (QCT), were excluded because QCT is only able to measure pure trabecular bone [43], whereas DXA measures trabecular and cortical bone and is used as a reference measurement of BMD [44]. Some other bone parameters were measured in the included trials, but were not considered as an outcome measure in this review due to the variety of the outcomes measures used by every author, for instance frequency of falls. This might not be a good predictor of prevention of osteoporosis as it is more a consequence of osteoporosis and not used to diagnose or evaluate the development of the disease.
Assessment of risk of bias: Risk of bias was examined by using work as an assessment tool in this review. This is a three-item tool that was designed for quality assessment using two points for randomisation, two points for blinding, and only one point for reporting withdrawal/ dropout. All questions aimed to score 1 point for yes, or 0 for no, and the total score ranged from 0-5.
This tool has been reported to offer the most optimum validity and reliability of evidence and has been used in meta-analyses, e.g. by James and Carroll et al. [39]. Using a range of scores from, 0-2 refers to a high risk of bias, and 2-5 refers to a low risk of bias. All relevant studies were included regardless of their score using this quality assessment tool.
Results
Outcome of search strategy
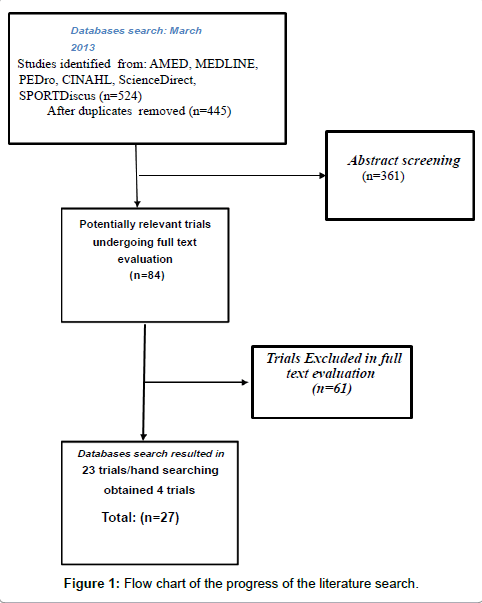
The electronic search of databases: AMED, CINAHL, MEDLINE, PEDro, SPORTDiscus and Science Direct, resulted in 524 trials, and after removing duplicates, 445 results remained. After screening the titles and abstracts (362 removed) and then checking the full texts, 61 were excluded according to the inclusion/exclusion criteria. A total of 23 trials resulted from the electronic search. The manual search of journals and a reference list of the trials and a related systematic review resulted in 4 trials. A total of 27 articles were included. A flow chart of the progress of the literature search is demonstrated in Figure 1.
Participants
Sample size: A total of 3,198 participants were included in this review. The sample sizes ranged from n=25 in Bemben et al. [42] to the largest sample size n=320 in Going et al. [45].
Years since menopause: All studies included women who were postmenopausal, but the time since menopause differed notably from women who were at least one year postmenopausal [46-48].
Age of the participants: In general all included trials used middle-aged and elderly women; however, some trials selected a range of ages starting from relatively young i.e. in the fourth decade [42,45,46,49,50,51].
Baseline characteristics: All the included studies were randomised controlled trials (RCTs) and therefore used one or more treatment groups and controls. Most of the intervention and control groups were similar in the baseline characteristics, except in eight studies.A difference of the age in the groups at baseline was mentioned in two studies. In Kerr et al. [52] participants in the control group were significantly older than those in the treatment groups. In Bolton et al. [53] the exercisers were 4.0 years older than the controls.
Interventions and comparisons
Four types of exercises are included in this review: weight bearing, non-weight bearing, combination and whole body vibration (WBV). A considerable number of the included trials used additional medication or supplements, or specifically tested an exercise as an adjunct to medication.
Effectiveness of Exercise intervention versus sham/control:
A) Weight bearing exercises: A total of 7 weight bearing trials were included, with various activities e.g. standing on one leg, walking, jogging, Tai Chai Chuan (TCC) and aerobic exercise. Participants in the intervention group were compared to controls with no intervention including no calcium/vitamin D or medications, in 3 studies [46,53-55].
In the study of Chan et al. [54] participants were either randomised to TCC or controls. Bone loss was found in both groups, but it occurred at a slower rate in the TCC group. Thus, TCC may have good effects to maintain BMD in postmenopausal women while in Preisinger et al. [46] and Sakai et al. [55] no major difference in terms of BMD at any site between groups was found. However, Preisinger et al. [46] subjects who exercised regularly in a programme that included brisk walking, jogging and complex exercise to train movement patterns adjusted to functional activities (diagonal or diagonal spiral movement), showed a lesser mean regression slope at proximal and distal forearm, which indicates the effects of exercises on BMD could be more beneficial with regular exercise.
Sakai et al. [55] intervention focused on uni-pedal standing for 1 minute on each leg, 3 sets a day, compared to controls with no exercise. There was no significant change in the BMD, however, when subjects were divided based on the age, subjects who were older than 70 showed a significant BMD increase at the hip compared to controls.
The rest of the weight bearing studies compared the exercise either with calcium/vitamin D alone or with some medications, controls with placebo or subjects with usual activity [56-58].
Prince et al. [56] main focus was to assess the effects of the calcium and also the effects of combining unspecified weight bearing exercises and walking with calcium, which had the greatest improvement of the BMD at the FN but not at any other body site. On the other hand, the placebo group showed a decrease of the BMD at all sites.
Loss of the BMD (p<0.02) in the control group was also observed by Going et al. [45] when they were compared to exercises in a group programme including aerobic and balance, weight bearing circuit, weight bearing modest impact activities with or without HRT, or HRT users alone. Improvement of the BMD was the highest in the trochanter in the exercisers only and interaction of exercise with HRT did not show any significant BMD improvement except in the total body BMD (p=0.052).
Combining walking or jogging on a treadmill and an Omega-3 supplement resulted in a significant increase of the BMD in the L2-L4 from baseline (p<0.05) [58]. However, exercise alone showed a slight improvement of the BMD at the same site. In contrast to Tartibian et al. [58] trial, a combination of walking with isoflavone did not show any interaction to change the BMD, neither in the exercise only or medication only groups nor the placebo group [57].
The results suggest that in several weight bearing studies, exercises were found better than with no intervention, but that was not consistent in all studies and all tested body areas. Exercise with additional supplements seemed to achieve better results than exercise alone with some products, while exercise interventions with HRT did not show significant improvements.
B) Non-weight bearing exercises: A total of 8 non-weight bearing studies have been conducted including various types of resistance and strengthening exercises with different intensities, same frequency of 3 times/week, and a large number of them supplied participants with calcium.
All the non-weight bearing trials assessed the effect of exercise alone against other interventions and controls except for one study [59]. Here, intervention was resistive exercise training and compared to controls who continued their usual activity. It was observed that women in the control group had a significant decrease of the BMD at the LS and FN (p<0.05) compared to non-significant bone loss at both sites in the exercise group.
Three studies assessed the effect of non-weight exercise interventions but with different adjustments against controls. Pruitt et al. [60] assessed high intensity (HI) and low intensity (LI) resistance training. The HI group started with a warm up of 1 set of 14 repetitions at intensity of 40% one-repetition maximum (1-RM), then performed 2 sets of 7 repetitions at 80% 1-RM, whereas, LI group performed 3 sets of 14 repetitions at 40% 1-RM.
The second study was by Bemben et al. [42] who determined high load (HL) and high repetition (HR) effects of non-weight bearing exercises where the HL group did 8 repetitions of each exercise at intensity of 80% of (1-RM), and the HR group did 16 repetitions of each exercise at 40% of 1-RM. While Pruitt et al. study, BMD was not improved significantly at any site in any group and there was no major loss of spinal BMD. Furthermore, proximal femur BMD improved slightly in the controls. Maintaining spine BMD was also noted in addition to hip in 2000.
Kerr et al. [52] examined the effects of two different types of exercise 1) strength, which targeted the skeletal loading; and, 2) fitness training, which targeted aerobic fitness and both groups performed the same exercises but the fitness group had minimal loads which remained constant over the study duration. The strength group in this study had a significant improvement of the BMD at the intertrochanteric site and total hip, while the fitness and control groups showed bone loss at the inter-trochanter, moreover, the total body BMD decreased in all groups.
The remaining non-weight bearing studies had more than two interventions by assessing the exercise, either alone or with medications, and also with controls, mainly comparing the exercise alone group, medications alone group, exercises+medications and placebo (control) group. Chilibeck et al. [61] examined the effects of the strength training exercise with or without bisphosphonates. Women in both the exercise and non-exercise group had a decrease of the BMD at the LS, but surprisingly, exercisers had more significant decrease than non-exercisers. Furthermore, no interactions of bisphosphonates and exercises were found at any site.
Cussler et al. [50] studied the effects of exercise with or without HRT. There was no change of the BMD in any group, although there was a non-significant increase from the baseline of the strength training group (STG), and there was a non-significant decrease of the BMD in the Circuit Training Group (CTG) in Cussler et al. [50] where half of the participants received HRT and participants were divided into four groups by the HRT status [62-66]. These groups were: 1) HRT+exercise, 2) HRT, no exercise, 3) no HRT+exercise, 4) no HRT, no exercise control group. The strengthening exercise focused on the relationship between the BMD change and the weight lifted, which was calculated for each specific exercise to find out the most improvement of the BMD at the greater trochanter, which was associated with an SD unit of change of total weight lifted.
Finally, the exercise effects with or without antioxidants were tested in the trial of Chuin et al. [67] where subjects performed a resistance training programme. The control group were given a placebo drug with no exercise and had a significant BMD loss at the LS (p<0.05).However, BMD was maintained in the other groups.
In general, non-weight bearing studies focused on comparing the effects of the exercises alone or with various medications. Only Kerr et al. [52] appeared to find significant changes in BMD at total hip and intertrochanter in the strength training group. Most of the interventions showed either no significant improvement or a decrease of the BMD.
C) Combination exercises: A total of 7 trials used a combination of weight bearing and non-weight bearing exercises, that included a variety of exercise regimens such as, moderate intense exercise, resistance training, aerobic, progressive weight bearing etc. The majority of the combination of exercises RCTs compared the intervention of combination exercises only with control groups. Controls were given no exercise intervention except in one study where the control group was given a stretching exercise as sham [48].
Two trials assessed the exercise effects alone or with medications [51,61]. Milliken et al. [51] assessed the effects of aerobic and resistance training with or without HRT and controls with no intervention. The effects of the exercise when it was combined with HRT were significant in the greater trochanter (p=0.03) while women in the exercise group alone had a significant increase on the BMD of the Ward’s triangle. A non-significant decrease in the BMD at all sites in the control group was reported. Chilibeck et al. [61] determined the effects of the weight training combined with walking with or without isoflavone. All groups in this study had a decline in the BMD, however, exercise+isoflavone had a greater decrease of the BMD at two sites; total hip and trochanter than exercise alone, showing no main effect of the exercise.
The remaining trials compared the effects of the exercise against controls with no intervention. In one trial [49] the exercise group performed progressive weight bearing, resistance exercise with small and large muscle groups, abdominal strengthening, stretching and balance exercise, and showed significant increase of the BMD at two sites: the femur and spine, compared to controls. Two studies found small improvements of the BMD. Englund et al. [62] reported improvement of the BMD at the Ward’s triangle in the exercise group who received a combination of aerobic, balance, coordination and strengthening, while there was a decrease in the controls. Additionally, a major increase was noted in different sites: arms, LS and trochanter in the exercises compared to the controls. Similarly, Bolton et al. [53] showed a slight improvement of the hip BMD in the exercise group including moderate intense exercise and resistance training compared to bone loss in the controls.
Korpelainen et al. [63] found that a combination of jumping and balance exercises rendered no significant change of the BMD at any site, in both exercise and control groups. Controls had no intervention.
D) Whole body vibration (WBV): Six studies included subjects exposed to the whole body vibration, two of these were combined with strengthening training with subjects standing on the platforms. Three of the WBV studies had more than one variation of the WBV intervention, either by giving two different frequencies [64,65] or by providing two different WBV protocols.
While a significant bone loss at the trochanter and LS was reported in the control group by Beck and Norling [64], BMD slightly decreased in both WBV groups (High frequency=2 × 3 minutes, 12.5 Hz, 1 g, low frequency=15 minutes, 30 Hz, 0.3 g). The group that received high frequency WBV showed the least decrease of the trochanter BMD. On the other hand, no major change was reported in the Areal BMD in any group of the study by Slatkovska et al. [65] where the two intervention groups were WBV with different frequencies either high frequency (90Hz) or low frequency (30Hz) of WBV.
Compared two different groups of WBVs, i.e., Vertical Vibration Training (VVT) and Rational Vibration Training (RVT), whereas Verschueren et al. [66] compared the WBV with another type of exercises, i.e., resistance training. In both of these studies, participants were given low limb strengthening exercises on the platform. BMD improved in the total hip in the training groups, while no change was observed in the resistance group or controls [68].
In two WBV studies, the control groups were either given a placebo device [69] or low intensity exercise which targeted fitness and did not affect the endpoint chosen. In that study the primary endnote was BMD at (FN) and LS (L1-L4) as the authors acknowledged. Both (RVT and VVT) groups demonstrated an improvement of the BMD at the LS and FN compared to LS BMD loss that was noted in the control group. On the other hand, FN BMD was maintained in the latter group. Rubin et al. [69] demonstrated a significant improvement of the spine BMD in the active WBV group compared to BMD loss in the placebo device group.
Exercises alone versus a combination of calcium and vitamin D: A total of 11 trials of all the included trials had calcium/vitamin D added to the programme, where only one trial specifically assessed the effectiveness of the calcium alone and with exercise.
A) Weight bearing: Prince et al. [56] included 3 groups supplemented with calcium either by milk powder or tablet, or exercise with tablets of calcium, and the placebo group which was the control. Exercise and calcium groups could maintain BMD at hip, trochanter and inter trochanter including FN which did not maintain the BMD in the calcium group.
Another weight bearing study by Going et al. [45] showed significant improvement of the trochanter BMD the in the exercise-only group compared to other groups (HRT, HRT+exercise and placebo groups). All subjects were supplemented with calcium in all groups.
B) Non-weight bearing: The majority of the non-weight bearing participants were given calcium/vitamin D. However, some trials had participants that were not supplied with calcium [59,67].
Active groups in these studies who exercised maintained the BMD level compared to two trials where not all participants were given calcium [42,47]. In Bemben et al. [42] study, only subjects who had a calcium level of less than 1500 mg/day and Chilibeck et al. [47] only provided calcium for subjects who were not in the Bisphosphonates group. Although, exercisers in Chilibeck et al. [47] study had a significant increase of the LS BMD, after removing an outlier with a family history of osteoporosis, no main effect of the exercise remained ( p=0.065).
While exercisers in Bemben et al. [42] maintained BMD level at total body, spine and proximal femur. non-weight bearing did not seem to be effective to significantly improve the BMD level with or without calcium.
C) Combination: Two of the combination exercise trials showed an increase of the BMD [49,53]. A significant increase of the BMD at the trochanter was observed in a study by Metcalfe et al. [49] when combination exercise groups were compared to controls.
Another study observed a slight increase of the BMD at total hip compared to a significant loss in the control group at the same site [53], or maintenance of the BMD at total hip and trochanter [61] in the exercise group alone.
D) Whole body vibration: A study showed a significant BMD improvement at LS of both VVT and RVT groups compared to controls with sham exercises that did not affect BMD. On the contrary, no effect on the BMD was found at any site of LS total hip and FN in a trial by Slatkovska et al. [65].
Adding calcium to weight bearing exercise seems to prevent bone loss, although it is difficult to determine if the change of the BMD happened due to a combination of exercise and calcium, in most of the studies all subjects were given calcium. However, most of the controls in the trials who were also given calcium had a decrease of the BMD which may indicate calcium alone had no effect on BMD.
All subjects had both Vitamin D with calcium in only 5 studies [47,53,60,65].
Effects of the medications with exercise: A considerable number of studies in this review assessed the effects of some medications by dividing groups either with medications alone, exercises alone, or a combination of (medications and exercises) against controls.
Going et al. [45], Milliken et al. [51] and Tartibian et al. [58] showed good effects of combining exercise with medications, [45,51] combined exercise with HRT and found a slight improvement of the BMD, but Tartibian et al. [58] found a notable synergistic effect of Omega-3 and exercise.
On the other hand, some trials found no additional effects of combining exercise with bisphosphonates [61] or antioxidants [67]. Also, Wu et al. [57] found no noted effects of combining soy isoflavone with exercises, but with the extension of this trial [68] the most significant preservation of the BMD at Ward’s triangle happened in the exercises with isoflavone. Surprisingly, Chilibeck et al. [61] found negative effects of combining isoflavone with exercises, effects (decline) on the BMD of the total hip and trochanter, more than it was found in the control group. Compliance to the calcium was high in all groups (p>0.05).
In the majority of studies that combined exercises with a variety of medications, good effects were found however, most of them were only slight improvements and some negative synergistic effect was found.
Frequency of interventions: In the included studies, either most of them used the same or they varied remarkably.
A) Weight bearing exercise: The majority of weight bearing trials had a frequency of 3 times/week. A trial with more frequency than 3 times/week i.e., 4 times/week [54] found that the intervention group with TCC had a significant decrease of the BMD only at trochanter compared to BMD loss at FN and trochanter in the controls. Also Preisinger et al. [46] had at least 3 times/week intervention and found a significant decrease of the BMD at the proximal and distal forearm in the weight bearing exercise group compared controls with usual activity.
Also Sakai et al. [55] used a unipedal standing for one minute on each leg and found no effect of the BMD in the intervention group compared to the controls.
Which might indicate the change of the BMD is related to the activity of the weight bearing exercise rather than the frequency, which is difficult to do in this review due to the large variety of the exercises and the activities in the same exercise type.
B) Non-weight bearing: A total of 3 times/week was the frequency of all the non-weight bearing trials, so it is difficult to assess what the optimum frequency is.
C) Combination of exercises: Two studies had almost the same activities in terms of the combination of exercises [49,51]. Metcalfe et al. [49] intervention included walking with vests, resistance training, abdominal strengthening, stretching and balance. Milliken et al. [51] study included resistance training and walking with vests, and both studies had a frequency of 3 days/week and showed a significant increase BMD at the hip (trochanter, Ward’s triangle) respectively.
D) Whole body vibration: Two studies with similar frequency (3 days/week) and similar protocol i.e. exercising on the platforms but with different vibration frequency, showed a significant effect of the BMD. A significant increase at the LS of both (VVT and RVT) compared to controls with a sham exercise also Verschueren et al. [66] had an improvement of the BMD at the hip compared to maintaining the BMD in the resistance exercise group.
Slight loss of the BMD was found in two varied frequencies i.e. twice a day or twice a week, in two WBV studies [64,69]. In Rubin et al. [69] WBV subjects were standing on a high frequency platform i.e. 30Hz, compared to controls with a placebo device. While in Beck and Norling et al. [64] subjects were exposed to different vibration frequencies i.e. 12.5 Hz, 30 Hz, no absolute effect of the frequency of standing on the WBV was found in the WBV studies, this might be due to the difference of the frequency of the vibration used.
Supervision: Most of the studies were supervised except Rubin et al. [64,65]. In Rubin et al. [69] study, subjects had the WBV platforms delivered to their home to aid the blindness of the study and the compliance was taken from a recorder attached to the device. Slatkovska et al. [65] adherence was a self-reported adherence after 6 months, and the actual adherence was extracted from a digital clock recording time, date, and duration of every session .Finally the study of used A DVD player as a guide for exercise on the platforms, subjects had to sign every session for determining compliance.
Furthermore the supervision status was not mentioned in Verschueren et al. [66], Sakai et al. [55], Tartibian et al. [58].
Some studies were partially supervised [46,48,50,53,63] which means, patients were not supervised for all the conducted sessions. In only one of these trials the unsupervised sessions were taking place at home [53].
Risk of bias assessment: Evaluating the risk of bias with the Jadad tool in which a score of 0-2 means high isk of bias and a score of 3-5 means low risk of bias, only 6 trials demonstrated a low risk of bias as they scored 3 or more out of 5 [53,55,61,65,69]. All trials received a score of at least 1, as randomisation (one of the tool’s criteria) was required for the inclusion in this review. However, only nine studies discussed the randomisation process in sufficient detail and used appropriate randomisation methods. Only one study received the full score [61].
A common final score among the included trials was 2 out of 5. Points were lost for a lack of double-blinding and appropriate blinding. Some trials used double-blinding, however only for the medication aspect of the respective study, not the exercise intervention. As this review focused on the exercise intervention, these studies received 0 in the blinding category.
In three studies, participants and investigators were blinded to the group allocation. Rubin et al. [69] participants and investigators were blinded to what group was given an active or placebo vibrating platform, and another study by Chubak et al. [48], subjects in the control groups were given sham exercises i.e. stretching. Lastly, Chilibeck et al. [61] blinded subjects to the hypothesis of the study, and subjects were asked to perform sham exercises [61].
A considerable number of the studies blinded the technicians to assess BMD [46,48,53,59,61,63,65,66]. Also blinded participants were given sham to blind them and were unaware of the hypothesis
Dropouts and withdrawals were discussed and reasons for the premature end of participation were given in the majority of studies. Intention to treat was performed in a few studies which experienced a loss of follow up [45,47,48,63,64,69].
Discussion
After a comprehensive literature search, 27 studies were included in this review. The studies included four different main types of exercises for intervention: Weight bearing, non-weight bearing, combination and whole body vibration. Postmenopausal women with no osteoporosis performed exercises alone, with calcium/vitamin D supplements or other medical therapy e.g. HRT, added to the regimen.
Effectiveness of different types of exercise
A) Weight bearing exercise: A total of seven weight bearing trials satisfied the inclusion criteria for this review. Favourable effects on BMD either by maintaining or improving BMD slightly or significantly compared to the controls were reported.
However two studies reported no difference in BMD measurements between groups, and the general trend of the BMD for those two studies was decreasing [46,57]. Preisinger et al. [46] did not find any significant effects of weight bearing exercises including: brisk walking, jogging and complex exercises for training (diagonal or diagonal-spiral movements) when a longitudinal analysis was performed, there was a significant decrease in the BMD, while no significant change of the BMD was observed by the cross sectional analysis. The BMD was only measured in the proximal and distal forearm, not at the body’s main weight bearing sites, such as the hip, FN, LS. One could argue that the weight bearing exercises might potentially have a more significant impact on the participants’ weight bearing areas by placing increased loads on the bone structure; however, a comparison between different sites across the body might have provided somewhat different results.
This could be supported by the findings of Going et al. [45] who determined the greatest effect of weight bearing exercises at the trochanter, which is possibly because most of the performed exercises targeted the lower limb e.g. squats, stair climbing, skipping rope. However, Preisinger et al. [46] found that when participants in the exercise group were divided based on the regularity of the exercises, those who exercised regularly i.e. at least 3 times/week, showed a significantly lower bone loss at both sites of the forearm than those who exercised irregularly or less than one hour a week. Compliance was generally low in this study (48%), which suggests that the effects of exercise could be closely related to compliance and the regularity and frequency of the exercise activity.
The low compliance to the exercise was also an issue in a 2 year study of undefined weight bearing exercises, walking and calcium intake .The sessions were partially supervised, which could explain the low compliance rate. Prince et al. [56] found that only 39% of the exercise group performed the exercises regularly (3 hours/week). Nevertheless, the results showed that all the groups managed to maintain BMD at the trochanter, inter trochanter and the hip site but not at the FN, which was significantly higher in the exercise+calcium group compared to calcium tablet group.
Although the latter study had a shorter intervention duration than Preisinger’s [46] trial, (exercise+calcium group), Prince et al. [56] showed maintenance of the BMD but the study was measured at many sites, and that gives more ability to detect the change of BMD level at rather than if restricted to one site i.e. forearms like in Preisinger et al. [46]. Prince et al. [56] study shows subjects were already performing exercises for less than 2 hours a week before the beginning of the study which could help to maintain the BMD at all measured sites despite the low compliance.
Weight bearing trials with good effects on the BMD tended to have duration of one year or more, except for one [58]. This study had duration of 24 weeks, and looked at the effect of the exercise alone, which was mainly walking or jogging on a treadmill, compared to exercise with Omega-3 supplements, omega-3 alone, or controls with no intervention. The BMD improvement was slight in the exercise alone group at femoral neck and LS (L2-L4), but it was more significant than the control group, which may indicate that longer interventions may lead to more increases of the BMD.
Supporting this claim, in other weight bearing studies with a 6 month-intervention, no significant effects on BMD were found [55,57]. A six-month study of walking exercise with isoflavone intake or a placebo drug against isoflavone or placebo alone determined no significant differences in BMD between the groups after the treatment duration [57]. When that trial was extended to a total of 12 months [68] participants in the walking with placebo group had maintained total hip BMD, while the other 3 groups had decreased. Both walking with placebo and the isoflavone supplement alone showed maintenance of BMD at Ward’s triangle, while the other groups experienced a decrease in BMD, however, this study’s focus was rather on the effect of the exercise on fat mass, not on the BMD, which might have been a reason for bias.
Similarly to the previous 6-month studies, Sakai et al. [55] also failed to find effects of the weight bearing exercises on the BMD. The intervention was unipedal standing for one minute on each leg, 3 sets a day, however, when subjects were divided into groups based on age, women who were ≥ 70 years, saw a major improvement of the BMD at different sites i.e. Ward’s triangle and inter trochanter area, than women <70 years. This might indicate BMD in older women responds more significantly to weight bearing exercise. Chan et al. [54] had almost the same principle of exercise i.e. spending time on an activity on feet, but the duration was longer than Sakai et al. [55] trial, at 1 year.
Maintenance of the BMD was noted in the Tai Chi Chun (TCC) group compared to a significant loss in the FN BMD of the controls with usual activity, although the frequency of the TCC was 5 days per week compared to 3 times per week of walking in Wu et al. [68]. Both had a duration of one year and no calcium supplements, but the more frequent the exercise in Chan et al. [54] study showed no increase of the BMD level, which might mean TCC is less effective than only walking.
Results show that weight bearing exercise can maintain BMD level, and improvement was noted in longer durations with calcium supplementation. The two studies which observed a decrease of the BMD had a high risk of bias in that there was no focus on the BMD or no measure at the clinical important weight bearing sites; therefore a potentially beneficial effect cannot be entirely ruled out in these trials.
B) Non-weight bearing: Eight of the trials used non-weight bearing exercises as interventions. These were commonly combined with calcium/vitamin D supplements. The effects of non-weight bearing exercises in the studies were inconclusive. Maintenance of the BMD was documented in only 4 studies, two studies had conflicting results, and two showed a significant increase of the BMD.
Kerr et al. [52] reported the effects of either strength or fitness training compared to a control group, which were somewhat contradictory. Women in both fitness and strength groups undertook the same exercise, except that cycling was added to the fitness group. In this group, participants received constant minimum loads, while the strength training exercise was site specific and included hip extension, hip flexion and Latissimus dorsi pull down adding a stress on the hip which was gradually increased, so it is possible that gradual strengthening exercise which focus on the muscles attached to the hip can led to a BMD increase at intertrochanteric area and total hip while a decrease of total body BMD was noted.
Another conflicting finding was by Pruitt et al. [60] who did not report any significant change for either high or low intensity resistance training or controls with usual activity, except a slight proximal femur increase of the BMD in the control group. This might suggest that resistance exercise may not have a significant effect on BMD regardless of intensity, or that normal activity may be equally as effective as resistance training. Although subjects with HRT were ineligible to participate in that study, 4 subjects out a total of 11 controls were actually under HRT which might be the cause of this increment of the control BMD leading to statistical errors and bias. Also exercisers who were enrolled on different non-weight bearing exercise activities i.e. bench press, Lattisimus dorsi pull down, back extension, experienced more reduction of the BMD than controls. In a study by Chilibeck et al. [61] where the authors discovered that there was one subject with a history of severe osteoporosis, and after excluding that subject from analysis, the effect of exercise was found to maintain BMD.
Two of the non-weight bearing studies [59,67] had almost the same sample sizes in terms of age, duration, although there was a variation of the loads. Chuin et al. [67] started with performing 3 sets (8 repetitions) of one repetition maximum load (1-RM) then it was altered every 4 weeks, while Bocalini et al. [59] found that subjects that started with a resistance of one set at 50% of the 1-RM then gradually increased. The exercise groups maintained the BMD in LS only [67], compared to significant loss in controls with no intervention. In contrast, the placebo group in Bocalini et al. [59] maintained BMD at two clinically important sites, LS and FN. This might indicate that bone formation may respond better to low intensity resistance exercise [60].
One important aspect in most non-weight bearing studies might be a potentially indirect element of weight bearing, as many of the exercises were performed in standing or other positions in which added weight and would have increased the load on weight bearing joints. Potentially this may have had an effect on the BMD over the longer duration of the study and thus altered the results.
Several studies reported improvement in muscle size and strength, but not BMD, which might suggest the usefulness of non-WB exercises in an overall exercise programme to improve balance and protect joints in the prevention of osteoporosis, but might not directly affect the bone architecture.
Overall, it is difficult to reach a decisive conclusion about the effectiveness of non-weight bearing exercises on BMD based on the studies in this review, as a considerable number of studies show possible sources of bias and errors. The majority of the studies had small sample sizes, low adherence and a significant difference between compliance in groups was also noted [42] and large dropout rates [42,50,59,60]. In some cases dropouts/follow-up rates were not even mentioned [67]. Moreover, type 1 and 2 errors were mentioned as a limitation in Chilibeck et al. [47] study.
C) Combination: A total of 7 trials combined a variety of weight bearing and non-weight bearing exercises, moderate intense exercise, resistance training, aerobic, progressive weight bearing, abdominal strengthening, stretching and balance, coordination, jumping, walking and bicycling.
Some studies [48,53,63] had partial supervision for the treatment sessions. Especially in long interventions, partial supervision with a home exercise component might be an issue for this type of population (elderly women) as they might have a problem with memorising all of the exercises and do them in the exact way they were instructed to do without a guide present.
Also, performing exercises in the presence of an instructor, as many of the studies did, might help to encourage doing the exercises more correctly and regularly, rather than exercising alone. Moreover, a general problem with home-based exercises can be adherence, although Bolton et al. [53] reported that adherence was excellent. All three studies showed no significant change of the BMD, potentially the exercise interventions might have had more significant effects if the activities had been fully supervised, thus ensuring compliance and correct performance.
Two trials with full supervision showed a significant improvement of the BMD [49,51] at trochanter and Ward’s triangle respectively). Subjects in these trials performed walking as a weight bearing exercise wearing vests containing loads, besides other interventions i.e. Metcalfe et al. [51] who had a variety of exercises other than walking including climbing stairs, resistance exercise for large and small muscle groups, abdominal strengthening, stretching and balance. While Milliken et al. [51] resistance exercise targeted large and small muscle groups, including squats, back extension, and so on. Chilibeck et al. [61] study, included exercisers who performed resistance exercise and brisk walking, the controls were given stretching exercises 4 days a week which were used as sham intervention, all groups showed a reduction of the BMD at the total hip and trochanter.
The contradicting results in the difference of the BMD trend at weight bearing sites of [49,51,61] might be due to using weight vests, as a weight bearing study of Wu et al. [57] found that intervention of only walking 60 minutes 3 times a week reduced BMD. Thus, potentially walking with added weight/increased loads may be more effective than normal functional walking.
Chubak et al. [48] assessed the effectiveness of the combination exercises including moderate intensity training, walking and cycling, compared to stretching as a sham exercise finding no significant change of the total body BMD in the exercise group. The authors were too selective in their participant selection as they focused on over-weight women who were already performing less than one hour per week of moderate to vigorous intensity exercise before engaging in this .The effect of the exercise was mainly to check fat mass which was the reason mentioned by the authors about the lack of measuring BMD at some significant sites as only total body BMD was reported, and maybe some increase of the BMD would be found at some body areas.
However, women older than 60 years experienced more BMD improvement compared to younger women, which was the same finding as a unipedal standing study for Sakai et al. [55], where the higher increase of BMD was found in older women i.e. >70. This may indicate the effectiveness of exercise during the weight bearing activity which is more apparent in older subjects.
In a study of Englund et al. [62] the subjects had nearly the same age range as the 2 studies mentioned above 66-87. The effect of combination exercises including strengthening, coordination, aerobic and balance were found at the Ward’s triangle, arms, LS and trochanter in the exercise group compared to a significant decrease on Ward’s triangle BMD which was significantly lower than he controls. However, these results were found after adjusting the differences of the baseline characteristics. On the other hand, arms and trochanter had a significant increase of the BMD in the control subjects. In this trial, participants were actively seeking exercise advice before the authors assessed their eligibility for the study. Some participants were disappointed when they were allocated to the control group, which might have influenced their compliance to the control intervention; Lack of blinding may therefore have impacted on the results in this study.
Surprisingly, a lack of increase in FN BMD was found in the exercise group. This might be due to an absence of increased loads, which might not have provided adequate strain to increase the osteogenic response at that site. Another possible explanation is that bone turnover is higher in the cancellous bone of the trochanter.
A number of combined exercise studies examined long-term effects of the intervention in follow-up assessments [62,63]. Englund et al. [62] aimed to determine the effect five years after exercise cessation, finding that all groups lost BMD at all the measured sites except at LS. Similarly, Korpelainen et al. [63] assessed the effect of combined exercises after 6 years finding a reduction of BMD in both exercise and control groups across time.
Ideal frequency of different types of exercise
A) Weight bearing exercise: Studies in the weight bearing category had different frequencies of exercise ranging from 3 times/day [55] to 3 days/week [45]. Sakai et al. [55] managed to maintain BMD in both unipedal and control group showing that a unipedal standing assists an increase in the BMD significantly at the hip only in women over 70 years of age, while Going et al. [43] found weight bearing exercise alone improved BMD significantly at the trochanter.
Although the frequency of the study by Chan et al. [54] was higher than Going et al. [45] they found a significant decrease only at trochanter in the TCC group, compared to a significant decrease of the BMD at both FN and trochanter. This might be due to the difference of both of the exercises used in the two studies. It is difficult and unreliable to compare weight bearing studies with different exercise protocols, intensity and loads.
B) Non-weight bearing: All weight bearing had a frequency of 3/week, and it was difficult to determine if frequency could alter the results. However, despite all studies having the same frequency, a variation of the results was found within each study. This might be due to the different intensity used for exercises.
C) Combination: The combination of two exercise trials which determined a significant improvement of the BMD was found in Metcalfe et al. [49] and in Milliken et al. [51] which almost had the same exercise regimens included resistance training aerobic exercises. These studies had a frequency of 3 times/week of exercise, and the controls were subjects with no intervention. Another study by Bolton et al. [53] which also had a frequency of 3 times/week, total hip BMD increased non-significantly compared to non-significant BMD loss in the controls with usual life activity. Englund et al. [62] study had less frequency than the earlier studies i.e. 2 times/week, with a variety of aerobic, balance and coordination exercises which resulted in a slight increase of the Ward’s triangle in the exercise group compared to a no significant decrease of the Ward’s triangle BMD in the controls with no intervention, this might indicate that 3 times/a week of combination exercise could either maintain or improve BMD.
The exercise programmes in two studies had some similar components e.g. strength training, aerobic, walking, and had a frequency more than 5 days a week, the two studies had a difference in the supervision status and the place of the exercise. Chubak et al. [48] study was a partially supervised programme either at home or the gym, while participants in Chilibeck et al. [61] were fully supervised at the study setting and observed a not-significant decrease of the exercise group at hip. Chubak et al. [48] found no effect of the exercise, but the total body BMD was higher in subjects older than 60 years, this might mean that there are some factors like age that effect the exercise programme more than the frequency.
The effectiveness of the combination exercise might depend more on some factors than the frequency, such as the protocols used, the intensity of the non-weight bearing and age.
Heterogeneity
There was a large amount of heterogeneity in the interventions between different studies, exercise components even within the same category: for instance the weight bearing category included TCC, walking, unipedal standing, and so on. Moreover, in the intervention groups, some studies compared the exercise with controls with usual activity and some others compared exercise with medication, or the exercise was compared to controls with sham, which might have affected he accuracy of the results. Limiting the heterogeneity was attempted by including only trials that compared interventions to controls with usual activity or who had sham intervention. Nevertheless a large amount of heterogeneity remained due to the diversity of interventions, durations, frequencies and variables in participant selection, making an overall general conclusion regarding the effectiveness of exercise difficult. Narrowing the analysis of the results to the exercise subcategories allowed identifying certain trends.
Limitations and Weakness of the Review
The search strategy for this review produced a number of relevant articles. However, it is possible that other relevant articles were not found because of the limited databases in exercises and physiotherapy, as only a relatively new database (PEDro) has been developed. There are various medical and allied medical science databases that may not be specific enough to search within for articles related to exercises and physiotherapy. Considerable effort was employed to find all the relevant articles based on the aims, objectives, and inclusion and exclusion criteria. Limiting the results to English language articles may have reduced the number of available papers and it is possible that further relevant results may be found in foreign language studies. The heterogeneity of the included studies limited the conclusiveness of the results. Narrowing down the research question to specific categories of exercises or specifying the inclusion/exclusion criteria further might have provided more consistent results, but on the other hand might have ignored relevant findings in other categories.
Recommendations for Future Trials
It is important to conduct new trials in order to find more conclusive results on the effectiveness of exercises on BMD in the prevention of osteoporosis in postmenopausal women. These trials should include some features:
(1) The study must have a low risk of bias, which can be done by focusing on blinding (patient, therapist and assessor). Also, the method of randomisation should be explained clearly, accounting for subjects who were lost to follow-ups and reporting reasons for the losses. Although it is difficult to blind participants to exercises, they might be blinded about the aim of the study by involving them in a sham exercise, or exercises that do not affect the primary endnote, e.g. upper limbs exercises, while the aim is to measure the implications of exercises on the lower limbs.
(2) Studies should investigate the effects of an exercise regimen in preventing osteoporosis in postmenopausal women using long-term treatment duration and different frequencies. Generally longer studies had more effectiveness of the intervention but a considerable number of the included trials had only 6 months of follow up, and no adequate trials were found assessing the effects of different frequencies of the exercises on the BMD thus, more clarification about the possible effect of exercises in the long term and the optimum frequency is required.
(3) Studies with larger sample sizes are needed.
(4) More trials should look into weight bearing, non-weight bearing and a combination of weight bearing and non-weight bearing, thus aiming to overcome the errors in the previous trials to find more accurate results.
(5) In the whole body vibration (WBV) performing exercise on platforms should be also performed separately by other groups, to compare the effect of the each intervention alone and with WBV.
(6) Studies that compare the effects of the calcium with exercise, calcium alone, exercise alone with control, in order to determine the effectiveness of the calcium with or without exercise should be conducted.
Conclusions
The aim of this review was to assess the effectiveness of different types of exercise on BMD in post-menopausal women, including weight bearing exercise, non-weight bearing exercise, a combination of weight bearing and non-weight bearing as well as vibration. Further, aims were to identify evidence about optimal exercise frequency and the effects of adding nutritional supplements, especially calcium and/ or vitamin D, to the intervention.
Weight bearing exercise appeared to have good effects on the BMD in post-menopausal women with longer intervention time and maybe calcium/vitamin D supplements however, some studies were not conclusive. Most of the non-weight bearing exercise studies used additive medication and supplements e.g. calcium, vitamin D, HRT, but the results were not significantly in favour to these types of exercises.
However, longer studies showed more notable effects than shorter studies, which suggests that non-weight bearing exercises over a longer duration may have beneficial effects on BMD.
Combination exercise trials showed no significant effects on BMD, but some good effects were noted when the exercises were combined with HRT. The majority of studies had low quality assessment scores, which may have influenced the results. Some sources of risk of possible risk bias and errors were found in most of the trials especially in the non-weight bearing studies like small sample sizes, large dropout rates and low compliance which should be avoided in the future research.
In terms of frequency, most studies performed exercise 3 times/ week which showed good effects on BMD. The longer the term of the treatment duration, the more benefits on BMD were noted. The most effective frequency of each type of exercise was difficult to determine due to the large variety of the exercises and participant compliance. Furthermore, some frequencies of the exercises were changed during the trials, so future research should aim to test exercise with a variety of frequencies.
Adding calcium seemed to be beneficial when accompanied with exercises, especially weight bearing or combination exercises, while calcium alone appeared to have no effectiveness on the BMD. However, in many of those studies, all groups received calcium supplements, allowing no clear conclusion about the effect of calcium and exercise in comparison to no supplementation or exercise.
Summarizing the results of this review, weight bearing exercise might be the recommended exercise type for maintaining or improving BMD in post-menopausal women especially when combined with nutritional supplements. However, further research should confirm validity of the results with larger sample sizes and improve study quality for both non-weight bearing and a combination of weight bearing and non-weight bearing exercise types which showed controversial results on BMD in this review. Whole body vibration combined with exercise seems to give good results on BMD, but further research is recommended to distinguish effects of WBV plus exercise against exercise alone.
Overall, however, due to a considerable amount of heterogeneity and a lack of distinction between the effects in combined interventions, the results of this review are not conclusive enough to allow for a recommendation regarding the effectiveness of a specific intervention in this population. In order to provide a solid evidence base for practice recommendations in the treatment and prevention of osteoporosis, further high quality research is necessary.
Acknowledgments
I am very grateful to Dr. Stuart for his invaluable support and assistance throughout the development of this dissertation. I would also like to thank Bianca, Dhoha and Alanood for their advice and support.
References
- Demontiero O, Vidal C, Duque G (2012) Aging and bone loss: new insights for the clinician. TherAdvMusculoskelet Dis 4: 61-76.
- Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359: 1761-1767.
- Ford MA, Bass MA, Keathley R (2007) Osteoporosis knowledge and attitudes: a cross-sectional study among college-age students. J Am Coll Health 56: 43-47.
- Garnero P, Sornay-Rendu E, Claustrat B, Delmas PD (2000) Biochemical markers of bone turnover, endogenous hormones and the risk of fractures in postmenopausal women: the OFELY study. J Bone Miner Res 15: 1526-1536.
- Adachi JD (2010) Impact of Prevalent Fractures on Quality of Life: Baseline Results From the Global Longitudinal Study of Osteoporosis in Women. Mayo ClinProc 85: 806-813.
- Jang JH, Castano O, Kim HW (2009) Electrospun materials as potential platforms for bone tissue engineering. Adv Drug Deliv Rev 61: 1065-1083.
- Ito M, Nakamura T, Tsurusaki K, Uetani M, Hayashi K (1999) Effects of menopause on age-dependent bone loss in the axial and appendicular skeletons in healthy Japanese women. Osteoporosint 10: 377-383.
- Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ 3rd, et al. (2008) A reference standard for the description of osteoporosis. Bone 42: 467-475.
- Francis RM, Baillie SP, Chuck AJ, Crook PR, Daymond T, et al. (2000) Management of osteoporosis in patients with hip fractures. QJM 93: 501-506.
- Kotz K, Deleger S, Cohen R, Kamigaki A, Kurata J (2004) Osteoporosis and health-related quality-of-life outcomes in the Alameda County Study population. Prev Chronic Dis 1: 1-9.
- Bianchi ML, Orsini MR, Saraifoger S, Ortolani S, Radaelli G, et al. (2005) Quality of life in post-menopausal osteoporosis. Health Qual Life Outcomes 3: 78.
- Hannan MT, Felson DT, Dawson-Hughes B, Tucker KL, Cupples LA, et al. (2000) Risk factors for longitudinal bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res 15: 710-720.
- Ilich JZ, Kerstetter JE (2000) Nutrition in bone health revisited: a story beyond calcium. J Am CollNutr 19: 715-737.
- Cashman KD (2007) Diet, nutrition and bone health. J Nutr 137: 2507S-2512S.
- Lips P (2001) Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev 22: 477-501.
- Martin AR, Sornay-Rendu E, Chandler JM, Duboeuf F, Girman CJ, et al. (2002) The impact of osteoporosis on quality-of-life: the OFELY cohort. Bone 31: 32-36.
- Cranney A, Jamal SA, Tsang JF, Josse RG, Leslie WD (2007). Low bone mineral density and fracture burden in postmenopausal women. CMAJ 177: 575-780.
- Kanis JA, Glüer CC (2000) An update on the diagnosis and assessment of osteoporosis with densitometry. Committee of Scientific Advisors, International Osteoporosis Foundation. Osteoporosint 11: 192-202.
- Blake GM, Fogelman I (2007) Role of dual-energy X-ray absorptiometry in the diagnosis and treatment of osteoporosis. J ClinDensitom 10: 102-110.
- Binkley TL, Berry R, Specker BL (2008) Methods for measurement of pediatric bone. Rev EndocrMetabDisord 9: 95-106.
- Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359: 1929-1936.
- Kerstetter JE, Kenny AM, Insogna KL (2011) Dietary protein and skeletal health: a review of recent human research. CurrOpinLipidol 22: 16-20
- Eichner SF, Lloyd KB, Timpe EM (2003) Comparing therapies for postmenopausal osteoporosis prevention and treatment. Ann of pharmacother 37: 744-746.
- Dane C, Dane B, Cetin A, Erginbas M (2007) Comparison of the effects of raloxifene and low-dose hormone replacement therapy on bone mineral density and bone turnover in the treatment of postmenopausal osteoporosis. GynecolEndocrinol 23: 398-403.
- Chapurlat, Delmas PD (2006) Drug insight: Bisphosphonates for postmenopausal osteoporosis. Nature clinical practice. EndocrinolMetab 2: 211-219.
- Christodoulou C, Cooper C (2003) What is osteoporosis? Postgrad Med J 79: 133-138.
- Lange U, Teichmann J, Uhlemann C (2005) Current knowledge about physiotherapeutic strategies in osteoporosis prevention and treatment. RheumatolInt 26: 99-106.
- Heydarnejad S, Dehkordi AH (2010) The effect of an exercise program on the health-quality of life in older adults. A randomized controlled trial. Dan Med Bull 57: A4113.
- Lord SR, Ward JA, Williams P, Zivanovic E (1996) The effects of a community exercise program on fracture risk factors in older women. OsteoporosInt 6: 361-367.
- Mccartney N, Hicks AL, Martin J, Webber CE (1995) Long-term resistance training in the elderly: effects on dynamic strength, exercise capacity, muscle and bone. J Gerontol A BiolSci Med Sci 50: B97-104
- Forwood MR, Larsen JA (2000) Exercise recommendations for osteoporosis. A position statement of the Australian and New Zealand Bone and Mineral Society. AustFam Physician 29: 761-764.
- Gutin B, Kasper MJ (1992) Can vigorous exercise play a role in osteoporosis prevention?A review. Osteoporosint 2: 55-69.
- Bouxsein ML, Marcus R (1994) Overview of exercise and bone mass. Rheum Dis Clin North Am 20: 787-802.
- Adachi JD (1996) Current treatment options for osteoporosis. J RheumatolSuppl 45: 11-14.
- Burr DB (1997) Muscle strength, bone mass, and age-related bone loss. J Bone Miner Res 12: 1547-1551.
- Frost HM (1997) On our age-related bone loss: insights from a new paradigm. J Bone Miner Res 12: 1539-1546.
- Layne JE, Nelson ME (1999) The effects of progressive resistance training on bone density: a review. Med Sci Sports Exerc 31: 25-30
- Bergström I, Landgren B, Brinck J, Freyschuss B (2008) Physical training preserves bone mineral density in postmenopausal women with forearm fractures and low bone mineral density. OsteoporosInt 19: 177-183.
- Martyn-ST James M, Carroll S (2006) A meta-analysis of impact exercise on postmenopausal bone loss: the case for mixed loading exercise programmes. OsteoporosInt 17: 1225-1240.
- Howe TE, Shea B, Dawson LJ, Downie F, Murray A, et al. (2011). Exercise for preventing and treating osteoporosis in postmenopausal women. Cochrane Database Syst Rev 2: 55-69.
- Higgins JPT, Green S (2009) Cochrane Handbook for Systematic Reviews of Interventions5.0.2. In: The Cochrane Library, Chichester, UK: John Wiley & Sons, Ltd.
- Bemben DA, Fetters NL, Bemben MG, Nabavi N, Koh ET (2000) Musculoskeletal responses to high-and low-intensity resistance training in early postmenopausal women. Med Sci Sports Exercise 32: 1949-1957.
- Engelke K, Kemmler W, Lauber D, Beeskow C, Pintag R, Kalender WA (2006). Exercise maintains bone density at spine and hip EFOPS: a 3-year longitudinal study in early postmenopausal women. OsteoporosInt 17: 133-142.
- El Maghraoui A, Roux C (2008) DXA scanning in clinical practice. QJM 101: 605-617.
- Going S, Lohman T, Houtkooper L, Metcalfe L, Flint-wagner H, et al. (2003) Effects of exercise on bone mineral density incalcium-replete postmenopausal women with and without hormone intensity versus low-intensity resistance training program on bone mineral density in older women. J bone miner res 10: 1788-1795.
- Preisinger E, Alacamlioglu Y, Pils K, Saradeth T, Schneider B (1995) Therapeutic exercise in the prevention of bone loss: a controlled trial with women after menopause. Am J Phys Med Rehabil 74: 120-123.
- Chilibeck PD, Davison KS, Whiting SJ, Suzuki, Y, Janzen CL, Peloso P (2002) The effect of strength training combined with bisphosphonate (etidronate) therapy on bone mineral, lean tissue, and fat mass in postmenopausal women. Can J PhysiolPharmacol 80: 941-950.
- Chubak J, Ulrich CM, Tworoger SS, Sorensen B, Yasui Y, et al. (2006) Effect of exercise on bone mineral density and lean mass in postmenopausal women. Med Sci Sports Exerc 38: 1236-1244.
- Metcalfe L, Lohman T, Going S (2001) Post-menopausal Women and Exercise for Prevention of Osteoporosis. ACSM'S Health Fitness J 5: 6-14.
- Cussler EC, Lohman TG, Going SB, Houtkooper LB, Metcalfe LL, et al. (2003) Weight lifted in strength training predicts bone change in postmenopausal women. Med Sci Sports Exerc 35: 10-17.
- Milliken LA, Going SB, Houtkooper LB, Flint-wagner HG, Figueroa A, et al. (2003) Effects of exercise training on bone remodeling, insulin-like growth factors, and bone mineral density in postmenopausal women with and without hormone replacement therapy. Calcif Tissue Int 72: 478-484.
- Kerr D, Ackland T, Maslen B, Morton A, Prince R (2001) Resistance training over 2 years increases bone mass in calcium-replete postmenopausal women. J Bone Min Res 16: 175-181.
- Bolton KL, Egerton T, Wark J, Wee E, Matthews B, et al. ( 2012) Effects of exercise on bone density and falls risk factors in post-menopausal women with osteopenia: a randomised controlled trial. J Sci Med Sport 15: 102-109.
- Chan K, Qin L, Lau M, Woo J, Au S, et al. (2004) A randomized, prospective study of the effects of Tai Chi Chun exercise on bone mineral density in postmenopausal women. Archives Phys Med Rehabil 85: 717-722.
- Sakai A, Oshige T, Zenke Y, Yamanaka Y, Nagaishi H, et al. (2010) Unipedal standing exercise and hip bone mineral density in postmenopausal women: a randomized controlled trial. J Bone Miner Metab 28: 42-48.
- Prince R, Devine A, Dick I, Criddle A, Kerr D, et al. (1995) The effects of calcium supplementation (milk powder or tablets) and exercise on bone density in postmenopausal women. J Bone Miner Res 10: 1068-1075.
- Wu J, Oka J, Higuchi M, Tabata I, Toda T, et al. (2006a). Cooperative effects of isoflavones and exercise on bone and lipid metabolism in postmenopausal Japanese women: a randomized placebo-controlled trial. Metabolism 55: 423-433.
- Tartibian B, Maleki HB, Kanaley J, Sadeghi K (2011) Long-term aerobic exercise and omega-3 supplementation modulate osteoporosis through inflammatory mechanisms in post-menopausal women: a randomized, repeated measures study. NutrMetab 8.
- Bocalini DS, Serra AJ, Dos Santos L, Murad N, Levy RF (2009) Strength training preserves the bone minearl density of postmenopausal women without hormone replacement therapy. J Aging Health 21: 519-527.
- Pruitt LA, Taaffe DR, Marcus R (1995) Effects of a one-year high-intensity versus low-intensity resistance training program on bone mineral density in older women. J Bone Miner Res 10: 1788-1795.
- Chilibeck PD, Vatanparast H, Pierson R, Case A, Olatunbosun O, et al. (2013) Effect of exercise training combined with isoflavone supplementation on bone and lipids in postmenopausal women: A randomized clinical trial. J Bone Miner Res 28: 780-793.
- Englund U, Littbrand H, Sondell A, Pettersson U, Bucht G (2005) A 1-year combined weight-bearing training program is beneficial for bone mineral density and neuromuscular function in older women. OsteoporosInt 16: 1117-1123.
- Korpelainen R, Keinanen-kiukaanniemi S, Heikkinen J, Vaananen K, Korpelainen J (2006) Effect of impact exercise on bone mineral density in elderly women with low BMD: a population-based randomized controlled 30-month intervention. OsteoporosInt, 17: 109-118.
- Beck BR, Norling TL (2010) The effect of 8 mos of twice-weekly low- or higher intensity whole body vibration on risk factors for postmenopausal hip fracture. Am J PhysMed Rehabil 89: 997-1009.
- Slatkovska L, Alibhai S, Beyene J, Hu H, Demaras A, et al. (2011) Effect of 12 months of whole-body vibration therapy on bone density and structure in postmenopausal women. Ann Intern Med 155: 668-679.
- Verschueren SM, Roelants M, Delecluse C, Swinnen S, Vanderschueren D, et al. (2004) Effect of 6-month whole body vibration training on hip density, muscle strength, and postural control in postmenopausal women: a randomized controlled pilot study. J Bone Miner Res 19: 352-359.
- Chuin A, Labonte M, Tessier D, Khalil A, Bobeuf F, et al. (2009) Effect of antioxidants combined to resistance training on BMD in elderly women: a pilot study. Osteoporosis International 20: 1253-1258.
- Wu J, Oka J, Tabata I, Higuchi M, Toda T, et al. (2006b). Effects of isoflavone and exercise on BMD and fat mass in postmenopausal Japanese women: a 1-year randomized placebo-controlled trial. J Bone Miner Res 21: 780-789.
- Rubin C, Recker R, Cullen D, Ryaby J, Mccabe J, et al. (2004) Prevention of postmenopausal bone loss by a low-magnitude, high-frequency mechanical stimuli: a clinical trial assessing compliance, efficacy, and safety. J Bone Min Res 19: 343-351.
- Russo C, Lauretani F, Bandinelli S, Bartali B, Cavazzini C, et al. (2003) High-frequency vibration training increases muscle power in postmenopausal women. Arch Phys Med Rehabil 84: 1854-1857.
- Carter ND, Khan KM, Mckay HA, Petit MA, Waterman C, et al. (2002) Community-based exercise program reduces risk factors for falls in 65- to 75-year-old women with osteoporosis: randomized controlled trial. CMAJ 167: 997-1004.
- Chien MY, Yang RS, Tsauo JY (2005) Home-based trunk-strengthening exercise for osteoporotic and osteopenic postmenopausal women without fracture -- a pilot study. ClinRehabil 19: 28-36.
- Iwamoto J, Takeda T, Ichimura S (2001) Effect of exercise training and detraining on bone mineral density in postmenopausal women with osteoporosis. J OrthopSci 6: 128-132.
- Bassey EJ,Ramsdale SJ(1995) Weight-bearing exercise and ground reaction forces: a 12-month randomized controlled trial of effects on bone mineral density in healthy postmenopausal women. Bone 16: 469-476.
- Evans EM, Racette SB, Van pelt RE, Peterson LR, Villareal DT (2007) Effects of soy protein isolate and moderate exercise on bone turnover and bone mineral density in postmenopausal women. Menopause 14: 481-488.
- Gusi N, Raimundo A, Leal A (2006) Low-frequency vibratory exercise reduces the risk of bone fracture more than walking: a randomized controlled trial. BMC MusculoskeletDisord 7: 92.
- Kerr D, Morton A, Dick I, Prince R (1996) Exercise effects on bone mass in postmenopausal women are site-specific and load-dependent. J Bone Miner Res 11: 218-225.
- Stengel S, Kemmler W, Pintag R, Beeskow C, Weineck J, et al. ( 2005) Power training is more effective than strength training for maintaining bone mineral density in postmenopausal women. J App Physiol 99: 181-188.
- Von stengel S, Kemmler W, Kalender WA, Engelke K, Lauber D (2007) Differential effects of strength versus power training on bone mineral density in postmenopausal women: a 2-year longitudinal study. Br J Sports Med 41: 649-655.
- Wayne PM, Buring JE, Davis RB, Connors EM, Bonato P, et al. (2010) Tai Chi for osteopenic women: design and rationale of a pragmatic randomized controlled trial. BMC MusculoskeletDisord 11: 40.
- Wayne PM, Kiel DP, Buring JE, Connors EM, Bonato P, et al. (2012) Impact of Tai Chi exercise on multiple fracture-related risk factors in post-menopausal osteopenic women: a pilot pragmatic, randomized trial. BMC Complement Altern Med 12: 7.
- Ebrahim S, Thompson PW, Baskaran V, Evans K (1997) Randomized placebo-controlled trial of brisk walking in the prevention of postmenopausal osteoporosis. Age Ageing 26: 253-260.
- Preisinger E, Kerschan-Schindl K, Wöber C, Kollmitzer J, Ebenbichler G, et al. (2001) The effect of calisthenic home exercises on postmenopausal fractures--a long-term observational study. Maturitas 40: 61-67.
- Adami S, Gatti D, Braga V, Bianchini D, Rossini M (1999) Site-specific effects of strength training on bone structure and geometry of ultradistal radius in postmenopausal women. J Bone Miner Res 14: 120-124.
- Douchi T, Yamamoto S, Oki T, Maruta K, Kuwahata R, et al. (2000) The effects of physical exercise on body fat distribution and bone mineral density in postmenopausal women. Maturitas 35: 25-30.
- Fjeldstad C, Palmer IJ, Bemben MG, Bemben DA (2009) Whole-body vibration augments resistance training effects on body composition in postmenopausal women. Maturitas 63: 79-83.
- Kemmler W, Engelke K, Weineck J, Hensen J, Kalender WA (2003) Theerlangen fitness osteoporosis prevention study: a controlled exercise trial in early postmenopausal women with low bone density-first-year results. Arch Phys MedRehabil 84: P673-682.
- Kemmler W, Engelke K, Lauber D, Weineck J, Hensen J, et al. (2002) Exercise effects on fitness and bone mineral density in early postmenopausal women: 1-year EFOPS results. / Effets des exercicessur la santeet la densiteosseuse chez des femmes menopausees: resultats d ' un an d ' etude de l ' EFOPS. Med SciSportsExerc 34: 2115-2123.
- Kemmler W, Von stengel S, Bebenek M, Engelke K, Hentschke C, et al. (2012). Exercise and fractures in postmenopausal women: 12-year results of the Erlangen Fitness and Osteoporosis Prevention Study (EFOPS). OsteoporosInt 23: 1267-1276.
- Kerschan K, Alacamlioglu Y, Kollmitzer J, Wober C, Kaider A, et al. (1998) Functional impact of unvarying exercise program in women after menopause. Am J Phys Med Rehabil 77: 326-332.
- Kohrt WM, Ehsani AA, Birge SJ Jr (1997) Effects of exercise involving predominantly either joint-reaction or ground-reaction forces on bone mineral density in older women. J Bone Miner Res 12: 1253-1261.
- Maddalozzo GF, Widrick JJ, Cardinal BJ, Winters-stone KM, Hoffman MA, et al. (2007) The effects of hormone replacement therapy and resistance training on spine bone mineral density in early postmenopausal women. Bone 40: 1244-1251.
- Shen CL, Chyu MC, Yeh JK, Zhang Y, Pence BC, et al. (2012) Effect of green tea and Tai Chi on bone health in postmenopausal osteopenic women: a 6-month randomized placebo-controlled trial. OsteoporosInt 23: 1541-1552.
- Asikainen TM, Suni JH, Pasanen ME, Oja P, Rinne MB, et al. (2006)Effect of brisk walking in 1 or 2 daily bouts and moderate resistance training on lower-extremity muscle strength, balance, and walking performance in women who recently went through menopause: a randomized, controlled trial. PhysTher86: 912-923.
- Cao ZB, Tabata I, Nishizono H (2009) Good maintenance of physical benefits in a 12-month exercise and nutritional intervention by voluntary, home-based exercise: a 6-month follow-up of a randomized controlled trial. J Bone Miner Metab 27: 182-189.
- Carter ND, Khan KM, Petit MA, Heinonen A, Waterman C, et al. (2001) Results of a 10 week community based strength and balance training programme to reduce fall risk factors: a randomised controlled trial in 65-75 year old women with osteoporosis. Br J Sports Med 35: 348-351.
- Cheng S, Sipilä S, Taaffe DR, Puolakka J, Suominen H (2002) Change in bone mass distribution induced by hormone replacement therapy and high-impact physical exercise in post-menopausal women. Bone 31: 126-135.
- Karinkanta S, Heinonen A, Sievänen H, Uusi-Rasi K, Fogelholm M, et al. (2009) Maintenance of exercise-induced benefits in physical functioning and bone among elderly women. Osteoporosint 20: 665-674.
- Karinkanta S, Heinonen A, Sievänen H, Uusi-rasi K, Pasanen M, et al. (2007) A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: randomized, controlled trial. Osteoporosint 18: 453-462.
- Mayoux-Benhamou MA, Bagheri F, Roux C, Auleley GR, Rabourdin JP, et al. (1997) Effect of psoas training on postmenopausal lumbar bone loss: a 3-year follow-up study. Calcif Tissue Int 60: 348-353.
- Uusi-rasi K, Beck TJ, Sievanen H, Heinonen A,Vuori I (2003) Associations of hormone replacement therapy with bone structure and physical performance among postmenopausal women. Bone32: 704-710.
- Uusi-rasi K, Sievanen H, Heinonen A, Kannus P, Vuori I (2004a). Effect of discontinuation of alendronate treatment and exercise on bone mass and physical fitness: 15-month follow-up of a randomized, controlled trial. Bone 35: 799-805.
- Kilbreath S, Refshauge KM, Beith J, Ward L, Sawkins K, et al. (2011) Prevention of osteoporosis as a consequence of aromatase inhibitor therapy in postmenopausal women with early breast cancer: rationale and design of a randomized controlled trial. ContempClin Trials 32: 704-709.
- Mcguire R, Waltman N, Zimmerman L (2011) Intervention components promoting adherence to strength training exercise in breast cancer survivors with bone loss. West J Nurs Res 33: 671-689.
- Ott CD, Twiss JJ, Waltman NL, Gross GJ, Lindsey AM (2006) Challenges of recruitment of breast cancer survivors to a randomized clinical trial for osteoporosis prevention. Cancer Nursing, 29: 21-31.
- Saarto T, Sievanen H, Kellokumpu-lehtinen P, Nikander R, vehmanen L, et al. (2012). Effect of supervised and home exercise training on bone mineral density among breast cancer patients. A 12-month randomised controlled trial. OsteoporosInt 23: 1601-1612.
- Schwartz AL, Winters-stone K, Gallucci B (2007) Exercise effects on bone mineral density in women with breast cancer receiving adjuvant chemotherapy. Oncology Nursing Forum 34: 627-633.
- Swenson KK, Nissen MJ, Anderson E, Shapiro A, Schousboe J, et al. (2009) Effects of exercise vs bisphosphonates on bone mineral density in breast cancer patients receiving chemotherapy. J Sup Oncol 7: 101-107.
- Waltman NL, Twiss JJ, Ott CD, Gross GJ, Lindsey AM, et al. (2010b) The effect of weight training on bone mineral density and bone turnover in postmenopausal breast cancer survivors with bone loss: a 24-month randomized controlled trial. OsteoporosInt 21: 1361-1369.
- Winters-stone KM, Dobek J, Nail L, Bennett JA, Leo MC, et al. (2011) Strength training stops bone loss and builds muscle in postmenopausal breast cancer survivors: a randomized, controlled trial.Breast Cancer Res Treat 127: 447-456.
- Ríos-díaz J, Linares hevilla FJ, Martínez-payá JJ, Palomino cortés MÁ, Del bañoaledoME (2008) Arquitectura y organizacióninterna del hueso ante la aplicación de diferentesestímulosmecánicos. Fisioterapia 30:194-203.
- Tolomio S, Ermolao A, Lalli A, Zaccaria M (2010) The effect of a multicomponent dual-modality exercise program targeting osteoporosis on bone health status and physical function capacity of postmenopausal women. J women aging 22: 241-254.
- Verschueren SM, Bogaerts A, Delecluse C, Claessens AL, Haentjens P, et al. (2011) The effects of whole-body vibration training and vitamin D supplementation on muscle strength, muscle mass, and bone density in institutionalized elderly women: a 6-month randomized, controlled trial. J Bone Miner Res 26: 42-49.
- Bravo G, Gauthier P, Roy PM, Payette H, Gaulin P, et al. (1996) Impact of a 12-month exercise program on the physical and psychological health of osteopenic women. J Am Geriatrics Society 44: 756-762.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 4444
- [From(publication date):
February-2017 - Jan 18, 2025] - Breakdown by view type
- HTML page views : 3648
- PDF downloads : 796