Research Article Open Access
Excreta-Related Infections and the Role of Latrines to Control the Transmission in Ethiopia
Samuel F*Department of Medicine, Ambo University, Ambo, Ethiopia
- *Corresponding Author:
- Fikresilasie Samuel
Department of Medicine
Ambo University, Ambo, Ethiopia
Tel: +251929050512
E-mail: fikre16sam@gmail.com
Received date: June 15, 2016; Accepted date: October 13, 2016; Published date: November 30, 2016
Citation: Samuel F (2016) Excreta-related Infections and the Role of Latrines to Control the Transmission in Ethiopia. J Community Med Health Educ 6:496. doi: 10.4172/2161-0711.1000496
Copyright: © 2016 Samuel F. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Unimproved sanitation facilities and open defecation practices are common factors for the occurrence of excreta related infections (ERIs) in Ethiopia. These diseases can easily be controlled if every person uses a properly constructed and improved latrine system. Hence, the objective of this review is to assess the current status of ERIs and the role of latrines to control the transmission. Excreta related infections were high in burden as compared to the global situation. This is directly related to the access and use of improved sanitation facilities. In Ethiopia only 27% of the current population has access to improved latrines, which is below the expected outcome. Moreover, the reports showed inter-urban and urban-rural disparities in access to improved latrines. Reduction of ERIs morbidity was reported in different studies after latrine construction. In conclusion, it is already obvious that escalation of latrine coverage and awareness to the society about sanitation, maintenance of latrines improve the burden of these infections. Hence, government concerned bodies, health extension programmers and the society together should work to reduce sanitary related disease by scale up low cost sanitary technologies.
Keywords
Sanitation; Latrine; Infection control; Transmission
Introduction
Sanitation can be defined as the safe disposal of human excreta and associate hygiene practices or a safe toilet accompanied by hand washing with soap [1,2]. Human excreta are the source of many infectious disease agents. Diseases for which human excreta are the source are known as excreta borne diseases [3]. Hence, the provision of appropriate facilities for defecation is essential response for people’s dignity, safety, health and well-being [4].
Safe sanitation is widely acknowledged to be an essential groundwork for better health, welfare and economic productivity, but progress in reducing the burden of sanitation related diseases in developing countries remains slow [5]. Besides, social factors like poverty, ignorance, poor standards of living, overcrowding, etc. are exaggerating the situation. These factors are mainly responsible for the increased morbidity and mortality in these countries.
Excreta-related infections are the most important and wide spread problems in Ethiopia. The most important reason is the majority of the population; especially in rural areas do not have access to safe and civilized latrine system or improved sanitation facilities. As a result most of the population in rural areas and many villages defecate in open fields or in any available spaces. Human excreta contaminate the surface soil/field, food and water sources. The exposed excreta provide breeding places for flies and other insects. Flies carry from faeces infectious agents to food and finally reach the consumer with the food [3]. In unimproved latrines also, flies can access the latrine contents and serve as a mechanical transmitter of pathogens. The latrine contents can be used as a breeding site for flies, which may further contribute to disease transmission [6].
Furthermore, shared sanitation in the community could contribute to the transmission of diarrheal diseases caused by issues of cleanliness and maintenance, overuse, or caused by users occasionally opting for less hygienic means of excreta disposal [7]. For these reasons excreta borne diseases such as typhoid fever, shigellosis, amoebiasis; helminthic infections are very common and serious in the Ethiopia [3]. These diseases can easily be controlled if everybody uses a properly constructed and maintained latrine system. Therefore, the paper is planned to review current status of sanitary related infections and the role of latrines to control the transmission in Ethiopia using updated published articles done in the country as well as country profile documents reported by FMOH.
Review
Sanitation burden of the disease
Each year there are approximately 4 billion diarrhoea cases that cause 2.2 million deaths, mostly among children under the age of five. This means a rate of one child every fifteenth second, which is 15% of all of the death causes among the children under the age of five. Approximately 10% of the population in developing countries is affected by intestinal worms. Intestinal parasitic infections can lead to malnutrition, anemia and retarded growth. Six million people are blind from trachoma. It is the most common cause of blindness in the world. 200 million people in the world are infected with schistosomiasis, of which 20 million suffer severe consequences. Hundreds of millions of people suffer from different types of intestinal parasites annually [8-15].
As shown in Table 1 excretory related diseases in Ethiopia are high in burden as compared to the global cases. Studies from different part of the country showed that it is because of poor sanitary conditions in the country. High prevalence of shigellosis was reported from northwest Ethiopia in patents under five years of age. The study indicated that factors such as educational level, latrine usage, source of drinking water, and hand washing habits showed a statistically significant association with the prevalence of Shigella species [16-22].
| Diseases | Transmission mechanisms | Pathogen | Burden | |
| Global | Ethiopia | |||
| Cholera | Fecal-oral | Vibrio cholera | 1.4-4.3 mill | N |
| Typhoid | Fecal-oral | Salmonella typhi | >21 mill | - |
| shigellosis | Fecal-oral | Shigella | 164.7 mill | - |
| Rotavirus | Fecal-oral | Virus | 111 mill | - |
| Amoebiasis | Fecal-oral | Protozoa | 50 mill | - |
| Giardiasis | Fecal-oral | Protozoa | 2.8 ×10 8 | |
| Ascariasis | Fecal-oral | Helminths | 807 mill | 26 mill |
| Trichuriasis | Fecal-oral | Trichuristrichiura | 604 mill | 21 mill |
| Hookworms | Larval skin penetration | Ancylostomaduodenale and Necatoramericanus |
576 mill | 11 mill |
| Schistosomiasis | Water contamination | Parasitic worms | 207 mill | 5.01 mill |
| Guinea worm | Drinking contaminated water | Dracunculusmedinensis | 542 cases | 4 cases |
| Filariasis | Insect breed or feed in sites of poor sanitation |
Wuchereriabancrofti, Brugiamalayi or B. timori. | 120 mill | 30 mill at risk |
| Trachoma | Transmitted through contact with eye and nose discharge of infected person | Clamydia trachomatis | 84 mill | >65 millat risk |
| mill: Million | ||||
Table 1: Main diseases linked to unimproved sanitation and hygiene.
Occurrence of acute diarrhoea related with lack of latrine ownership, lack of home-based water treatment, lack of improved water sources and consumption of left-over food was reported in Southern Ethiopia [23]. Similarly in southwest Ethiopia, a populationbased cross-sectional study on diarrheal morbidity was carried out.
As a result, 66% of acute watery diarrhea, 20% of dysentery, and 14% of persistent diarrhea episodes were described by Teklemariam and others [24]. Besides, the prevalence of diarrhea among mothers and under-five children in Western Ethiopia was 8.2% and 18.0%, respectively [25].
Furthermore, trachoma is a public health problem in Ethiopia accounting for 35-50% of cases of blindness. Trachoma is endemic in southwest Ethiopia with active trachoma being a public health problem. The overall prevalence estimate of active trachoma was 25.2% in the study area [26]. Moreover, Prevalence of trachoma was found to be 12% in Mojo and Lume districts [27].
Intestinal worm infections are also common in developing countries, like Ethiopia. The study conducted by Fikreslasie and others report showed the high prevalence of schistosomiais, ascariasis, trichiuriasis and Hookworm infections in south Ethiopia. Most prevalent parasites were Schistosoma mansoni (61.0%), hookworm (51.3%), Ascaris lumbricoides (49.7%) and Trichuris trichiura (44.6%). Infections with Taenia spp. (1.3%), Enterobius vermicularis (1.7%), Strongyloides stercoralis (1.0%) and Hymenolepis nana (1.7%) were also observed [28].
Global sanitation coverage
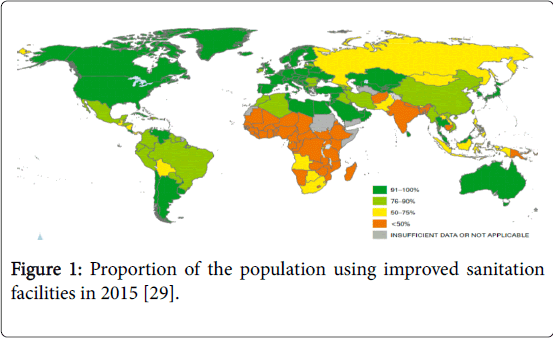
Nearly one third of the current global population (68%) has gained access to an improved sanitation facility since 1990, a total of 2.1 billion people. This means 82% of the global urban population and 51% of the rural population, uses improved sanitation facilities. However, the proportion gaining access varies across developing regions (Figure 1). Western Asia and Northern Africa have provided access to 50% and 41% of the current population since 1990, respectively. By contrast, Sub-Saharan Africa has provided access to less than 20% of the current population [29].
Ethiopia sanitation coverage
Currently Ethiopia is making progress to increase the sanitation coverage proportional to the current population. According to the government report, in the year 2000 less than 15% of the Ethiopian population had access to basic sanitation but now after the introduction of the Health Extension Package and widespread hygiene and sanitation promotion the Federal Ministry of Health (FMOH) 2008/9 reported that, the national coverage of sanitation has reached 60% (Table 2) [30].
| Region | Access to excreta disposal | ||
| No. of house holds | No. hose holds with latrines | Percent coverage | |
| Tigrai | 1,030,199 | 726’946 | 71 |
| Afar | 258,572 | 16,795 | 6.5 |
| Amhara | 4,209,129 | 2,644,417 | 63 |
| Oromia | 6,011,967 | 3,377,365 | 56 |
| Somali | 708,028 | 18,660 | 3 |
| BG | 158,156 | 32,473 | 21 |
| SNNPR | 3,272,573 | 2,444,862 | 75 |
| Gambella | 72,304 | 7,446 | 10 |
| Harari | 49,488 | 20,114 | 41 |
| Addis Ababa | 696,210 | 530,934 | 76 |
| Dire Dawa | 80,041 | 38,188 | 48 |
| National | 16,546,667 | 9,878,199 | 60 |
SNNPR: Southern Nations, Nationalities, and Peoples' Region
Table 2: Access to excreta disposal in Ethiopia [30].
According to FMOH report an average of more than 60% excreta disposal access is available in the country [30]. However, inter-region access to excrete disposal varies between 76% and 3% (Table 2). Addis Ababa, SNNPR and Tigrai regions have more than 70% latrine coverage. Dire Dawa, Harari, Gambella, BG, Somali and Afar regions have less than 50% latrine access. The highest and the lowest latrine access was reported from Addis Ababa and Somali regions, respectively. The difference in access to excreta disposal between regions has an impact on burden of excreta related infections in the country. It is obvious that societies in regions with less latrine coverage are more at risk of diarrheal diseases than other regions.
The escalation of access to excreta disposal in Ethiopia reduces the open defecation practice of the society significantly. Recently WHO reported that Ethiopia has achieved the largest decrease in the proportion of the population practicing open defecation (from 92% in 1990 to 29% in 2015), which is a reduction over five times greater than the regional average for the same period. Open defecation was practiced by 44.3 million Ethiopians in 1990 and nowadays in 2015 there are 28.3 million people who are practicing open defecation due to deficiency in facilities and malpractice. Similarly, the Southern Asia region, where the number of open defecators is highest, has also made significant improvements. Bangladesh, Nepal and Pakistan have all achieved reductions of more than 30 percentage points since 1990 [29]. However, the access possibly will not indicate the quality of sanitation facilities. According to WHO report, Ethiopia has not met the Millennium Development Goal (MDG) target like other least developed countries and has a moderate kind of progress to enhance improved sanitation facilities. The proportion of 2015 populations that gained access since 1990 is only 27%, which is below the expected outcome (<50%) (Table 3).
| Year | Improved latrines base on ratio | Use of an improved sanitation facility (%) | References | ||
| Urban | Rural | Urban | Rural | ||
| 1990 | - | - | 20 | 0 | [29] |
| 1998 | 49.2 | 3.1 | 54 | 4 | [33] |
| 1999 | 43.9 | 1.7 | 46 | 2 | [34] |
| 2000 | 55.2 | 3.8 | 57 | 5 | [35] |
| 2003 | 0.78 | 0.47 | 63 | 10 | [36] |
| 2004 | 55.5 | 9.5 | 64 | 11 | [37] |
| 2005 | 0.58 | 0.18 | 52 | 7 | [38] |
| 2015 | - | - | 27 | 28 | [29] |
Table 3: Urban rural improved latrine coverage in Ethiopia from 1990-2015.
Though it is below the expected outcome, Ethiopia had considerable progress to encourage increased access to and use of improved hygiene and sanitation through health extension workers using house to house methods, as well as newer community empowerment tools such as Community-Led Total Sanitation and Hygiene (CLTSH) [30]. One study conducted in northwest Ethiopia indicated that the progress seems to be achievable via Health Extension Package, and school children through motivating health extension workers to involve school teachers and children [31]. In general, as efforts to improve sanitation are being undertaken in the country, approaches should not only to meet coverage targets, but should also be implemented in a way that achieves uptake, reduces exposure, and delivers genuine health gains [32-38]. Facilities, installations and sanitary systems are expensive and require the effort of both the authorities and the WHO as well as rich countries contribution. Without contributions and aids, poor developing countries will continue to suffer.
Concerning to inter-urban and urban-rural disparities in access to improved latrines, the reports showed significant differences among years. As shown in Table 3 over 50% of urban residents of the country in the year 1998, 2000, 2003, 2004 and 2005 had access to an improved latrines, while it varies between 20% and 46% in the year 1990, 1999 and 2015. Similarly, the report showed a high level urban-rural disparity especially in some surveyed years. While about 64% of urban residents in 2004 were reported to use latrines, the ratio of access is only 11% for rural counterparts. Similarly, it varies between 57% and 5%; 63% and 10% in 2000 and 2003, respectively, in both cases in favor of urban residents. However, in 2015 the access to improved latrines is in ratio of 1 to 1, which is reported by WHO.
As clearly presented in Table 3, urban sanitation figures generally far outshine rural access. But, it is widely known that the poor, unplanned, densely populated areas are badly underserved. This density therefore poses a greater risk of contamination than thinly populated rural areas [39]. In general, the current sanitation coverage in Ethiopia is far from the MDG target and the majority of the populations, mainly the urban poor, are living in a polluted environment, exposed to water and sanitation-related diseases [40]. Regarding to use of improved sanitation facilities, the government report has a positive picture in the past years than 2015 data reported by WHO.
Importance of proper latrine utilization
Several studies have revealed that the incidence of many diseases is reduced when people have access to, and make regular use of effective basic private sanitary installations. It is important to keep pathogens out of the environment because many of these organisms are capable of surviving for long periods of time under different conditions. Therefore, effective excreta management at the household and community levels produces far ranging societal benefits by helping to protect water resources and the food supply from faecal contamination [41]. It results in the isolation or destruction of pathogenic material hence, a break in the transmission pathway.
Luby demonstrated the importance of toilet construction and hygiene promotion in controlling fly breeding, reducing diarrhoea by 23% and trachoma by 75% [42]. In addition, Epidemiological studies by Esrey and others report have shown use of latrines can reduce diarrhoea by 36% or more, cholera by 66%, and worm infestations by between 12 and 86% [43]. A recent comprehensive review of survey data from 172 countries result confirmed a strong association between access to sanitation and reduction of child mortality and morbidity. Sanitation access lowered the probability of children suffering from diarrhoea by 7-17%, and reduced mortality for children under five by 5-20%. The survey indicated that child morbidity and mortality are substantially lower for children with access to advanced sanitation technologies [44]. In the same way the reviewing result from 67 studies (includes 28 countries) showed that: there are median reductions of diarrhoea morbidity rates by 22% and mortality rate by 21% [45].
The escalation of an access to latrines and a good progress to improve the sanitation facilities in Ethiopia has significant effect on reduction of excretory related infections. Some studies conducted in the country revealed a positive association of the two factors. It increase school attendance, especially for girls, and help school children to learn better [46]. Beside, a study in Ethiopia pointed out that most of the interventions (including multiple interventions, hygiene and water quality) were found to significantly reduce the levels of diarrhoeal illness, with the greatest impact being seen for hygiene and household treatment interventions [47]. The study from North West Ethiopia confirmed these evidences: children living in households without latrine facilities were about 92% more likely to develop diarrhea than children living in households with such facilities [25]. In the same way from western Ethiopia children from the households disposing refuse in pit/burn were 69% less likely to have diarrhea compared to children from the households who claimed disposing their refuse indiscriminately in open field [48]. In some communities of Ethiopia a reduction in the prevalence of ocular chlamydia was also reported after latrine construction ended [49].
Challenges of Latrine Utilization
Limited sanitation options, high demand to sanitation facilities compounded by poverty are creating a major challenge to expand improved latrines in Ethiopia [39]. As well, availability of latrines can be affected by different factors such as, income level, frequency of visits by health workers, walking time from local health institutions, and distance from urban areas [50]. Economic reasons and hygiene education are also factors frequently reported. The following are confronting factors which mainly affect the progress.
Poverty
Poor access to sanitation disproportionately affects the poorest people in society. Data from the 2012 report by WHO shows how progress in achieving the MDGs for sanitation has been highly inequitable. Beyond economic inequalities, the burden of inadequate sanitation often falls disproportionately on the most vulnerable people living in developing countries [1]. These poor people are surviving on subsistence incomes. At this level of poverty, income is primarily spent on food and goods, with other items given low priority. It is difficult to convince these people to use their limited finances on sanitation when they have lived their entire life without it. Even when they are convinced that sanitation will be beneficially, the perceived high cost of installation keeps many people from adopting [51]. Furthermore, persistent drought conditions exacerbate poverty, increase indebtedness, and reduce funds available for water, latrines and soap. As a result the spread of latrine coverage is highly confronted [39].
Behavior
Findings showed that providing infrastructure does not ensure use when there are significant and culturally engrained behavioral barriers to using latrines [52]. Effective sanitation and hygiene programmes need to combine interventions to change behavior with the selection of the right technology. Changing behavior requires culturally sensitive and appropriate health education. People need to understand, in terms meaningful to their lifestyles and existing belief systems, why better health depends on the adoption of hygiene practices such as handwashing (after defecation, after handling babies’ faeces, and before cooking), on the use of latrines for safe disposal of faeces, and on safe storage and handling of drinking-water and food. Raising awareness of why sanitation and hygiene are important will often increase motivation to change harmful behaviors [46].
In Ethiopia with so many other critical needs at household, village, kebele, woreda, zonal, regional and federal levels, it is hardly surprising that sanitation rarely reaches the top five in priority assessments. It is often, unfortunately viewed as a luxury component of service delivery rather than as a preventive health intervention [37]. It is unfortunate that the wealthy and developed countries are still unaware and not practicing their share of the matter. It is better to understand that what affects some remote countries today may surely affect them tomorrow. On the other hand, latrines themselves may be viewed as dirty and evil places. It may be considered more sanitary to defecate in the fields away from the house. Existing traditions and beliefs also play a part in the reception of latrines. It is difficult to change long ingrained behaviors dictating defecation practices and without proper reinforcing people will revert to old habits [49].
Education
Well-designed education programmers to demonstrate the link between sanitation, hygiene, health and economic development can contribute to increasing demand for improved sanitation. Hygiene promotion campaigns are most effective among younger populations, and students can be targeted both as beneficiaries and as agents of behavioral change within their families and their communities. Hygiene education should be included in school curricula, together with the provision and maintenance of sanitation facilities at school premises. These are essential elements of marketing campaigns in schools. Education, especially for women, is also important because educated mothers are more likely to adopt healthy hygiene and sanitation behaviors and consequently have lower infant mortality rates in their households [46]. Besides, developed countries scholars must have their share in such conditions with the new findings and technology in hand. Relying on the self-obtainable resources will do but not enough. Support, share and participation of all community will do much better in such conditions.
Studies reported that under poor environmental conditions, mothers with primary education and above protected their children against diarrhea better than mothers with no education. Thus, implementing effective educational programs that emphasize environmental health and sanitation practices and encouraging female school enrolment would reduce childhood diarrheal morbidity in the region [53]. There is also high burden of water, sanitation and hygiene related diseases in people living HIV/AIDS, encouraging hygiene education and additional support for the provision of water, sanitation, and hygiene services is essential to these people [54].
Maintenance
Another frequent barrier to latrine adoption is difficulties in maintenance of latrines. The major maintenance problems are frequently related to emptying. It may requires extra costs that are difficult for families to afford. Besides, there are concerns with hygiene during emptying and the frequency with which it must be done [51]. Studies indicated that though the society has sufficient knowledge about safe hygienic practices, the knowledge is not properly utilized. A study in South Africa pointed out that maintenance of sanitary systems in numerous schools was very poor for the reason that school authorities were ignoring the importance of using clean toilets [55]. Such ignorance make unhealthy school environment.
Conclusion
Excreta-related infections are the most important and wide spread problems in Ethiopia. The progress in reducing the burden of these diseases is remains slow. The most important reason is the majority of the population; do not have access to safe and improved sanitation facilities, only 27% of the societies have improved sanitations. The remaining societies are at risk of these infections as a result of unimproved sanitation facilities. Though Ethiopia is doing considerable progress to encourage increased access to and use of improved hygiene and sanitation through health extension workers, MDG target has not met. Poverty, behavioral barriers to use latrines, lack of access to health education and maintenance problem were confronting factors frequently reported in different studies. In order to enhance sanitation services for all in the post-MDG era, urgent action is required that will establish proper monitoring and evaluation systems that can measure real access to improved sanitation facilities [40]. Finally, inadequate data on role of latrines and positive picture of government data, which contradicts with some findings, were the limitation of this review paper.
References
- Elisa R, Isabelle P (2012) Toilets for health: a report by the london school of hygiene and tropical medicine in collaboration with domestos.
- Federal democratic republic of ethiopia ministry of health (2015) Blended learning module for the health extension programme. hygiene and environmental health part1.
- Ababa A (2004) Federal democratic republic of ethiopia ministry of health construction usage and maintenance of sanitary latrine extension package.
- The Sphere Project (2011) Humanitarian charter and minimum standards in disaster response: minimum standards in water supply, sanitation and hygiene promotion.
- Water aid report (2011) The sanitation problem: What can and should the health sector do?
- Irish S, Aiemjoy K, Torondel B, Abdelahi F, Ensink JHJ (2013) Characteristics of latrines in central tanzania and their relation to fly catches. PLoS ONE 8: e67951.
- Fuller JA, Clasen T, Heijnen M, Eisenberg JN (2014) Shared sanitation and the prevalence of diarrhea in young children: evidence from 51 countries, 2001-2011. Am J Trop Med Hyg 91: 173-180.
- Huuhtanen S, Laukkanen A (2010) A guide to sanitation and hygiene in developing countries. Global dry toilet association of Finland Tampere.
- World Health Organization (2015) Cholera fact sheet.
- Crump JA, Luby SP, Mintz ED (2004) The global burden of typhoid fever. Bulletin of the World Health Organization 82: 346-353.
- KotloffKL, Winickoff JP, Ivanoff B, Clemens JD, Swerdlow DL, et al. (1999) Global burden of Shigella infections: implications for vaccine development and implementation of control strategies. Bulletin of the World Health Organization 77.
- Parashar UD, Hummelman EG, Bresee JS, Miller MA, Glass RI (2003) Global illness and deaths caused by rotavirus disease in children. Emerg Infect Dis 9: 565-572.
- Dhawan VK, Cleveland KO, Cantey JR (2016) Amebiasis.
- Pestehchian N, Rasekh H, Babaei Z, Yousefi HA, Eskandarian AA, et al. (2012) Identification of genotypes of giardia duodenalis human isolates in isfahan, iran, using polymerase chain reaction - restriction fragment length polymorphism. Adv Biomed Res 1: 84.
- Bethony J, Brooker S, Albonico M, Geiger SM, Loukas A, et al. (2006) Soil-transmitted helminth infections: ascariasis, and hookworm. Lancet 367: 1521-1532.
- Hotez PJ, Kamath A (2009) Neglected tropical diseases in sub-saharan Africa: review of their prevalence, distribution and disease burden. PLoSNegl Trop Dis 3: e412.
- Steinmann P, Keiser J, Bos R, Tanner M, Utzinger J (2006) Schistosomiasis and water resources development: sytematic review, meta-analysis and estimates of people at risk. Lancet Infect Dis 6: 411-25.
- Hopkins DR, Ruiz-Tiben E, Weiss A, Withers PC , Eberhard ML, et al. (2013) Dracunculiasis eradication: and now, south sudan. Am. J Trop Med Hyg 89: 5-10.
- Ottesen EA (2006) Lymphatic filariasis: treatment, control and elimination. AdvParasitol 61: 395-441.
- ITI (2007) International Trachoma Initiative.
- World Health Orgaization (2008) Global alliance for the elimination of blinding trachoma database. Glob Health atlas.
- Aragaw M, Tafese T, Beyene Z, Hailemariam Z, Azaze A, et al. (2016) Shigellosis outbreak at addisababa university: march-april 2010. Ethiop Med J 49: 341-348.
- Godana W, Mengistie B (2013) Determinants of acute diarrhoea among children under five years of age in Derashe District, Southern Ethiopia. Rural Remote Health 13: 2329.
- Teklemariam S, Getaneh T, Bekele F (2000) Environmental determinants of diarrheal morbidity in under-five children, Keffa-Sheka zone, South West Ethiopia. Ethiop Med J 38: 27-34.
- Muluken D, Abera K, Worku T (2011) Predictors of under-five childhood diarrhea: Mecha District, West Gojam., Ethiopia. Ethiop J Health Dev 25: 192-200.
- Ejigu M, Kariuki MM, Ilako DR, Gelaw Y (2013) Rapid trachoma assessment in Kersa District, Southwest Ethiopia. Ethiop J Health Sci 23: 1-9.
- Yalew KN, Mekonnen MG, Jemaneh AA (2012) Trachoma and its determinants in Mojo and Lume districts of Ethiopia. Pan Afr Med J 13: 8.
- Samuel F, Degarege A, Erko B (2014) Efficacy and side effects of albendazole currently in use against Ascaris, Trichuris and hookworm among school children in Wondo Genet, southern Ethiopia. ParasitolInt 63: 450-455.
- World Health Organization (2015) Progress on sanitation and drinking water-2015 update and mdg assessment.
- Federal Democratic Republic Of Ethiopia Ministry Of Health (2011) Final National Hygiene & Sanitation Strategic Action Plan for Rural, Per-Urban & Informal Settlements in Ethiopia. Addis Ababa, Ethiopia.
- Gedefaw M, Amsalu Y, Tarekegn M, Awoke W (2015) Opportunities, and challenges of latrine utilization among rural communities of Awabel district, northwest Ethiopia, 2014. Open J Epidemiol 5: 98-106.
- Clasen T, Boisson S, Routray P, Torondel B, Bell M, et al. (2014) Effectiveness of a rural sanitation programme on diarrhoea, soil-transmitted helminth infection, and child malnutrition in Odisha, India: a cluster-randomised trial. Lancet Glob Health 2: e645-653.
- Central Statistical Authority (2011) Welfare monitoring survey 1998.
- Ethiopia Ministry of Economic Development and Cooperation (1999) Poverty situation in Ethiopia.
- Central Statistical Authority (2001) Ethiopia demographic and health survey.
- World Health Organization (2003) World health survey.
- Central Statistical Authority (2004) Welfare monitoring survey 2004.
- Central Statistical Authority (2005) Ethiopia demographic and health survey 2005.
- Federal Democratic Republic of Ethiopia (2005) Ministry of health national hygiene and sanitation strategy: to enable 100% adoption of improved hygiene and sanitation.
- Beyene A, Hailu T, Faris K, Kloos H (2015) Current state and trends of access to sanitation in Ethiopia and the need to revise indicators to monitor progress in the Post-2015 era. BMC Pub Health 15: 451.
- Carr R, Strauss M (2001) Excreta-related infections and the role of sanitation in the control of transmission. Water Quality: Guidelines, Standards Health.
- Pitet D (2005) Clean hands reduce the burden of disease cited. Lancet 366: 185-187.
- Esrey SA, Potash JB, Roberts L, Shiff C (1991) Effects of improved water supply, sanitation and hygiene. Bulletin of the Royal Society of Tropical Medicine and Hygiene. 77: 5151-5521.
- Gunther I, Fink G (2010) Water, sanitation, and children’s health: evidence from 172 dhs surveys. World Bank Policy Research Working Paper No. 5275, Washington DC, USA.
- Esrey SA, Feachem RG, Hughes JM (1985) Interventions for the control of diarrhoeal diseases among young children: improving water supplies and excreta disposal facilities. Bull World Health Organ 63: 757-772.
- World Health Organization (2004) The Sanitation Challenge: Turning commitment into reality.
- Fewtrell L, Colford JM (2005) Water, sanitation and hygiene in developing countries: interventions and diarrhoea-a review. Water SciTechnol 52: 133-142.
- Girma R, Wondwossen B, Bishaw D, Tefera B (2008) Environmental determinants of diarrhea among under-five children in Nekemte Town, Western Ethiopia. Ethiop J Health Sci 18: 39-45.
- Haile M, Tadesse Z, Gebreselassie S, Ayele B, Gebre T, et al. (2013) The association between latrine use and trachoma: a secondary cohort analysis from a randomized clinical trial. Am J Trop Med Hyg 2013 89: 717-720.
- Awoke W, Muche S (2013) A cross sectional study: latrine coverage and associated factors among rural communities in the District of Bahir Dar Zuria, Ethiopia. BMC Public Health 4: 13-99.
- Conville JM (2003) How to Promote the Use of Latrines in Developing Countries. Michigan Technological University, Master’s International Program.
- Routray P, Schmidt WP, Boisson S, Clasen T, Jenkins MW (2015) Socio-cultural and behavioural factors constraining latrine adoption in rural coastal odisha: an exploratory qualitative study. BMC Public Health 15: 880.
- Sinmegn MT, Asres AG, Shimeka TA (2014) Determinants of childhood diarrhea among underfive children in BenishangulGumuz Regional State, North West Ethiopia. BMC Pediatr 14: 102.
- Yallew WW, Terefe MW, Herchline TE, Sharma HR, Bitew BD, et al. (2012) Assessment of water, sanitation, and hygiene practice and associated factors among people living with HIV/AIDS home based care services in Gondar city, Ethiopia. BMC Public Health 12: 1057.
- Sibiya JE, Gumbo JR (2013) Knowledge, attitude and practices (KAP) survey on water, sanitation and hygiene in selected schools in Vhembe District, Limpopo, South Africa.Int J Environ Res Public Health 10: 2282-2295.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 13050
- [From(publication date):
December-2016 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 11368
- PDF downloads : 1682