Evidence Based Approach of Emphysematous Pyelonephritis: A Case Report
Received: 02-Jun-2022 / Manuscript No. cpb-22-65783; / Editor assigned: 06-Jun-2022 / PreQC No. cpb-22-65783(PQ); / Reviewed: 20-Jun-2022 / QC No. cpb-22- 65783; / Revised: 23-Jun-2022 / Manuscript No. cpb-22-65783(R); / Accepted Date: 30-Jun-2022 / Published Date: 30-Jun-2022 DOI: 10.4172/2167-065X.1000270
Abstract
This is a case report of a 64-year-old man with Type 2 diabetes mellitus who was presented with symptoms of fever, vomiting, and flank pain. The patient was diagnosed with Emphysematous pyelonephritis (EPN). Emphysematous pyelonephritis is a serious, acute necrotizing renal parenchymal and perirenal infection with the formation of gas. Uncontrolled diabetes mellitus, obstruction of the urinary tract are the main predisposing factors and Escherichia Coli is the most frequent causative pathogen. Computed Tomography (CT) scan revealed well-defined emphysematous right pyelonephritis, urethritis, and cystitis. Imaging revealed the presence of extensive gas in the renal parenchyma prompting the use of broad-spectrum antibiotics and percutaneous drainage as a part of a conservative management regimen. The patient made a full recovery and was discharged 15 days after admission.
Introduction
Emphysematous pyelonephritis (EPN) is an acute life-threatening infection defined by the presence of gas in the renal system, most commonly in the parenchyma but also in the perinephric tissues [1]. First described by Kelly and MacCullum in 1898, the majority of cases (over 90%) are seen in diabetics; other risk factors include urinary tract obstruction, neurogenic bladder, alcoholism, and anatomic deformity[2].
Escherichia coli is the most common causal pathogen isolated in urine or pus culture in approximately 70% of reported cases along with other microorganisms like Klebsiella, Clostridium, Candida, Aspergillus, Cryptococcus and Amoeba [3]. Antibiotics with a broad spectrum of coverage should be used aggressively. Early intervention with nephrectomy was also considered a need with developments in interventional radiology and the introduction of stronger antibiotics; nephrectomy is reserved for patients who do not respond to conservative therapy [4]. Usual presentation of emphysematous pyelonephritis is similar to those of pyelonephritis, including fever, chills and loin pain [5]. Although renal, perirenal gas can be detected on a conventional KUB film or with ultrasonography; the CT scan is the preferred method for diagnosis and staging. It also aids in the diagnosis of urinary tract obstructions and stones [6].
The presented case is a classic case of emphysematous pyelonephritis with diabetes mellitus that necessitated strong antibiotic therapy and care.
Case presentation
A 64 year old male patient was admitted in the Nephrology department with complaints of right loin and flank pain for a week. Associated symptoms include fever, vomiting and strangury along with pneumaturia. Patient was a known case of diabetic for the past ten years and was on treatment with oral anti diabetics. On admission he was well oriented. On general examination the patient was febrile (Temp 100.2F), Blood Pressure 140/90 mmHg, PR- 78/min, RR: 24/min and SPO2 96% in RA. Basic investigation on admission revealed high blood sugar levels (RBS 399 mg/dl, HbA1C 12.1 %), WBC 24.27(Polymorphs 87%, Lymphocytes 6 % and Monocytes 7%). Patient was moderately hyponatremic with Na level 120 mmol/L. Urinalysis revealed traces of protein, Glucose +++, Ketones++. Presence of bacteria was evident in urine. Creatinine was 1.40 mg/dl and liver parameters were unremarkable.
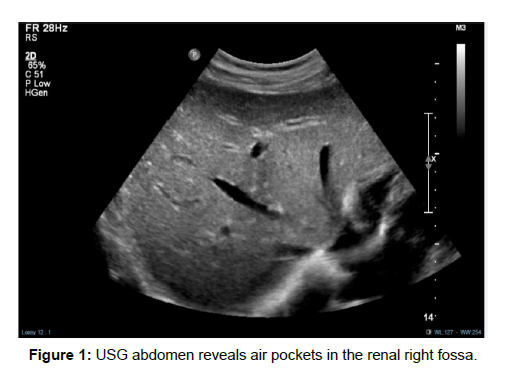
Considering a diagnosis of complicated UTI, the patient was started on Inj. Meropenem 1gm TID till blood cultures were obtained. Electrolyte imbalance and hyperglycemia levels were also corrected at the same time. An USG of the abdomen (Figure 1) revealed air pocket
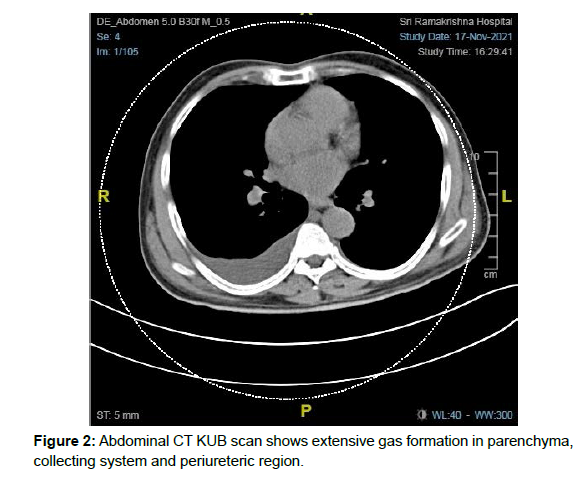
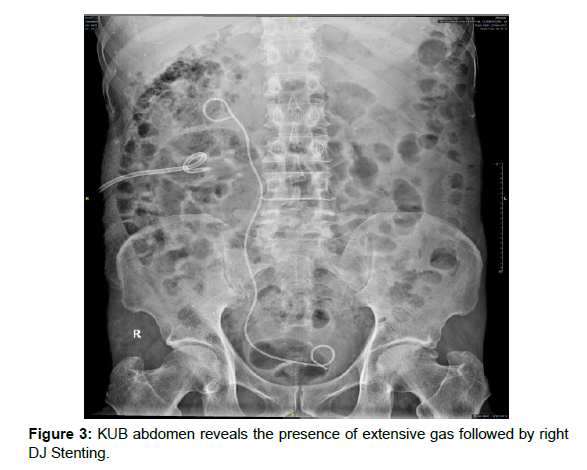
in the right renal fossa as well as urinary bladder and right kidney was not clearly delineated. Thus the patient was provisionally diagnosed as Emphysematous right pyelonephritis with cystitis. To confirm the diagnosis and to rule out the obstruction a non- contrast CT was done (Figure 2) which confirmed extensive gas formation in renalGram staining of the urine revealed the presence of Gram negative bacilli and blood culture was obtained which confirmed the offensive organism as extended spectrum Beta Lactamase (ESBL) Escherichia coli which was sensitive to meropenem which was continued. During the course of therapy urologists were consulted for PCN procedure which was done uneventfully followed by later Right DJ stenting (Figure 3).
Clinically, the patient began to improve , his sugar levels were brought under control (RBS 132 mg/dl) and his sodium levels improved from 120 mmol/L to 133 mmol/L. WBC counts were drastically improved from 24.27/mm3 to 10.43/mm3 and creatinine value reduced to 1.04 mg/dl from 1.4 mg/dl.
The patient was discharged under stable conditions after 15 days of intravenous Meropenem. He was stepped down to oral antibiotic for 10 days with instructions to return to the nephrology outpatient department for follow-up. Patient visited the OP as advised after a week and was clinically improved and recovered with a serum creatinine of 1.07 mg/dl. The patient remained asymptomatic all along.
Discussion
Emphysematous pyelonephritis is a rare upper urinary tract necrotizing illness. Mortality rates have been reported to be as high as 40–50%. EPN with EC (emphysematous cystitis) is a rare variant of EPN [7].
Haung et al. adopted a modified staging system, based on CT findings, as four classes correlated with severity
→Class 1: Gas presence in the collecting system only(emphysematous pyelitis)
→Class 2: Gas presence in the renal parenchyma without extension to the extra renal area
→Class 3A: Gas and or abscess presence in the perinephric space
→Class 3B: Gas or abscess presence in the pararenal area; and
→Class 4: Bilateral EPN of any class or EPN in a solitary kidney [8].
Predisposing factors include diabetics, presence of glucosefermenting bacteria, impaired vascular supply with poor kidney perfusion, and impaired immunity. In non-diabetic patients obstruction of the urinary tract is the underlying factor [4]. Factors which are related to high mortality are systolic blood pressure <90 mmHg, altered mental status, increase in serum creatinine, thrombocytopenia, bilateral disease. In more severe conditions, an acute renal failure or a septic shock can occur [2].
Confirmation of the diagnosis is by radiologic study. Plain X-ray abdomen can be more specific than sonography in detecting air in the renal collecting system but both have limitations because of superimposition of gas from the bowel or retro peritoneum. CT abdomen is a more specific and sensitive tool, and has been recommended as the most useful diagnostic modality of choice [4].
As evidence based approach, according to an investigation conducted by Jeng-Jong Huang and Chin-Chung Tseng, it is revealed that for localized EPN (class 1 and 2); PCD combined with antibiotic treatment can provide a good outcome [9].
The mainstay of treatment depends on clinical scenario and aforementioned classification. It includes intravenous antibiotics according to local clinical approach and usually double J stent insertion, percutenous drainage or even nephrectomy [5]. According to a case report by Stuart Deoraj, Fady Zakharious, on Emphysematous pyelonephritis: outcomes of conservative management and literature review, it concluded that a conservative management with 6 weeks of meropenem resulted in complete clinical and biochemical resolution of symptoms with no further relapses [10].
Our patient management strategy was similar and based on the results of the lab investigation and reports. The patient was started on Inj Meropenem on an empirical basis and then continued based on the culture results. Percutaneous drainage and right DJ stenting was performed .This strategy is associated with a lower mortality than medical management or emergency nephrectomy. Delayed elective nephrectomy may be eventually required in some patients. The advantages of percutaneous drainage include increased patient stability for subsequent reversal of some of the underlying contributory factors [3].
Conclusion
EPN is a rare necrotizing infection that is associated with a significant mortality and morbidity. The development of EPN is aided by uncontrolled diabetes, anatomical abnormalities and urinary tract blockage. CT scan is the modality of choice in the diagnosis. The mortality rate is reported to be 13.5% for emphysematous pyelonephritis [5]. which can be controlled with the aggressive use of appropriate antibiotics and minimal invasive techniques. Our case study clearly shows that in patients with severe infection and comorbities, clinical suspicion, early diagnosis and Intensive antimicrobial therapy along with early intervention will significantly improve the clinical result.
Acknowledgement
I would like to acknowledge the immense support of my Doctor, Nephrology department and clinical pharmacy department.
Declaration of patient consent
The author attests to having gotten all necessary patient consent papers. The patient understands that his name and initials will not be published, and that while every effort will be taken to keep his identity hidden, complete anonymity cannot be guaranteed.
References
- Mohamed AH, Mohamud HA (2020) Emphysematous pyelonephritis caused by candida species: A case report and outcome of 1 year follow-up. Urol Case Rep 1: 101113.
- Yao J, Gutierrez OM, Reiser J (2007) Emphysematous pyelonephritis. Kidney Int 71: 462-465.
- Arsene C, Saste A, Arul S, Mestrovich J, Kammo R, et al. (2014) A case series of emphysematous pyelonephritis. Clin Med Case Rep
- Nasr AA, Kishk AG, Sadek EM, Parayil SM (2013) A case report of emphysematous pyelonephritis as a first presentation of diabetes mellitus. Iran Red Crescent Med J 15.
- Yeung AM, Cheng CH, Chu PS, Man CW, Chau H, et al. (2019) A rare case of asymptomatic emphysematous pyelonephritis. Urol Case Rep 1: 100962.
- Mohsin N, Budruddin M, Lala S, Al Taie S (2009) Emphysematous pyelonephritis: a case report series of four patients with review of literature. Renal failure 31: 597-601.
- Li S, Wang J, Hu J, He L, Wang C, et al. (2018) Emphysematous pyelonephritis and cystitis: A case report and literature review. Int J Med Res 46: 2954-2960.
- Mazumder P, Al Khouja F, Moeller J, Lahham S (2021) A Case Report on Distinguishing Emphysematous Pyelitis and Pyelonephritis on Point-of-care Ultrasound. Clin Pract Cases Emerg Med 5: 35.
- Huang J, Tseng C (2000) Emphysematous Pyelonephritis. Arch Intern Med 160: 797-805.
- Chávez Valencia V, Orizaga de La Cruz C, Aguilar-Bixano O, Lagunas Rangel FA (2020) Coexistence of emphysematous cystitis and bilateral emphysematous pyelonephritis: a case report and review of the literature. Cen Case Rep 9: 313-317.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Mathew L (2022) Evidence Based Approach of Emphysematous Pyelonephritis: A Case Report. Clin Pharmacol Biopharm, 11: 270. DOI: 10.4172/2167-065X.1000270
Copyright: © 2022 Mathew L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1699
- [From(publication date): 0-2022 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 1344
- PDF downloads: 355