Research Article Open Access
Evaluation of Dentofacial Changes and Teporomadibular Joint Status of Mentally Challenged Individuals Attending Special Schools in Vadodara District, Gujarat,India
Sachin Chaware1*, Vrushali Thakare2 and Ajith Krishnan CG3
1Department of Prosthodontics, MGV KBH Dental College and Hospital, Panchavati, Nasik, Maharashtra, India
2Department of Public Health Dentistry, MGV KBH Dental College and Hospital, Panchavati, Nasik, Maharashtra, India
3Department of Public Health Dentistry, K.M. Shah Dental College & Hospital, Piparia, Vadodara, Gujarat, India
- *Corresponding Author:
- Dr. Sachin Chaware
Mango 602, Dream City
Takli Road, Nasik Road
Nasik, Maharashtra, India
Tel: 919405310342
E-mail: sac32in@yahoo.in
Received Date: July 22, 2014; Accepted Date: September 23, 2014; Published Date: September 26, 2014
Citation: Chaware S, Thakare V, Krishnan A (2014) Evaluation of Dentofacial Changes and Teporomadibular Joint Status of Mentally Challenged Individuals Attending Special Schools in Vadodara District, Gujarat, India. J Oral Hyg Health 2:164. doi:10.4172/2332-0702.1000164
Copyright: © 2014 Chaware S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
Objectives: A cross sectional study was conducted to investigate the Dentofacial changes and TMJ status and of mentally challenged individuals attending special schools in Vadodara District, Gujarat India.
Materials & Methods: A total of 277 individuals were surveyed of which 205 were males and 72 were females.The data was collected by using the WHO 1997 methodology.
Results: Clicking was the only positive finding observed for TMJ and it was seen in 11.02% of the study subjects. Tenderness and reduced jaw mobility was not seen among any of the study subjects. Crowding and spacing of anterior teeth was seen in 47.95% and 33.91% of the study subjects respectively. Anterior open bite was seen in 8.18% of the study subjects Molar discrepancy of half a cusp mesial or distal to normal was seen in 25.73% of the study subjects and 24.56% of the study subjects had molar discrepancy of one cusp or more mesial or distal to that of normal. Definite malocclusion was seen in 19.29%, severe malocclusion in 24 (14.03%) study subjects and 33 (19.29%) subjects had very severe malocclusion.
Conclusions: Dentofacial changes and TMJ status of Mentally Challanged Individuals attending special school in Vadodara District, Gujarat, India is poor with a greater deficit between the needs and services availability.
Keywords
Dentofacial changes; Mentally challenged individuals; Temporomandibular joint
Introduction
Mentally challenged individuals have an intellectual ability significantly lower than average and limited ability to adapt to the environment. Mental disability is a general term used when an individual’s intellectual development is significantly lower than average and his or her ability to adapt to the environment is consequently limited [1]. According to American Association of Mental Retardation (AAMR), mental retardation is a disability that occurs before age 18. It is characterized by significant limitations in intellectual functioning and adaptive behaviour as expressed in conceptual, social and practical adaptive skills [2,3]. Mentally challenged subjects are found in all societies of the world. Globally, the prevalence is estimated to be 30 per thousand [4]. Data related to prevalence of mentally challenged subjects in India is very rare. According to the National Sample Survey Organization in India, in 1991, out of 1000 children in the rural areas, 31 had some developmental delays, whereas in urban areas 9 out of every 1000 children were developmentally delayed [5]. Mentally challenged subjects may have impaired mobility, neuromuscular problems (drooling, gagging and swallowing problems), uncontrolled body movements, gastroesophageal reflux or seizures etc. They may also exhibit delay in language development, deficits in memory skills and are at a greater risk for health problems, require extra help and rely on others to achieve and maintain good health. Oral health is not an exception to this and may result into inadequate oral care and put them at higher risk for developing oral health problems [6-9].
Evaluation of occlusal dysfunction, several studies have reported that high prevalence of crowding, spacing, missing and irregularities associated with maxillary and mandibular teeth [9-11]. Significant prevalence of anterior open bite and cross bite was reported by Asokan et al. [12], whereas, Adenubi et al. [13] 40 reported 15% of subjects with malocclusion of which 40% had anterior open bite, and 10% had anterior cross bite. Similar status was reported by Vigilid [14]. Oredugba and Akindayomi [9] reported highest prevalence of Angle’s class I malocclusion followed by Angle’s class II and Angle’s class III. Svatun and Heloe [15] reported Angles class III malocclusion in 16% of the mentally challenged. Oredugba [16] reported 51% of the study subjects with Down syndrome to have Class I malocclusion. Mestrovic et al. [17] reported class III malocclusion in 43.8% of the study subjects. Regarding temporomandibular joint dysfunction, significant prevalence temporomandibular joint click was reported by Asokan et al. [18]. The similar finding was reported by Bhowate and Dubey [19] and Desai et al. [20]. It has been observed from the available literature that Dentofacial changes and TMJ Status of mentally retarded individuals have received very little attention. Surprisingly scares information is available on the Dentofacial changes and TMJ Status of these individuals and no such information could be retrieved for Vadodara District. More studies are thus essential to facilitate the integration of dental preventive regimens into the treatment protocol in order to establish desirable preventive measures and oral health care. Hence the present study was carried out to investigate the Dentofacial changes and TMJ status and of mentally challenged individuals attending special schools in Vadodara District.
Materials and Methods
A cross sectional study was conducted to assess Dentofacial changes and TMJ Status of mentally challenged individuals attending special schools in Vadodara city. Prior to the start of the study, permission was taken from the concerned authorities after explaining purpose and procedure of the study. A voluntary informed verbal consent was taken from each study subject before examination. The oral examination of the study subjects was carried out using Basic Oral Health Surveys, WHO 1997 criteria [21]. WHO Oral Health Assessment forms were used to record the data. The examination was carried out by a single examiner, trained and calibrated prior to the study and recorded by a trained recording clerk.
Inclusion criteria
1) All the mentally challenged individuals attending special schools in Vadodara City.
2) Sex: Both the genders males as well as females were included.
Exclusion criteria
1) Study subjects who are contraindicated for examination.
2) Study subjects with previous history of obnoxious behaviour as informed by the school authority
3) Study subjects for whom permission was not granted by the authorities.
Examination Procedure
The demographic data of the study subjects was recorded by the trained personal. The study subject was then made to sit on a comfortable chair. The oral examination was carried out by the single examiner and the data was recorded by the recorder. Clinical findings were reported to the authorities of special schools at the end of the examination procedure. A health talk was given to the study subjects, teachers of respective special schools after completion of data collection.
Observations and Results
There are a total of nine special schools for mentally challenged individuals in Vadodara District, of which eight were included in our study as one of the institutions was not willing to participate in the study. Out of total 294 study subjects in the eight institutions, oral examinations of 277 study subjects were carried out using WHO 1997 criteria. Remaining 17 subjects could not be examined because of severe uncooperative behaviour or not being present on the day of examination and hence were excluded from the analysis.
Distribution of the study subjects
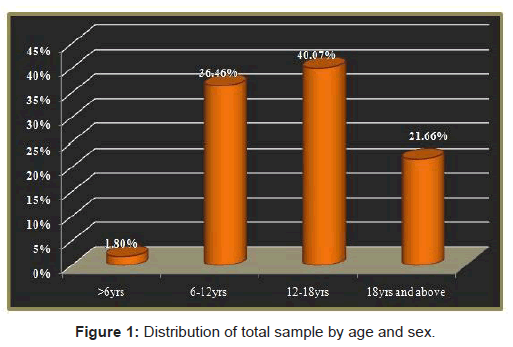
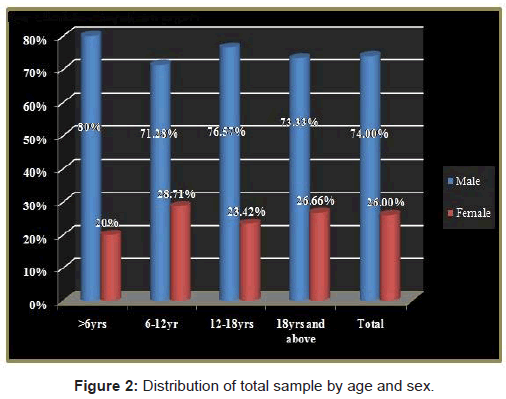
Table 1, Figures 1 and 2: Distribution of total sample by age and sex
There were total 277 study subjects with age range of 4 years to 30 years and mean age of 13.84 + 5.24 yrs. Out of 277 study subjects, 205 (74.00%) were males and 72 (26.00%) were females. Percentage of males was higher than females in all the three age groups. There were 5 (1.80%) subjects in the age group of below 6 years, 101 (36.46%) subjects in the age group of 6-12 years, 111 (40.07%) subjects in the age group 12- 18 years and 60 (21.66%) subjects in age group of above 18 years.
| Age Group(Yrs) | Male (%) | Female (%) | Total (%) |
|---|---|---|---|
| Below 6 yrs | 4 (80.00%) | 1 (20.00%) | 5(1.80%) |
| 6-12 yrs | 72 (71.28%) | 29 (28.71%) | 101 (36.46%) |
| 12-18 yrs | 85 (76.57%) | 26 (23.42%) | 111 (40.07%) |
| 18 yrs and above | 44 (73.33%) | 16 (26.66%) | 60 (21.66%) |
| Total | 205 (74.00%) | 72 (26.00%) | 277 (100.00%) |
Table 1: Distribution of total sample by age and sex.
Temporomandibular joint finding
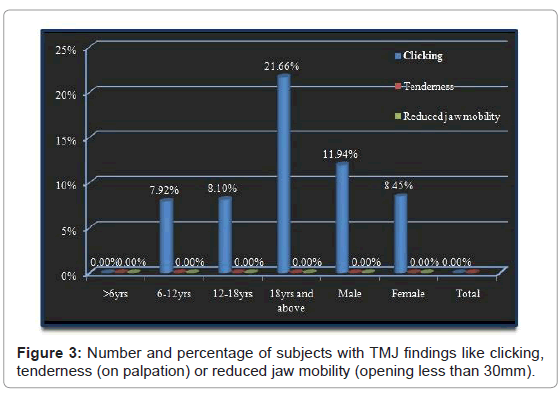
Table 2 and Figure 3: Number and percentage of subjects with TMJ findings like clicking, tenderness (on palpation) or reduced jaw mobility (opening less than 30mm)
Temporomandibular joint was examined for clicking, tenderness (on palpation) or reduced jaw mobility (opening less than 30 mm). Number and percentage of subjects with TMJ findings have been presented in Table 2 and Figure 3. Clicking was the only positive finding recorded in all the age groups except those below 6 years. It was seen in 30 (11.02%) study subjects had clicking at the time of examination. Percentage of clicking increased with age and was highest in the age group above 18 years. This difference was significant statistically. (P=0.002)
| TMJ condition | Clicking | Tenderness | Reduced jaw mobility | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Age group | M n/% | F n/% | T n/% | M n/% | F n/% | T n/% | M n/% | F n/% | T n/% |
| Below 6yrs | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 |
| 6-12 yrs | 6 8.33 | 2 6.89 | 8 7.92 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 |
| 12-18yrs | 7 8.23 | 2 7.69 | 9 8.10 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 |
| 18-30 yrs | 11 25.00 | 2 12.50 | 13 21.66 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 |
| Total | 24 11.94 | 6 8.45 | 30 11.02 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 | 0 0.00 |
| χ2= | |||||||||
Table 2: Number and percentage of subjects with clicking tenderness (on palpation) or reduced jaw mobility (opening less than 30mm).
Table 3 : Number and percentage of subjects with crowding, spacing, diastema, anterior maxillary and mandibular irregularity Crowding was seen in 82 (47.95%) and 58 (33.91%) subjects had spacing of anterior teeth. 28 (16.37%) study subjects had midline diastema. Anterior maxillary and mandibular irregularity was present respectively in 70 (40.93%) and 68 (39.76) study subjects.
| Age Group | Crowding n (%) | Spacing n (%) | Diastema n (%) | Ant maxillary irregularity n (%) | Ant mandibular irregularity n (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 12-17yrs (n= 111) | 60 (54.05) | χ2= 3.427 df = 1 P = 0.064 NS |
33 (29.72) | χ2= 1.757 df = 1 P = 0.185 NS |
11 (9.90) | χ2 = 9.654 df = 1 P = 0.002 HS |
49 (44.14) | χ2 = 1.347 df = 1 P = 0.246 NS |
45 (40.54) | χ2= 0.028 df = 1 P = 0.867 NS |
|
| 18-30yrs (n=60) | 22 (36.66) | 25 (41.66) | 17 (28.33) | 21 (35.00) | 23 (38.33) | ||||||
| Gender | |||||||||||
| Male (M=129) | 61 (42.28) | χ2= 0.392 df = 1 P = 0.531 NS |
45 (34.88) | χ2 =0.002 df = 1 P = 0.967 NS |
21 (16.27) | χ2= 0.354 df = 1 P = 0.552 NS |
52 (40.31) | χ2= 0.411 df = 1 P =0.521 NS |
48 (37.20) | χ2= 2.027 df = 1 P = 0.155 NS |
|
| Female (F=42) | 21 (50.00) | 13 (30.95) | 7 (16.66) | 18 (42.85) | 20 (47.61) | ||||||
| Total (n= 171) | 82 (47.95) | 58 (33.91) | 28 (16.37) | 70 (40.93) | 68 (39.76) | ||||||
Table 3: Number and percentage of subjects with crowding, spacing, diastema, anterior maxillary and mandibular Irregularity.
Table 4: Number and percentage of subjects with maxillary and mandibular overjet, open bite and antero-posterior molar relationship.
Maxillary over jet was present in 135 (78.94%) study subjects, mandibular over jet (cross bite) in 13 (7.60%) and openbite in 14 (8.18%) study subjects. Remaining 9 (5.28%) study subjects had edge to edge bite. 85 (49.70%) subjects had normal anterio-posterior molar relation. 44 (25.73%) study subjects had lower first molar that is half a cusp mesial or distal to its normal relation and 42 (24.56%) subjects had lower first molar which is one cusp or more mesial or distal to its normal relation.
| Age Group | No abnormality / Minor malocclusion | Definite malocclusion | Severe Malocclusion | Very severe Malocclusion | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 12-17yrs (n= 111) | 51 (45.94) | χ2= 0.257 df =1 P =0.612 NS |
21 (18.91) | χ2 = 0.029 df =1 P =0.864 NS |
18 (16.21) | χ2 = 1.247 df =1 P =0.264 NS |
21 (18.91) | χ2= 0.029 df =1 P =0.864 NS |
|||
| 18-30yrs (n=60) | 30 (50.00) | 12 (20.00) | 6 (10.00) | 12 (20.00) | |||||||
| Gender | |||||||||||
| Male (M=129) | 64 (49.61) | χ2 = 1.491 df =1 P =0.222 NS |
24 (18.60 | χ2 = 0. 032 df =1 P =0.858 NS |
16 (12.40) | χ2 = 0. 736 df =1 P =0.391 NS |
25 (19.37) | χ2 = 0. 060 df =1 P =0.807 NS |
|||
| Female (F=42) | 17 (40.47) | 9 (21.42) | 8 (19.04) | 8 (19.04) | |||||||
| Total (n= 171) | 81 (47.36) | 33 (19.29) | 24 (14.03) | 33 (19.29) | |||||||
Table 4: Number and percentage of subjects with maxillary and mandibular overjet, open bite and antero-posterior molar relationship.
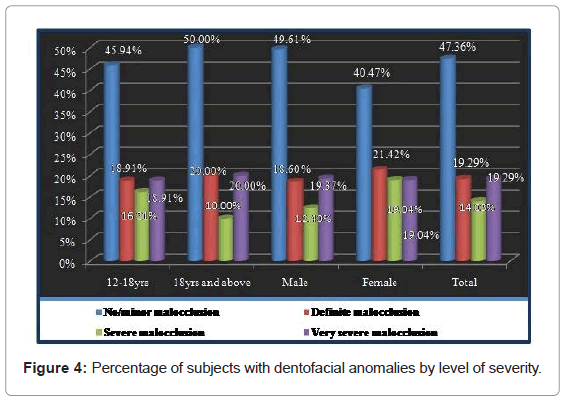
Table 5 and Figure 4: Percentage of subjects with dentofacial anomalies by level of severity.
As shown in Table 4 and Figure 3, 81 (47.36%) subjects had no or minor malocclusion. Definite malocclusion was seen in 33 (19.29%), severe malocclusion in 24 (14.03%) study subjects and 33 (19.29%) subjects had very severe malocclusion. No statistically significant difference was seen in the prevalence of malocclusion as per age or gender (P>0.05).
| Age Group | Maxillary overjet n (%) | Mandibular overjet n (%) | Openbite n (%) | Ant-post molar relation | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal n (%) | Half cusp n (%) | Full cusp n (%) | ||||||||||||||
| 12-17yrs (n= 111) | 87 (78.37 | χ2= 0.062 df = 1 P = 0.804 NS |
10 (9.00) | χ2 = 0.891 df = 1 P = 0.345 NS |
10 (9.00) | χ2 = 0.284 df = 1 P =0.594 NS |
51 (45.94) | χ2 = 1.791 df =1 P =0.181 NS |
34 (30.06) | χ2= 3.974 df =1 P =0.046 S |
26 (23.42) | χ2= 0. 221 df =1 P =0.638 NS |
||||
| 18-30yrs (n=60) | 48 (80) | 3 (5.00) | 4 (6.66) | 34 (56.66) | 10 (16.66) | 16 (26.66) | ||||||||||
| Male (M=129) | 99 (76.74) | χ2 = 1.871 df = 1 P = 0.71 NS |
12 (9.30) | χ2 = 0.00 df = 1 P = 0. 985 NS |
9 (6.97) | χ2= 1.109 df = 1 P = 0.292 NS |
61 (47.28) | χ2= 0.321 df =1 P =0.571 NS |
33 (25.58) | χ2 = 0.027 df =1 P =0.870 NS |
35 (27.13) | χ2= 2.238 df =1 P =0.135 NS |
||||
| Female (F=42) | 36 (85.71) | 1 (2.38) | 5 (1.190) | 24 (57.14) | 11 (26.19) | 7 (16.66) | ||||||||||
| Total (n= 171) | 135 (78.94) | 13 (7.60) | 14 (8.18) | 85 (49.70) | 44 (25.73) | 42 (24.56) | ||||||||||
Table 5: Number and percentage of subjects with dentofacial anomalies by level of severity.
Discussion
Mentally challenged individuals have an intellectual ability significantly lower than average and limited ability to adapt to the environment. They have impaired physical coordination and cognitive sequencing skill that limit independence in task completion and may result in an inability to maintain proper oral hygiene. These individuals are particularly vulnerable to having unmet health care needs as they are faced with many challenges in understanding and maintaining their health. Maintenance of oral health in these subjects is further complicated by systematic problems [22] , unwillingness by dentist to treat these subjects [23], operating loss of dentist in treating these subject96, higher costs of treatment [24] , severe behavioural problems, assistance or support needed from caretakers to maintain their oral health, adverse habits like lip biting , tongue thrusting etc.
Extensive exploration of available literature revealed very scarce data related to Dentofacial anomolies of mentally challenged study subjects in India. Many of the studies on mentally challenged have been done in combination with other handicapping conditions and results have been discussed collectively.
There were total 277 study subjects with age range of 4yrs to 30 years which were divided as below 6 years, 6-12yrs, 12-18 years and 18years and above. Out of 277 study subjects, 74.00% were males and 26.00% were females. Percentage of males was higher than females in all the three age groups (Table 1 and Figure1,2).
TMJ clicking was seen in 11.02% study subjects. It was highest in the age group 18 years and above (21.66%) and more in males than females (Table 2 and Figure 3). This finding was in contradiction to the study conducted by Asokan et al. [18] in which none of the study subject had clicking.
TMJ problems recorded in the these subjects may be due the presence of malocclusion, occlusal discrepancy, parafunctional habits like bruxism, masticatory dysfunction, hypotonia and hyperextensibility of joints, uncoordinated and uncontrolled movements of jaw etc. Similar justifications were given by Bhowate R and Dubey [19] and Desai et al. [20]. TMJ clicking in the present study was found to increase with increase in age (P<0.05). This may be because age acts as a risk factor for TMJ disorders (although not very serious) and TMJ disorders tend to affect people between the ages of 20 and 50 years [25].
Dentofacial anomalies were measured for the study subjects from the age of 12 years and above. 4.09% and 2.92% of the study subjects had missing teeth in maxillary and mandibular arch respectively. Oredugba [16], Rao et al. [26] reported slightly higher prevalence of missing anterior teeth compared to present study. Crowding and spacing of anterior teeth was seen in 47.95% and 33.91% of the subjects respectively. 16.37% of the study subjects had midline diastema. Anterior maxillary and mandibular irregularity was present respectively in 40.93% and 39.76% of the subjects respectively (Table 3). Kawaguchi and Nakashima [10] reported similar prevalence of crowding as seen in the present study. Rao et al. [26], Oredugba and Akindayomi [9], Mestrovic et al. [17] recorded lower prevalence of crowding. Slightly higher prevalence of crowding compared to present study was reported by Oredugba [16].
Higher prevalence of spacing, midline diastema and lower prevalence of anterior maxillary irregularity and anterior mandibular irregularity compared to the present study was reported by Rao et al. [26]. Maxillary overjet was present in 78.94% of the study subjects, mandibular overjet in 7.60% and openbite in 8.18% of the study subjects (Table 4). Similar prevalence of openbite was reported by Oredugba and Akindayomi [9]. Asokan et al. [18] reported slightly higher prevalence of open bite and cross bite. Adenubi et al. [13] reported 15% of subjects with malocclusion of which 40% had anterior openbite, and 10% had anterior crossbite. Vigilid [14] reported similar prevalence of mandibular overjet in mentally retarded and higher prevalence of anterior open bite compared to the present study. Normal anterioposterior molar relation was seen in majority of the study subjects (49.70%) followed by subjects with half cusp (25.73%) or full cusp (24.56%) discrepancy (Table 4).
Similar findings about molar relation were recorded by Rao et al. [26] and Vigilid [14] reported similar prevalence of mandibular over jet in mentally retarded and higher prevalence of anterior open bite compared to the present study.
Normal anterioposterior molar relation was seen in majority of the study subjects (49.70%) followed by subjects with half cusp (25.73%) or full cusp (24.56%) discrepancy (Table 4). Similar findings about molar relation were recorded by Rao et al. [26] and Vigilid [14]. Oredugba and Akindayomi [9] reported highest prevalence of Angle’s class I malocclusion followed by Angle’s class II and Angle’s class III. Svatun and Heloe [15] reported Angles class III malocclusion in 16% of the mentally challenged. Oredugba [16] reported 51% of the study subjects with Down syndrome to have Class I malocclusion which can be correlated with normal molar relation in our study and 47% had class III malocclusion. Ajami et al. [27] reported majority of mentally challenged study subjects with Angle’s Class I malocclusion.
Mestrovic et al. [17] reported class III malocclusion in 43.8% of the study subjects. Variation in findings in different studies may be attributed to difference in indices used to record malocclusion, variation in severity of mental subnormality, types of mental subnormality included in different studies etc.
There was no significant association between percentage of subject with various dentofacial anomalies among age groups except for diastema and open bite (P<0.05). No statistically significant gender difference was observed for various dentofacial anomalies. The percentage of subjects with no or minor malocclusion was 47.36%. Definite, severe and very severe malocclusion was seen in 19.29%, 14.03% and 19.29% subjects respectively (Table 5 and Figure 4). This finding was in accordance with that reported by Rao et al. [26]. Onyeaso [28] has reported similar prevalence of no minor malocclusion and severe malocclusion but higher prevalence of very severe malocclusion compared to the present study.
Higher prevalence of malocclusion in the present study can be attributed to various etiological factors like deficient maxillary growth, abnormal tongue size and various harmful habits [22]. Disharmonious relationship between intraoral and perioral movements, uncoordinated and uncontrolled movements of jaws, lips and tongue, retardation of growth of jaws and their placement anterior to the cranial base may be some of the factors responsible for higher prevalence of malocclusion seen in the present study. Functional anomalies of the tongue and perioral muscles, particular pattern of oral habits, incompetent lip among the mentally retarded may also play a vital role. Mentally subnormal child is sensitive and more vulnerable to stress because it has inadequate concept of its environment. This may result in emotional insecurity and forces the child to diversify into deleterious oral habits like thumb sucking, tongue thrusting etc. These habits bring about harmful unbalanced pressures to bear upon the immature, highly malleable alveolar processes and the potential changes in position of teeth in occlusion [29]. Similar interpretations were given by Nunn [30], Vigilid [14], Bhowate and Dubey [19], Winter et al. [31].
Higher prevalence of malocclusion as compared to the present study was reported by Desai et al. [20] and Vittek et al. [32], Mestrovic et al. [17]. Desai et al. [20] correlated the severity of malocclusion with level of dependency among study subjects. Studies conducted by Scott et al. [33], Adenubi et al. [13], Bhowate and Dubey [19], Asokan et al. [12] reported lower prevalence of malocclusion as compared to the present study. The variation in malocclusion may be due to diverse methodologies employed in assessment of malocclusion, dissimilar percentage of various types and degrees of mental subnormality, geographic and genetic disparities among study subjects etc. Similar observations were made by Onyeaso [28], Vittek et al. [32]. Although there is considerable information available about the occlusal pattern of normal children, there is a paucity of comparable information about mentally challenged there by making comparison of findings difficult. There was no statistically significant difference in level of severity between males and females (P>0.05) which was in agreement to that seen by Vigilid [14]. A contradictory finding was reported by Onyeaso [28] wherein a significant gender difference in the dental aesthetic index (DAI) scores was observed. No statistically significant difference in the severity of malocclusion as recorded by DAI was observed in age groups (P>0.05). The findings of the study indicate that there is a high prevalence of Dentofacial anomalies in mentally challenged study subjects in Vadodara District.
Conclusion
1. Clicking was the only positive finding observed for TMJ and it was seen in 11.02% of the study subjects. Tenderness and reduced jaw mobility was not seen among any of the study subjects.
2. Crowding and spacing of anterior teeth was seen in 47.95% and 33.91% of the study subjects respectively. Anterior open bite was seen in 8.18% of the study subjects
3. Molar discrepancy of half a cusp mesial or distal to normal was seen in 25.73% of the study subjects and 24.56% of the study subjects had molar discrepancy of one cusp or more mesial or distal to that of normal.
4. Definite malocclusion was seen in 19.29%, severe malocclusion in 24 (14.03%) study subjects and 33 (19.29%) subjects had very severe malocclusion.
Thus it is concluded from the observations of the present study that the Dentofacial change and TMJ Status of mentally challenged study subjects attending special schools in Vadodara District is poor and there is a significant unmet need for dental preventive and treatment services.
References
- McDonalds R, Avery DR, Dean JA (2004) Dentistry for child and adolescents. (8th Edn) Mosby publishers, St. Louis (Missouri), p. 524-56.
- Introduction to Mental Retardation.
- Mental retardation: Medline Plus Medical Encyclopedia.
- PahlaKadam (Rajasthan MahilaKalyanMandal) Ajmer District, Rajasthan.
- National Sample Survey Organization (2003) Disabled persons in India. NSS report no. 485 (58/26/1), New Delhi.
- Disorder Information Sheet.
- Welbury R, Duggal M, Hosey MT (2005) Pediatric Dentistry. (3rd Edn) Oxford University press : p. 414-430.
- Agarwal AK, Sharma VP (2002) Rehabilitation Management of Mentally Retarded Amongst Physically Disabled. IJPMR 13: 35-38.
- Oredugba FA, Akindayomi Y (2008) Oral health status and treatment needs of children and young adults attending a day centre for individuals with special health care needs. BMC Oral Health 8: 30.
- Kawaguchi T, Nakashima M (1990) Oral findings of institutionalized handicapped children. Fukuoka ShikaDaigakuGakkaiZasshi 17: 13-21.
- Dinesh RB, Arnitha HM, Munshi AK (2003) Malocclusion and orthodontic treatment need of handicapped individuals in South Canara, India. Int Dent J 53: 13-18.
- Asokan S, Muthu MS, Sivakumar N (2008) Oral findings of Down syndrome children in Chennai city, India. Indian J Dent Res 19: 230-235.
- Adenubi JO, Saleem FH, Martirez JN (1997) Dental health care at The Disabled Children's Rehabilitation Center in Riyadh. The Saudi Dent J 9 : 9-13.
- Vigild M (1985) Prevalence of malocclusion in mentally retarded young adults. Community Dent Oral Epidemiol 13: 183-184.
- Svatun B, Helöe LA (1975) Dental status and treatment needs among institutionalized mentally subnormal persons in Norway. Community Dent Oral Epidemiol 3: 208-213.
- Oredugba FA (2007) Oral health condition and treatment needs of a group of Nigerian individuals with Down syndrome. Downs Syndr Res Pract 12: 72-76.
- Mestrovic S, MiksicM, Stefanac-Papic J, Stipetic J (2002) Prevalence of Malocclusion in Patients with Downs Syndrome. ActaStomatol Croat 36: 239-241.
- Asokan S, Muthu MS, Sivakumar N (2008) Oral findings of Down syndrome children in Chennai city, India. Indian J Dent Res 19: 230-235.
- Bhowate R, Dubey A (2005) Dentofacial changes and oral health status in mentally challenged children. J Indian SocPedodPrev Dent 23: 71-73.
- Desai M, Messer LB, Calache H (2001) A study of the dental treatment needs of children with disabilities in Melbourne, Australia. Aust Dent J 46: 41-50.
- Joharji RM, Adenubi JO (2001) Prevention of pit and fissure caries using an antimicrobial varnish: 9 month clinical evaluation. J Dent 29: 247-254.
- Pilcher ES (1998) Dental Care for the Patient with Down Syndrome. Down Synd Res and Pract 5: 111-116.
- Balogh RS, Ouellette-Kuntz H, Hunter DJ (2004) Regional variation in dental procedures among people with an intellectual disability, Ontario, 1995-2001. J Can Dent Assoc 70: 681, 681a-681f.
- Waldman HB, Perlman SP, Swerdloff M (2001) Children with mental retardation/developmental disabilities: do physicians ever consider needed dental care? Ment Retard 39: 53-56.
- Lim C. T m j Solution - Tmj Disorders.
- Dinesh RB, Arnitha HM, Munshi AK (2003) Malocclusion and orthodontic treatment need of handicapped individuals in South Canara, India. Int Dent J 53: 13-18.
- Ajami BA, Shabzendedar M, Rezay YA, Asgary M (2007) Dental treatment needs of children with disabilities. J Dent Res Dent Clin Dent Prospects 1: 93-98.
- Onyeaso CO (2003) Orthodontic treatment need of mentally handicapped children in Ibadan, Nigeria, according to the dental aesthetic index. J Dent Child (Chic) 70: 159-163.
- Dinesh RB, Arnitha HM, Munshi AK (2003) Malocclusion and orthodontic treatment need of handicapped individuals in South Canara, India. Int Dent J 53: 13-18.
- Dinesh RB, Arnitha HM, Munshi AK (2003) Malocclusion and orthodontic treatment need of handicapped individuals in South Canara, India. Int Dent J 53: 13-18.
- Winter K, Baccaglini L, Tomar S (2008) A review of malocclusion among individuals with mental and physical disabilities. Spec Care Dentist 28: 19-26.
- Vittek J, Winik S, Winik A, Sioris C, Tarangelo AM, et al. (1994) Analysis of orthodontic anomalies in mentally retarded developmentally disabled (MRDD) persons. Spec Care Dentist 14: 198-202.
- Scott A, March L, Stokes ML (1998) A survey of oral health in a population of adults with developmental disabilities: comparison with a national oral health survey of the general population. Aust Dent J 43: 257-261.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 14817
- [From(publication date):
December-2014 - Jul 04, 2025] - Breakdown by view type
- HTML page views : 10125
- PDF downloads : 4692