Case Report Open Access
Evaluation of Dentoalveolar Compensation in the Treatment of Class III Malocclusion
Guilherme Janson1*, José Eduardo Prado de Souza1, Roberto Bombonatti1, Mariana Pracucio Gigliotti1 and Pedro Andrade Júnior21Department of Orthodontics. Bauru Dental School, University of São Paulo, Brazil
2Private practice, São Paulo, Brazil
- Corresponding Author:
- ADr. Guilherme Janson, D.D.S., M.Sc., Ph.D., M.R.C.D.C
(Member of the Royal College of Dentists of Canada) Professor
Department of Orthodontics. Bauru Dental School
University of São Paulo-17012-901, Brazil
Tel: 55 14 32344480
E-mail: jansong@travelnet.com.br
Received date September 11, 2014; Accepted date October 15, 2014; Published date October 20, 2014
Citation: Janson G, Souza JEPD, Bombonatti R, Gigliotti MP, J├?┬║nior PA (2014) Evaluation of Dentoalveolar Compensation in the Treatment of Class III Malocclusion. J Interdiscipl Med Dent Sci 2:156. doi: 10.4172/2376-032X.1000156
Copyright: © 2014 Janson G, et al.. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Background: In Class III patients with mild jaw discrepancies and no cosmetic problems, compensatory orthodontic treatment is an alternative for them. The purpose of this retrospective study was to evaluate the cephalometric and occlusal changes of dentoalveolar compensation in the treatment of Class III malocclusions.
Methods: The sample consisted of 23 adult patients (mean age, 25.18 years) from whom lateral headfilms and dental casts were obtained and evaluated at the pretreatment and posttreatment stages. The cephalometric treatment changes were evaluated with paired t tests performed between the two stages, as well as the pretreatment and posttreatment occlusal statuses, assessed with Grainger’s treatment priority index (TPI), in order to evaluate the amount of occlusal changes.
Results: Cephalometric results showed statistically significant dentoalveolar changes primarily in the mandibular component. There were significant increases in overbite and overjet and decreases in apical base discrepancy and facial concavity. Occlusal results showed statistically significant reductions in TPI score, achieving an improvement ratio of 82.17% with the treatment protocol.
Conclusions: Compensatory treatment of adult patients with Class III malocclusion produce favorable and significant amount of dentoalveolar, skeletal and occlusal changes.
Keywords
Corrective orthodontics; Angle Class III malocclusion; Dentoalveolar compensation.
Introduction
Class III malocclusions are considered one of the most complex and difficult orthodontic problems to diagnose and treat, thus early intervention of skeletal Class III deformities in the mixed dentition or even in the deciduous dentition has been the best alternative to treat this malocclusion [1,2]. However, adult patients who present with a Class III deformity generally do not have many treatment options and their prognosis is not favorable [1,2]. They are usually potential candidates for orthognathic surgery to correct the skeletal anomaly. Nevertheless, an alternative for patients reluctant to undergo surgery or who are satisfied with their facial appearance is to treat with dentoalveolar compensation without correcting the underlying skeletal deformity [3-6].
The option for orthognathic surgical treatment clearly produces, in most cases, better esthetic results than compensatory treatment, but it is sometimes perceived as too aggressive and costly [7]. The dilemma we usually face is that a great number of these patients refuse to accept surgical therapy and prefer an orthodontic compensation treatment [8,9]. In patients with mild jaw discrepancies and no cosmetic problems, orthodontic treatment without surgery is often preferable since several non-surgical Class III adult case reports [4-6,8,10] have demonstrated very satisfactory results with conservative mechanics in these cases.
Therefore, the objectives of this study was to cephalometrically evaluate the effects of dentoalveolar compensation in the treatment of adults with skeletal Class III malocclusion and to evaluate the occlusal results and changes obtained with compensatory dentoalveolar mechanics in these patients.
Materials and Methods
The sample consisted of 23 adult subjects (10 male, 13 female, mean age [SD] 25.18 [6.69] years, range 18.00-39.92), with Class III malocclusion, selected from the private office file of Dr.______________. The selection criteria were a dental and skeletal Class III malocclusion (ANB, NAP and Wits) with at least an endto- end bilateral Class III molar relationship, anterior and posterior crossbites, and a concave facial profile. Fourteen patients were treated with two mandibular premolar and 6 with two mandibular first molar extractions. Only three patients were treated without extractions. The mean treatment time was 3.10 years (SD=0.90). Lateral cephalometric radiographs and dental casts were obtained from each subject before treatment (T1) and immediately after treatment (T2).
Cephalometric analysis
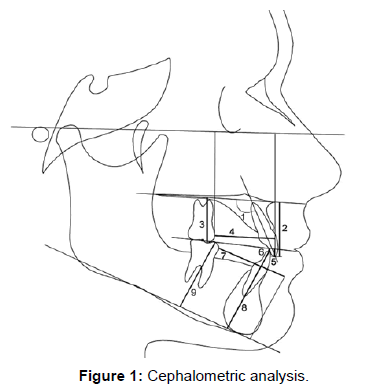
All lateral cephalograms were traced by one investigator (JEPS), digitized (Numonics AccuGrid XNT, model A30TL.F—Numonics Corporation, Montgomeryville, Pa) (Table 1 and Figure 1) and then analyzed with Dentofacial Planner Software 7.02 (Toronto, Ontario, Canada).
Occlusal evaluation
| IS.PP (o) | Maxillary incisor long axis to palatal plane |
| IS-PP (mm) | Perpendicular distance from the maxillary incisor edge to palatal plane |
| Mx6-PP (mm) | Perpendicular distance from the mesial cusp tip of the maxillary molar to palatal plane |
| Mx6-ANSPerp (mm) | Distance between the mesial point of the maxillary first molar and the anterior nasal spine-perpendicular line |
| Mx1-OP (mm) | Perpendicular distance from the maxillary central incisor edge to the occlusal plane |
| Md1-OP (mm) | Perpendicular distance from mandibular central incisor edge to the occlusal plane |
| Md6-PogPerp (mm) | Distance between the mandibular first molar mesial point and the pogonion-perpendicular line (measured only in cases in which these teeth were not extracted) |
| Md1-MP (mm) | Perpendicular distance from mandibular central incisor edge to the mandibular plane |
| Md6-MP (mm) | Perpendicular distance from the mesial cusp tip of the mandibular molar to mandibular plane (measured only in cases in which these teeth were not extracted) |
| NAP (°) | Angle between lines N-A and A-P |
Table 1: Unusual cephalometric variables.
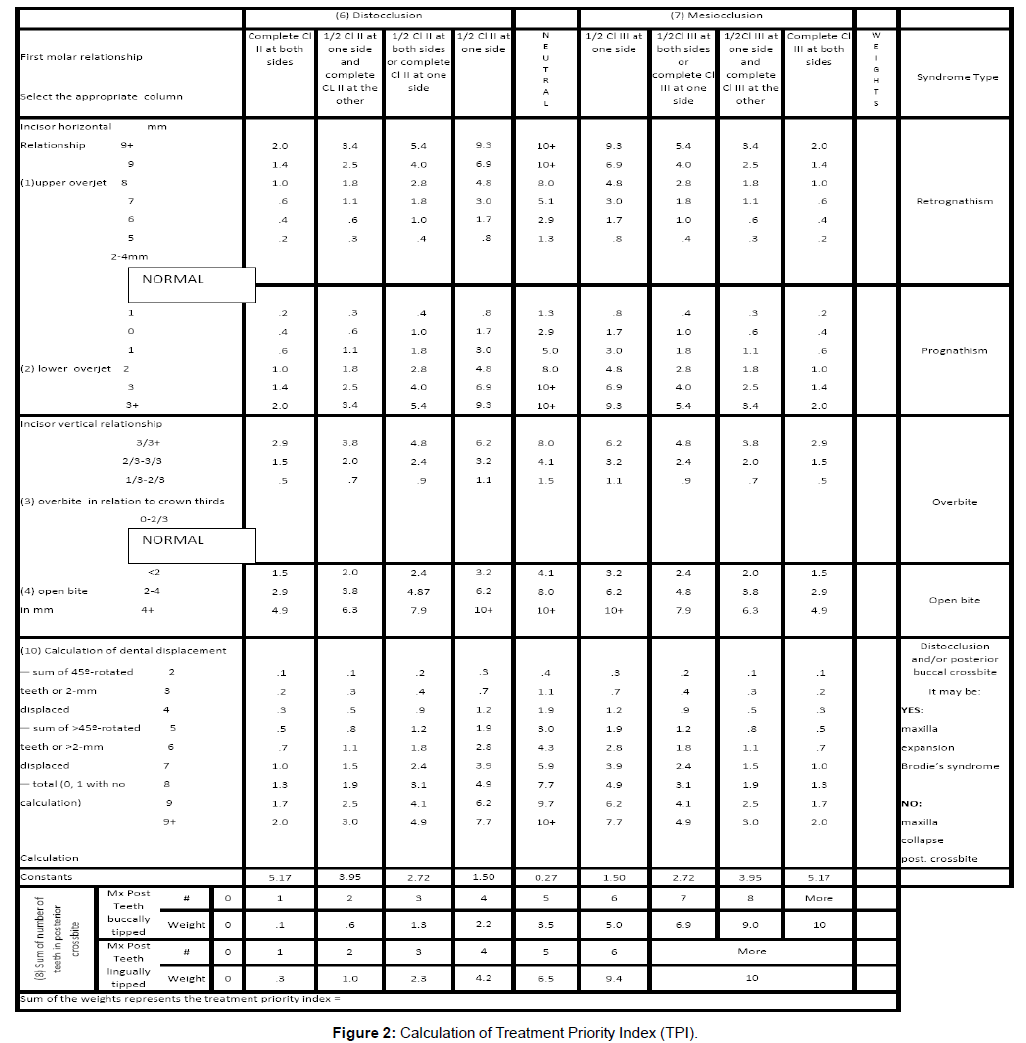
The Treatment Priority Index (TPI) [11] was calculated on the pre and posttreatment dental study models (Figure 2). Set patterns or combinations of the selected items defined syndromes. A total of seven syndromes evolved defining the incisor relationship horizontally (underjet, overjet) and vertically (overbite, open bite), the occlusion of the buccal segments (posterior crossbite), and tooth displacement (rotation and crowding) (Figure 2). On the basis of multiple regression analysis, the syndromes were weighted according to the permanent first molar relationship, mesio, neutro, and distoclusion. A constant, also corresponding to the molar occlusion, was added to the TPI score. The final result constitutes the TPI value [12], which represents the severity of malocclusion and could range from 0 to > 10.
The degree of improvement as a result of orthodontic treatment was assessed by two methods. The first method used the TPI change, which is the difference between the pretreatment and posttreatment scores. The second was the percent TPI reduction, which reflects the TPI change relative to the pretreatment score and is calculated by dividing the difference between initial (ITPI) and final (FTPI) TPI by the initial TPI score.
Error study
Cephalograms and dental casts of 10 randomly selected patients were retraced, redigitized, and remeasured by the same examiner. The casual errors were calculated according to Dahlberg’s formula [13], Se2=Σd2/2n. The systematic errors [14] were calculated with dependent t tests, for P<0.05.
Statistical analyses
Means and standard deviations for each variable were calculated to enable characterization of the groups. All variables were normally distributed (Kolmogorov-Smirnov test) for the initial and final values, and for the treatment changes. Therefore, the Class III intra-group cephalometric and occlusal changes were evaluated with paired t tests (P<0.05). The statistical analyses were performed with Statistica for Windows 6.0 (Statsoft, Tulsa, Okla).
Results
Only three cephalometric variables showed significant systematic errors (Mx6-PP, Mx6-ENAperp, Md6-GoMe), and the range of casual errors varied from 0.16 (overbite) to 3.30 (SNB). There was no systematic error for the TPI evaluation and the casual error was of 0.217.
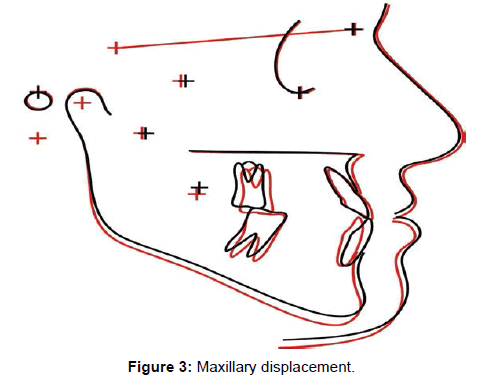
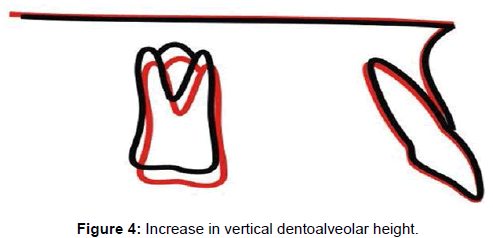
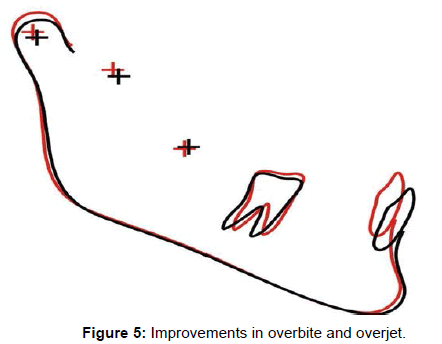
There was significant maxillary advancement, mandibular retrusion, improvement in apical base relationship and an increase in facial convexity and in lower anterior face height. The maxillary incisors had significant labial tipping and the molars had a significant vertical dentoalveolar height increase (Table 2 and Figures 3,4). The mandibular incisors experienced significant lingual tipping, retrusion and increase in dentoalveolar height, and the molars had an increase in dentoalveolar height. The overbite and overjet showed statistically significant improvements (Table 2 and Figures 3,5).
There was significant reduction in TPI and the mean TPI change was 9.85, with a percent TPI reduction of 82.17% (Table 3).
Discussion
Sample
The investigated patients had a moderate skeletal Class III malocclusion, as evaluated by means of ANB and more severe according to Wits, NAP and MxMdDif variables (Table 2). To compensate for the apical bases discrepancy the maxillary incisors were labially tipped and the mandibular incisors were lingualy tipped, as usually expected [4-6,9,15,16]. The Class III occlusal relationship was also very severe with an initial TPI of 11.77 (Table 3), showing that the evaluated cases were more severe than previous reports and studies [4,10].
Study design
Ideally, all patients should have been treated following a unique treatment protocol at a similar age range. However, if these strict criteria were applied a very limited number of patients would result to allow statistical evaluation. Some changes have been reported, but mostly in individual case reports [4-6,10,17]. Therefore, the Class III malocclusion occlusal changes were evaluated in order to allow an estimate of the most relevant changes obtainable with compensatory orthodontic approaches of the Class III malocclusion problem.
There may be some criticism in using Grainger´s treatment priority index [11] (TPI) for evaluation of the pretreatment and posttreatment occlusal statuses instead of using the more recent and currently mostly used PAR index [18,19]. The reason for this is because the PAR index presents some limitation in evaluating the posterior segment anteroposterior relationship [20]. To overcome this deficiency it has been suggested that there should be a different PAR index to separately evaluate Class I, II and III malocclusions [21].
Skeletal changes
Maxillary component: There were significant forward maxillary displacement, associated with an increase in the effective maxillary length, even in adult patients, which were more favorable than previous studies [4,15] (Table 2 and Figure 3). This probably resulted from the intensive use of Class III intermaxillary elastic mechanics [3-5,22]. Regarding Class III malocclusion treatment, small changes may represent finishing with an end-to-end incisor relationship or with a minimum overbite which will allow anterior guidance upon protrusion [23].
Mandibular component: There was a significant reduction in mandibular prognathism (SNB), despite significant increases in mandibular dimensions (Table 2 and Figures 3,5). This reduction occurs with most Class III treatment mechanics as they tend to increase the LAFH and the mandible experiences clockwise rotation [3-6,9,10,17]. An important factor that may have greatly accounted for the significant reduction in SNB was retrusion of B point resultant from retraction of the mandibular incisors in extraction cases (Figures 3,5). This seems to be the case because P-Nperp did not show a significant reduction. As the amounts of changes in opposite directions are added up they significantly contribute for the overall occlusal and esthetic improvements of the malocclusion [3,9].
Maxillomandibular relationship: Consequent to the small but significant maxillary forward displacement and mandibular retrusion, there were significant improvements in apical base relationships (ANB, Wits and NAP). The numerically greater improvement (Wits) was probably due to retraction of the mandibular anterior teeth in the extraction cases, which would also cause some retraction of B Point [3,6].
Vertical component: Although the Class III mechanics used tend to increase the growth pattern angles no significant increase was observed. Very likely this was a result of the extractions performed in most patients, especially when the mandibular first molars were extracted [17]. Only LAFH had a significant increase with treatment. Therefore, the mandibular extractions were efficient in controlling the growth pattern angles increase in patients with an associated open bite.
Maxillary dentoalveolar component: The applied mechanics caused significant labial tipping of the maxillary incisors which contributed to correction of the negative overjet of the malocclusion (Table 2). This effect is expected with the use of Class III elastics [3-5,9,17], however, the amount of incisor protrusion was not significant, especially demonstrating a net tipping effect. Despite the lingual torque (0º) of the bracket system used, there was still some labial tipping of these teeth. Perhaps, if other system was used, the labial tipping could have been ever greater [3]. There was extrusion of the maxillary molars which is also a usual response to Class III elastics and that may have contributed to increase the LAFH, associated with growth in some cases [22,24]. Although the maxillary molars experienced slight mesial displacement, it was not statistically significant. Therefore, there was only a small contribution of maxillary dentoalveolar changes to correct the anteroposterior Class III discrepancy.
Mandibular dentoalveolar component and dental relationships: There was significant lingual tipping, retrusion and extrusion of the mandibular incisors, which is expected with the use of Class III elastics [22,25] (Table 2). The compensatory labial torque (10º) to the mandibular incisors, provided in the bracket slots, was not enough to completely counteract the Class III elastic force. The significant increase in mandibular first molar dentoalveolar height was probably due to growth changes in those patients in the final stages of development. Dentoalveolar changes in mandibular component constituted the main mechanism of compensatory treatment in adult patients to correct the anteroposterior discrepancy in Class III malocclusions, as also previously reported [3,4,9]. All the mentioned changes provided significant improvement in the overjet and overbite.
Amount of occlusal changes
The Class III malocclusion patients had great initial occlusal malocclusion severity, associated in many cases with skeletal deficiencies (Table 3). The final TPI and the percent TPI reduction were very satisfactory. This fact demonstrated good patient compliance, regarding the use of Class III intermaxillary elastics [22,24].
To provide an estimate of the amount of occlusal changes of this treatment approach, the results observed in this study could be compared with the occlusal changes in Class II malocclusion [26]. Nonextraction and two-maxillary premolar extraction treatment protocols of complete Class II malocclusion provided percent TPI reductions of 79.78% and 91.32% and final TPIs of 1.58 and 0.68, respectively [26]. The present study obtained a percent reduction of 82.17% and a final TPI of 1.98 (Table 3). The similarities in the final occlusal status and percent TPI reduction with the non-extraction Class II malocclusion treatment demonstrate that the amount of changes obtained with the compensatory approach was very satisfactory. It did not reach final TPI and improvement ratio as the Class II malocclusion group treated with two-maxillary premolar extractions because the patient dependent anchorage requirement in this treatment protocol is smaller when compared to the Class II non-extraction protocol [26,27]. Most of the Class III treatment protocols used in these cases also require a similar patient compliance as in Class II non-extraction protocol, regarding the use of Class III intermaxillary elastics.
Clinical considerations
These results can provide to the orthodontist an estimate of the cephalometric and occlusal changes obtainable with Class III compensatory treatment, primarily with extraction in the mandibular arch. The results presented supply scientific basis to the orthodontist decision during treatment planning of patients with Class III malocclusions, demonstrating which are the areas where to expect greater changes and what percentage of occlusal changes can be obtained.
| Variables | Initial (n = 23) | Final (n = 23) | P | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Difference | |||
| Maxillary Component | |||||||
| SNA (o) | 81.30 | 3.19 | 82.17 | 4.53 | 0.87 | 0.08 | |
| A-NPerp (mm) | -2.15 | 3.54 | -1.05 | 3.62 | 1.10 | 0.01* | |
| Co-A (mm) | 81.39 | 6.17 | 83.00 | 6.13 | 1.61 | 0.00* | |
| Mandibular Component | |||||||
| SNB (o) | 84.21 | 4.55 | 83.05 | 5.29 | -1.16 | 0.02* | |
| P-Nperp | 2.98 | 7.55 | 2.23 | 8.43 | -0.65 | 0.32 | |
| Co-Go (mm) | 55.93 | 3.98 | 58.03 | 4.14 | 2.01 | 0.00* | |
| Co-Gn (mm) | 120.70 | 7.63 | 122.34 | 7.90 | 2.67 | 0.01* | |
| Co.GoMe (o) | 128.60 | 6.28 | 128.73 | 6.38 | 0.13 | 0.77 | |
| Maxillomandibular relationship | |||||||
| ANB (o) | -2.91 | 2.99 | -0.88 | 2.18 | 1.93 | 0.00* | |
| MxMdDif (mm) | 39.31 | 5.36 | 39.33 | 5.32 | -0.03 | 0.95 | |
| WITS (mm) | -9.40 | 4.63 | -5.22 | 3.63 | 4.18 | 0.00* | |
| NAP (o) | -7.68 | 6.11 | -4.38 | 4.53 | 3.30 | 0.00* | |
| Vertical Component | |||||||
| FMA (o) | 29.93 | 6.23 | 30.50 | 6.77 | 0.57 | 0.13 | |
| SN.PP (mm) | 8.17 | 4.12 | 8.35 | 4.68 | 0.18 | 0.66 | |
| SN-OP (o) | 43.00 | 4.90 | 43.43 | 5.17 | 0.43 | 0.28 | |
| LAFH (mm) | 67.82 | 7.58 | 70.67 | 7.28 | 2.85 | 0.00* | |
| SN.GoGn (o) | 33.66 | 6.81 | 34.34 | 7.68 | 0.68 | 0.10 | |
| Maxillary dentoalveolar Component | |||||||
| Mx1.NA (o) | 29.08 | 7.99 | 31.94 | 5.84 | 2.86 | 0.02* | |
| Mx1-NA (mm) | 6.61 | 3.59 | 7.08 | 2.83 | 0.47 | 0.31 | |
| IS.PP (o) | 119.09 | 7.03 | 122.69 | 7.00 | 3.60 | 0.01* | |
| IS-PP (mm) | 27.00 | 3.67 | 26.94 | 4.02 | -0.06 | 0.89 | |
| Mx6-PP (mm) | 23.33 | 2.75 | 24.97 | 2.33 | 1.64 | 0.00* | |
| Mx6-ANSPerp (mm) | 25.03 | 4.51 | 23.86 | 4.92 | -1.17 | 0.08 | |
| Mx1-OP (mm) | -0.15 | 1.79 | -0.75 | 2.28 | -0.60 | 0.33 | |
| Mandibular dentoalveolar Component | |||||||
| Md1.NB (o) | 20.24 | 6.51 | 14.75 | 6.26 | -5.49 | 0.00* | |
| Md1-NB (mm) | 3.97 | 2.52 | 2.22 | 2.24 | -1.75 | 0.00* | |
| Md1-MP (mm) | 39.94 | 4.54 | 42.18 | 4.10 | 2.24 | 0.00* | |
| Md6-MP (mm) | 29.63 | 4.46 | 31.00 | 4.64 | 1.37 | 0.00* | |
| Md1.MP (o) | 79.54 | 7.69 | 74.28 | 9.97 | -5.26 | 0.00* | |
| Md6-PogPerp (mm) | -31.05 | 4.84 | -29.97 | 4.47 | 1.08 | 0.14 | |
| Md1-OP (mm) | -1.08 | 2.81 | -2.33 | 1.82 | -1.25 | 0.05 | |
| Dental relationships | |||||||
| Overjet (mm) | -1.26 | 1.99 | 3.66 | 1.22 | 4.92 | 0.00* | |
| Overbite (mm) | 0.73 | 2.30 | 2.00 | 1.05 | 1.27 | 0.00* | |
Perp, Perpendicular; Mx1, maxillary central incisor; Mx6, maxillary first molar; Md1, mandibular central incisor; Md6, mandibular first molar *Statistically significant at P <0.05
Table 2: Comparison of changes from T1 to T2 (paired t test)
| ITPI | FTPI | Paired t test | TPI change | Percent TPI reduction |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | P | Mean (SD) | Mean (SD) |
| 11.77 (3.68) | 1.91 (0.73) | 0.0000* | 9.85 (3.79) | 82.17% (9.79) |
*Statistically significant at P<0.05
Table 3: Occlusal treatment changes, TPI change and percent TPI reduction with treatment
Conclusions
1. Compensatory mandibular extraction or non-extraction treatment of Class III malocclusions can establish normal overjet and overbite through significant changes in the maxillomandibular relationship, associated with labial tipping of the maxillary incisors and lingual tipping of the mandibular incisors. These changes also bring about increases in facial convexity and in facial height.
2. The final occlusal status and improvement ratio of Class III malocclusion patients treated with compensatory treatment were very satisfactory.
3. These treatment protocols can be used in patients with similar occlusal and skeletal discrepancies to the sample of this study, when surgical treatment is discarded.
References
- Campbell PM (1983) The dilemma of Class III treatment. Early or late? Angle Orthod 53: 175-191.
- Creekmore TD (1978) Class III treatment planning. J ClinOrthod 12: 650-655.
- Janson G, de Souza JE, AlvesFde A, Andrade P Jr, Nakamura A, et al. (2005) Extreme dentoalveolar compensation in the treatment of Class III malocclusion. Am J OrthodDentofacialOrthop 128: 787-794.
- Kondo E, Arai S (2005) Nonsurgical and nonextraction treatment of a skeletal class III adult patient with severe prognathic mandible. World J Orthod 6: 233-247.
- Hisano M, Chung CR, Soma K (2007) Nonsurgical correction of skeletal Class III malocclusion with lateral shift in an adult. Am J OrthodDentofacialOrthop 131: 797-804.
- Daher W, Caron J, Wechsler MH (2007) Nonsurgical treatment of an adult with a Class III malocclusion. Am J OrthodDentofacialOrthop 132: 243-251.
- Bilodeau JE (1997) [Treatment of class III severe malocclusion with orthodontics and oral surgery]. OrthodFr 68: 111-120.
- Ishikawa H, Nakamura S, Iwasaki H, Kitazawa S, Tsukada H, et al. (2000) Dentoalveolar compensation in negative overjet cases. Angle Orthod 70: 145-148.
- Lin J, Gu Y (2003) Preliminary investigation of nonsurgical treatment of severe skeletal Class III malocclusion in the permanent dentition. Angle Orthod 73: 401-410.
- Frank CA (1993) An American Board of Orthodontics case report: the nonsurgical orthodontic correction of a Class III malocclusion. Am J OrthodDentofacialOrthop 103: 107-114.
- Grainger RM (1967) Orthodontic treatment priority index. Vital Health Stat 2 : 1-49.
- Ghafari J, Locke SA, Bentley JM (1989) Longitudinal evaluation of the Treatment Priority Index (TPI). Am J OrthodDentofacialOrthop 96: 382-389.
- Dahlberg G (1940) Statistical methods for medical and biological students.Interscience, New York, USA.
- Houston WJ (1983) The analysis of errors in orthodontic measurements. Am J Orthod 83: 382-390.
- Hiller ME (2002) Nonsurgical correction of Class III open bite malocclusion in an adult patient. Am J OrthodDentofacialOrthop 122: 210-216.
- Ishikawa H, Nakamura S, Iwasaki H, Kitazawa S, Tsukada H, et al. (1999) Dentoalveolar compensation related to variations in sagittal jaw relationships. Angle Orthod 69: 534-538.
- Mora DR, Oberti G, Ealo M, Baccetti T (2007) Camouflage of moderate Class III malocclusions with extraction of lower second molars and mandibular cervical headgear. ProgOrthod 8: 300-307.
- Richmond S, Shaw WC, Roberts CT, Andrews M (1992) The PAR Index (Peer Assessment Rating): methods to determine outcome of orthodontic treatment in terms of improvement and standards. Eur J Orthod 14: 180-187.
- Shaw WC, Richmond S, O'Brien KD, Brook P, Stephens CD (1991) Quality control in orthodontics: indices of treatment need and treatment standards. Br Dent J 170: 107-112.
- Parkinson CE, Buschang PH, Behrents RG, Throckmorton GS, English JD (2001) A new method of evaluating posterior occlusion and its relation to posttreatmentocclusal changes. Am J OrthodDentofacialOrthop 120: 503-512.
- Hamdan AM, Rock WP (1999) An appraisal of the Peer Assessment Rating (PAR) Index and a suggested new weighting system. Eur J Orthod 21: 181-192.
- Ferro A, Nucci LP, Ferro F, Gallo C (2003) Long-term stability of skeletal Class III patients treated with splints, Class III elastics, and chincup. Am J OrthodDentofacialOrthop 123: 423-434.
- McNamara JA Jr, Seligman DA, Okeson JP (1995) Occlusion, Orthodontic treatment, and temporomandibular disorders: a review. J Orofac Pain 9: 73-90.
- Saito I, Yamaki M, Hanada K (2005) Nonsurgical treatment of adult open bite using edgewise appliance combined with high-pull headgear and class III elastics. Angle Orthod 75: 277-283.
- Proffit WR, Fields HWJ (2000) Contemporary orthodontics. Mosby, St Louis, USA.
- Janson G, Barros SE, de Freitas MR, Henriques JF, Pinzan A (2007) Class II treatment efficiency in maxillary premolar extraction and nonextraction protocols. Am J OrthodDentofacialOrthop 132: 490-498.
- Nangia A, Darendeliler MA (2001) Finishing occlusion in Class II or Class III molar relation: therapeutic Class II and III. AustOrthod J 17: 89-94.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 16299
- [From(publication date):
December-2014 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 11589
- PDF downloads : 4710