Epidermoid cyst of the parotid gland: Report of a rare case with literature review
Received: 28-Dec-2022 / Manuscript No. ocr-22-52727 / Editor assigned: 31-Dec-2022 / PreQC No. ocr-22-52727 / Reviewed: 16-Dec-2022 / QC No. ocr-22-52727 / Revised: 21-Dec-2022 / Manuscript No. ocr-22-52727 / Accepted Date: 21-Dec-2022 / Published Date: 28-Dec-2022 DOI: 10.4172/2161-119X.1000451
Abstract
Epidermoid cyst (EC) of the parotid gland is a benign pathology rarely encountered by otolaryngologist. It is usually mistaken for an abscess, neoplasm or other cysts including cystic neoplasm. It can get infected, mimicking an abscess or causes a facial nerve palsy which is very rare. MRI and fine needle aspiration cytology (FNAC) are important examinations for the diagnosis. Total excision of the cyst is the gold standard treatment. Recurrence is unusual. Malignant transformation has been reported in history. This entity should be considered by clinicians when faced to a gradually growing painless swelling in the parotid gland. In our literature review for the past 25 years, we have collected 13 cases in additional to ours. In this paper we report a case of congenital EC of the parotid gland in a 71 year old patient and we present a literature review for this pathology.
Keywords
Epidermoid cysts; parotid gland
Introduction
Epidermoid cysts are benign and frequent tumor like lesions. They can be found anywhere in the body, but most commonly seen in the skin. They can be congenital or acquired. If congenital, they develop out of the ectodermal tissue in areas where embryonic elements fuse together [1, 2]. If acquired, they arise from epithelial implantation after trauma or surgery [3]. Epidermoid cysts in the salivary glands are very rare entities. Literature search for the past 25 years revealed only very few cases in parotid gland and some cases in submandibular gland [4]. Epidermoid cyst of the parotid gland can be easily mistaken for an abscess, neoplasm or other cysts due to its rarity [5].
That’s why we are discussing, throughout a case observed in our ENT department, the diagnostic dilemma and treatment of this condition with a literature review for the majority of cases reported in the past 25 years.
Case Report
A 71 year old male, presented to our outpatient department with a painless swelling in the left retro auricular region. It increased gradually in size over 11 months. There were no episodes of infection or inflammation of the swelling. The medical history of the patient was insignificant (no history of trauma or surgery in the ear and facial region).
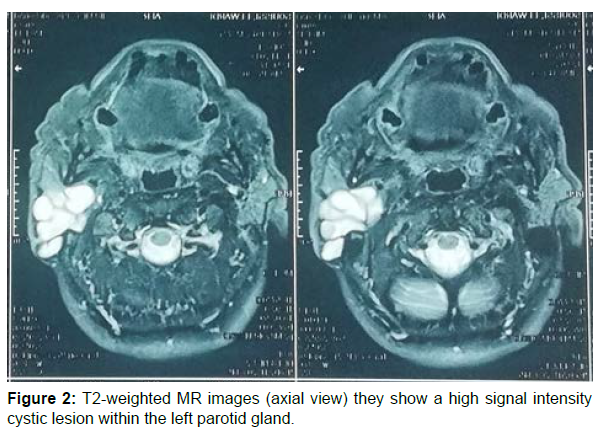
Examination revealed an approximately 7cm mass over the region of the left mastoid. On palpation it was mobile, ferm and painless. The skin over the swelling was normal and pinchable. No lymph nodes were found, facial nerve function was normal. No additional pathologies were observed in the ear, nose, throat and general examination. An Ultrasound and a MRI were performed, they showed a polylobed well encapsulated cystic lesion of the deep and superficial lobes of the left parotid with extension to the retro auricular region. The lesion gave a high intensity signal on T2 evoking a pleomorphic adenoma (Figures 1 and 2). Echo-guided fine needle aspiration of the swelling was also in favor of a cystic pleomorphic adenoma.
The patient underwent a superficial parotidectomy. After exposing the gland, pultaceous debris were found in (Figure 3).
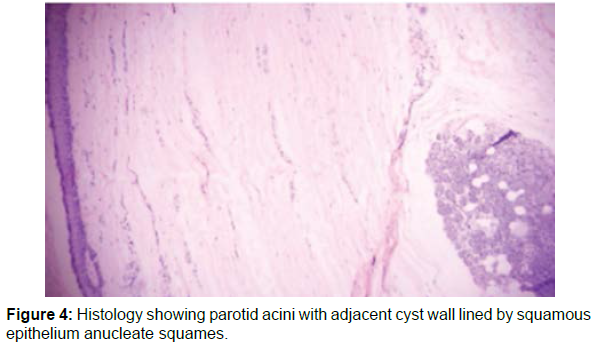
The post-operative period was uneventful. Histopathologic examination of the specimen revealed an epidermoid cyst of the parotid gland (Figure 4).
In six month of follow up, the patient had no complaints and he showed no signs of recurrence.
Discussion
Epidermoid cyst is defined as a simple cavity lined with an epidermis-like epithelium and filled with keratin debris. It develops intradermal or subcutaneously. It is a common benign skin lesion that could be found anywhere in the body [6]. It is most commonly found in the ovary and testicle, rarely in the head and neck region, where they represent only 7% of all ECs of the body [5].
In the parotid gland, cysts are very rare entities. They only account for 5% of all parotid tumors, most of which are the cystic component of neoplasm [7, 8]. The incidence of ECs in the parotid gland is unknown, according to PANNA N HEGDE et al only a few case reports of this pathology were published in the world literature. In a series of 708 parotidectomy reported by Richardson, 23 cystic lesions were found, only two were inclusion epidermoid cysts [9]. In our literature review we have encountered a total of 13 cases in the past 25 years in addition to ours, which make it an extremely rare pathology.
ECs of the parotid gland can be congenital or acquired. Congenital cysts are usually caused by a developmental failure in the separation of the surface ectoderm and neural tube which causes an entrapment of epithelial remnants [5, 10].
Acquired cysts arise from implantation and encystment of a viable epidermal fragment. The main risk factors are trauma, surgery or biopsy. Out of the 13 cases we have encountered, 5 were acquired cysts [8, 11]. Thompson et al described a case of EC six months after Myringoplasty with endaural incision [11]. He highlighted the fact that incisions in the skin around the ear escalate the risk of developing EC in the parotid gland. Another case of iatrogenic EC in the parotid gland following botulinum toxin injection in the masseter muscle was reported by Choong-Sang Lee [12].
Patient complaints are associated to a slow growing painless mass recognized as early as 3 months to 10 years. Physical examination usually shows a painless swelling, mobile and non-tender with or without fluctuation [13]. The skin overlying the mass is normal and pinchable [4]. Most cases reported in literature had no facial nerve paralysis or pathological lymph nodes in examination, like our patient. But in case of infection, cysts could become warm, red and tender. Sirikamakshi et al reported a case of infected EC of the parotid gland; the patient had fever and trismus, on palpation the lesion was firm, non-tender and well defined. They pointed out to the fact that if cysts stay longer without surgical remove they may get infected. M.Streppel et al also reported a rare case of facial palsy caused by an infected EC of the parotid gland. The reason of paralysis was believed to be the spread of inflammation from the parotid gland into the fallopian canal through the stylomastoid foramen, simulating Bell’s palsy. Facial nerve was not enclosed by the cyst.
Establishing a final diagnosis and determining the benign or malignant processes of the lesion preoperatively is challenging. Imaging, FNAC and excision biopsy are key examinations. Ultrasound scan normally shows a well-encapsulated avascular hypoechoic mass. In our case the mass had a polylobed contour and a vascular flow, which is untypical. MRI is the best imaging modality to assess a parotid tumor; it determines the location, the number of lesions, the signal features and the extension to facial nerve [14]. If done, it shows a well circumscribed mass with a high T2 signal and a thin enhancement in the contrastenhanced T1W images. Fine needle aspiration cytology is the most reliable and the least expensive tool for diagnosing parotid cysts. But the rate of inadequate sampling and false negative results is increased in cystic lesions compared with solid tumors [10]. Out of 13 case reports collected, 33% of cases had a successful preoperative diagnosis showing a sheet of benign squamous cells in a background of mild inflammatory infiltrate. In 60% of cases FNAC was not preformed. Omer Aydin et al reported a case of a cytologic atypia of uncertain malignancy and the final diagnosis was only made after histopathological examination [12].
And finally, in 8% of cases the aspiration was non-diagnostic. Surgical excision of the cyst is the gold standard treatment. It must be prudent to preserve important structures such as facial nerve and to prevent the rupture of the cyst which can lead to postoperative inflammation. In almost all cases reviewed the treatment was superficial parotidectomy, Srikamakshi et al described a case of EC involving the deep lobe of the parotide gland which needed a total parotidectomy. There are reports in the literature of malignant changes in epidermoid cysts, that’s why surgical removal of the cyst is essential. Final diagnosis is made based on histopathological features. Recurrence is uncommon [15].
Conclusion
To conclude, EC of the parotid gland is a very rare pathology, with very few cases having been mentioned in literature. It is important for clinicians to be aware of this possible diagnosis, as it can be mistaken for an abscess, neoplasm or other cysts including cystic neoplasm.
Diagnosis is based on imaging and FNAC. Complete excision is necessary to prevent recurrence.
References
- Hegde PN (2013) A Rare Case of an Epidermoid Cyst in the Parotid Gland-which was Diagnosed by Fine Needle Aspiration Cytology. J Clin Diagn Resn 7: 550-552.
- Mahalakshmi S, Reddy S, Ramamurthy TK, Shilpa B (2016) Rare Locations of Epidermoid Cyst: Case Reports and Review. J Health Sci 26:595-601. doi:10.4314/ejhs.v26i6.14
- Ganesan A, Nandakumar GK (2015) Epidermal Cyst of Parotid Gland: A Rarity and a Diagnostic Dilemma. Case Rep Dent: 1-3. doi:10.1155/2015/856170
- Hoang VT, Trinh CT, Nguyen CH, Chansomphou V, Chansomphou V, et al. (2019) Overview of epidermoid cyst. J Radiol Open 6:291-301. doi:10.1016/j.ejro.2019.08.003
- Ozcan KM, H Dere, I Ozcan, T Gun, T Gun (2006) an epidermal cyst in the parotid gland following ear surgery: a case report. J oral medi 2:193-195.
- G S Richardson, A A Clairmont, E R Erickson (1978) Cystic lesions of the parotid gland. Plast Reconstr Surg 61:364-370.
- Cho Y, Lee D-H (2017) Clinical Characteristics of Idiopathic Epidermoid and Dermoid Cysts of the Ear. J Audiol Otol 21:77-80.
- Thompson AC, Bradley PJ (1991) Iatrogenic epidermoid cyst of the parotid region following ear surgery. J Laryngol Otol 105: 227-228.
- Lee CS, Kim HK, Lim JH, Jeon KJ, Huh JK (2011) Iatrogenic epidermoid cyst in the parotid gland: A case report. J Korean Assoc Oral Maxillofac Surg 37:237-240.
- Manz D, Bankfalvi A, Lehnerdt G (2011) Epidermoidzyste als Raumforderung der Glandula parotis. HNO 59:64-67.
- Yigit N, Karslioglu Y, Yildizoglu U, Karakoc O (2015) Dermoid Cyst of the Parotid Gland: Report of a Rare Entity with Literature Review. Head Neck Pathol 9:286-292.
- Thiagarajan SKB (2013) A cheesy affair! - Report of a case of an epidermoid cyst of parotid. J Ocr 3.
- Streppel M, Thomas JP, Stennert E, Guntinas-Lichius O, Wagner M (2001) Infizierte Epidermoidzyste als Ursache einer peripheren Fazialisparese. Laryngo Rhino Otol 80:617-619.
- Faheem MH, Shady S, Refaat MM (2018) Role of magnetic resonance imaging (MRI) including diffusion weighted images (DWIs) in assessment of parotid gland masses with histopathological correlation. J Radiol Nucl Med 49:368-373.
- Pantanowitz L, Thompson LDR, Rossi ED (2018) Diagnostic Approach to Fine Needle Aspirations of Cystic Lesions of the Salivary Gland. Head Neck Pathol 12:548-561.
Indexed at, Google scholar , Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Samia M (2022) Epidermoid cyst of the parotid gland: Report of a rare case with literature review. Otolaryngol (Sunnyvale) 12: 451. DOI: 10.4172/2161-119X.1000451
Copyright: © 2022 Samia M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2698
- [From(publication date): 0-2022 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 2195
- PDF downloads: 503