Epidemiology of Leishmaniasis in Lattakia City among last Ten Years (2006-2016)
Received: 18-Sep-2017 / Accepted Date: 26-Sep-2017 / Published Date: 06-Oct-2017 DOI: 10.4172/2161-1165.1000325
Abstract
Background: Leishmaniasis is a major health problem in developing countries.
Aim: Studying the effect of Syrian War on the epidemiology and control of Leishmaniasis cases in Lattakia city.
Methods and materials: It was retro-spective study of the new reported cases of Cutaneous and Visceral Leishmaniasis in Lattakia during a peroid of 10 years (2006-2016). Methods of diagnosis were Giemsa stained microscopy for CL and VL cases. All patients treated with pentavalent antimonial compounds.
Results: At the beginning of Syrian War (2012-2016) we reported 2999 new cases of CL and 81 new cases of VL in Lattakia.
Conclusion: Syrian War has increased the incidence rate of Leishmaniasis in Lattakia.
Keywords: Leishmaniasis; Health; Diagnosis; Syria
Abbreviations
CL: Cutaneous Leishmaniasis; VL: Visceral Leishmaniasis
Introduction
Leishmaniasis consists of a complex of vector-borne diseases caused by more than 20 species of the protozoan genus Leishmania and is transmitted by sand fly vectors [1]. Clinical manifestations range from cutaneous ulcers to systemic multiorgan disease. Leishmania organisms are endemic in scattered foci in more than 80 countries on every continent except Australia and Antarctica [2]. According to WHO estimates from 2007 to 2011. Syria is the sixth country among 10 countries with the highest estimated case count of CL [3]. Until 1960, cutaneous leishmaniasis prevalence in Syria was restricted to 2 areas to which it is endemic (Aleppo and Damascus); preconflict (c. 2010) incidence was 23,000 cases/year [4]. However, in early 2013, an alarming increase to 41,000 cutaneous leishmaniasis cases was reported [4,5]. 6,500 cases occurred in Al Raka, because these places are not historical hotspots of CL, this change might be attributed to the massive human displacement within Syria and the ecologic disruption of sand fly (Ph. papatasi) habitats [6].
Methods
Our study was retro-spective study on new reported cases of Cutaneous and Visceral Leishmaniasis in Lattakia between 2006–2016 years. Data were collected from the Leishmaniasis and Contagious Diseases Center which is affiliated to WHO in Lattakia for all new reported cases between 2006–2016 years. We divided the ten years to two 5 year phases. The first phase (2006-2011) is before the Syrian War and the second phase (2012-2016) is after the War. We observed the effects of Syrian War on the incidence rate of Leishmaniasis in Lattakia. We excluded chronic, recurrence and partially treated cases. In our study we use Giemsa stained microscopy of specimens (cutaneous biopsies for CL and bone narrow aspiration for VL). All cases were treated by pentavalent antimonial compounds.
Results and Discussion
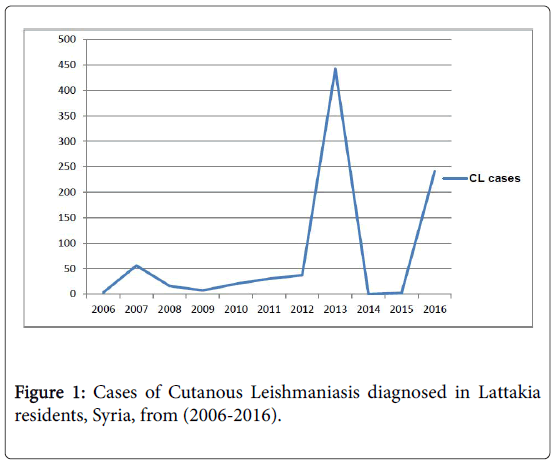
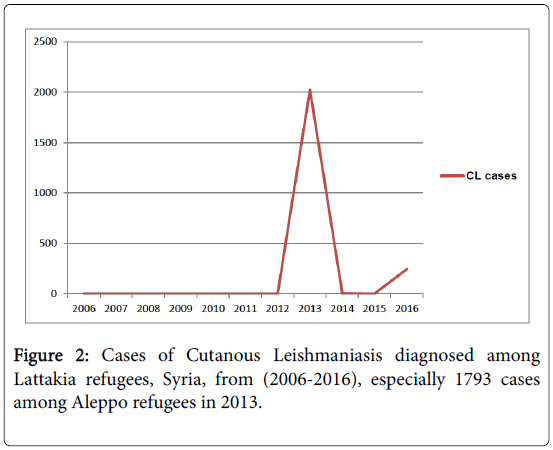
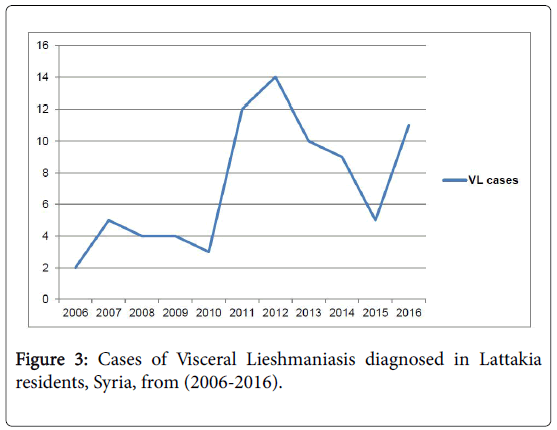
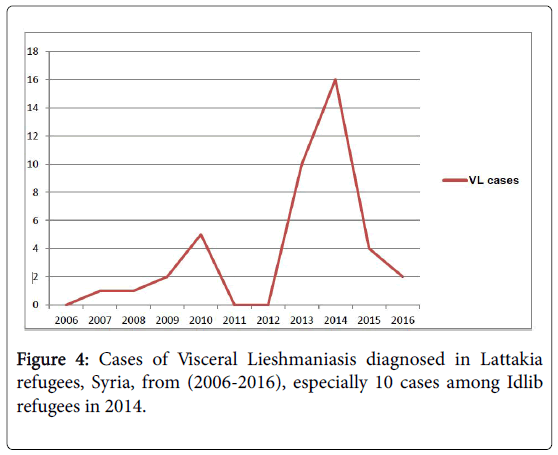
We observed 133 acute cases of CL 99.25%) of cases were from Lattakia and 0.75% were from Tartous) (Figure 1) and 39 new cases of VL (76.92% of cases were from Lattakia, 23.08% were from Idlib and Tartous) between (2006-2011) (Figure 2). Of the 133 CL cases, 87 were among males and 55 among females. Of the 39 VL cases, 16 were among males and 23 among females. We found that the highest incidences (39.84%) were among adult (20-39 year old) for the CL (Table 1) and (64.12%) for VL were among children (1-3years) (Table 2). Whereas between (2012-2016), we observed 2999 new cases of CL (64.16% of cases were from Aleppo and 35.84% of cases were from other cities) (Figure 3) and 81 new cases of VL (60.49% were from Lattakia, 39.51% were from other cities) (Figure 4). There Were 1628 males and 1371 females of CL cases, and according to VL cases: 37 males and 44 females. We found that 37.30% of CL patients were between 20-39 years (Table 1) and 48.18% of VL patients were between 1-3 years (Table 2). Syrian War has increased both CL and VL cases. 1793 cases of CL especially among Aleppo refugees in 2013. Unfortunately, there is no accurate census of Lattakia due to constant change in the population because of ongoing relocating and the increase of the death. In addition to collecting data may be is not punctual, because long duration of our study (10 years). We confirm that patient’s collaboration, early detection and diagnosis were important to ensure the effective delivery of treatment and successful control of this epidemic.
| Age groups | Cases (2006-2011) | Percent (%) | Cases (2011-2016) | Percent (%) |
|---|---|---|---|---|
| 0-4 | 7 | 5.26 | 292 | 9.73 |
| 5-9 | 15 | 11.27 | 498 | 16.6 |
| 10-19 | 35 | 26.31 | 604 | 20.14 |
| 20-39 | 53 | 39.84 | 1118 | 37.3 |
| 40-59 | 12 | 9.02 | 376 | 12.53 |
| 60< | 11 | 8.27 | 111 | 3.7 |
| Total number | 133 | 2999 |
Table 1: Cases of Cutaneous Leishmaniasis diagnosed in Lattakia governorate, Syria, according to age from (2006-2016).
| Age groups | Cases (2006-2011) | Percent (%) | Cases (2011-2016) | Percent (%) |
|---|---|---|---|---|
| 1 > | 3 | 7.69 | 16 | 19.75 |
| 3-1< | 25 | 64.12 | 39 | 48.18 |
| 5-4 | 4 | 10.25 | 11 | 13.58 |
| 7-6 | 0 | 0 | 4 | 4.93 |
| 9-8 | 1 | 2.56 | 1 | 1.23 |
| 12-10 | 1 | 2.56 | 2 | 2.46 |
| 18-13 | 0 | 0 | 0 | 0 |
| 18< | 5 | 12.82 | 8 | 9.87 |
| Total number | 39 | 81 |
Table 2: Cases of Visceral Leishmaniasis diagnosed in Lattakia governorate, Syria, according to age from (2006-2016).
Acknowledgements
I thank everyone who helps me at Leishmaniasis and Contagious Diseases Center, Dr. Zuheir Al Shehabi, MD, PHD, FASCP, Faculty of Medicine – Tishreen University and Dr Tamim Khromachou, MD, Clinical Assistant Professor of Family & Community Medicine, HealthPros.
References
- Jeronimo SMB, de Queiroz Sousa A, Pearson RD (2006) Leishmaniasis. In: Tropical infectious diseases: principles, pathogens and practice. Guerrant RL, Walker DH, Weller PF (editors), Churchill Livingstone Elsevier, Edinburgh, Scotland.
- Choi CM, Lerner EA (2001) Leishmaniasis as an emerging infection. J Investig Dermatol Symp Proc 6: 175.
- Alvar J, Vélez ID, Bern C, Herrero M, Desjeux P, et al. (2012) Leishmaniasis Worldwide and Global Estimates of Its Incidence. PLoS One 7: e35671.
- Hayani K, Dandashli A, Weisshaar E (2015) Cutaneous leishmaniasis in Syria: Clinical features, current status and the effects of war. Acta Derm Venereol 95: 62-66.
- Haddad N, Saliba H, Altawil A, Villinsky J, Al-Nahhas S (2015)Cutaneous leishmaniasis in the central provinces of Hama and Edlib in Syria: Vector identification and parasite typing. Parasit Vectors 8: 524.
- Al-Salem WS, Pigott DM, Subramaniam K, Haines LR, Kelly-Hope L,et al. Cutaneous leishmaniasisand conflict in Syria.Emerg Infect Dis 22.5 (2016): 931.
Citation: Hawat M, Husein M, Almahmoud I (2017) Epidemiology of Leishmaniasis in Lattakia City among last Ten Years (2006-2016). Epidemiology (Sunnyvale) 7: 325. DOI: 10.4172/2161-1165.1000325
Copyright: © 2017 Hawat M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5076
- [From(publication date): 0-2017 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 4300
- PDF downloads: 776