Review Article Open Access
Epidemiology, Driving Factors, Transmission and Control Options of Zika Virus: A Review
Getahun Asebe*
Department of Animal Science, Gambella University College of Agriculture and Natural Resource, Ethiopiaa
- *Corresponding Author:
- Getahun Asebe Gulich
Department of Animal Science
Gambella University College of Agriculture and Natural Resource, Ethiopia
Tel: 251911571579
E-mail: getahunasebe@gmail.com
Received date: April 06, 2016; Accepted date: April 20, 2016; Published date: April 26, 2016
Citation: Gulich GA (2016) Epidemiology, Driving Factors, Transmission and Control Options of Zika Virus: A Review. J Infect Dis Ther 4:278.doi:10.4172/2332-0877.1000278
Copyright: © 2016 Gulich GA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Infectious Diseases & Therapy
Abstract
Now days, the threats of infectious diseases particularly that emerges and or re-emerges is increasing. The main sources of emerging and re-emerging diseases originated from both wild and domestic animals. From few years onwards, diseases such as HIV/AIDS, SARS, Rift Valley fever, Influenza, Ebola, and so like, become the risks of the world. This paper deals about the recently re-merged diseases known as Zika fever. This disease is caused by a virus known as flavivirus and carried from one individual to another through a mosquito called Aedes causes this disease. The viral epidemiology covers the Americans, Africa, Asia and the pacific. Though not all the reservoir hosts are clearly identified, authors in general agreed the primates are the main reservoirs. Researchers tried to identify the driving factors of Zika virus infection as climatic condition, presence of vectors, the environmental ecology, travelling histories, urbanization and so like. Individual persons infected by Zika virus will show symptoms such as mild fever, rashes on the skin, inflammation of conjunctiva, pain on the muscle and joint, headache. The symptoms may normally stay from the minimum day 2 to twelve days. Currently the disease has no treatment and viral prevention; only it relies on the protection of the mosquito bite. Special precaution steps should be taken in cases of pregnant women and who intend to recently pregnant.
Keywords
Zika virus; Emerging; Re-emerging; Driving factors; Aedes
Introduction
Due to various reasons and factors recently, zoonotic diseases such as AIDS/HIV, EBOLA, SARS, Rift Valley Fever and the like are emerging and re-emerging and causing great threat for the world [1,2]. One of the recently re-emerging viral diseases is Zika which is family member of called flaviviridae and genus flavivirus, which is transmitted by daytime active mosquito called Aedes with the two most common known species as A. aegypti , A. albopictus that bite at night period. Historically the name Zika came from the natural forest found in Uganda Zika forest where the virus first isolated in 1947 [3,4]. The Zika virus causes Zika fever characterized with no or mild symptoms. Epidemiologically, the Zika virus gradually disseminated from the African continent to Asia within a narrow equatorial belt since 1950s. The virus then spread across eastward to the Pacific Ocean to French Polynesia then to Easter Island in 2014. In 2015, the virus spread to Mexico Central America, the Caribbean and South America, where the Zika outbreak has reached the pandemic stage [5-8].
Before, researchers did not think this disease as a problematic, because in Zika infection, the symptoms will go away within a week. About 80% of the people may not develop any symptoms after Zika virus infection. In Zika infection, admission and hospitalization is not common and death is rare. Despite there is no as such fatality reports from the Zika virus before, recently the issue of the virus becomes too sensitive due to the research findings showed, there is a high suspicion of causing a “Microcephaly” and intracranial calcifications (calcium deposits in the brain). The study evidence revealed by the public health officials there is a link between the virus infection and the birth defects in the newborns and the neurological abnormalities in the adults. According to the Brazil Ministry of Health (2015) information the country documented an estimated of 3500 cases of microcephaly and intracranial calcifications. This review paper tried to reveal the epidemiology, driving factors, transmission and control options of Zika virus.
Historical Background of Zika Virus
Zika is among the present emerging viral disease of family called flaviviridae and genus flavivirus, which is transmitted by daytime active mosquito called Aedes with the two most common known species as A. aegypti , A. albopictus also may bite at night period. The name Zika came from the natural forest found in Uganda Zika forest where the virus first isolated in 1947 [3,4].
Literatures documented that during scientists conducting yellow fever study in Uganda at the Zika forest in 1947 accidentally they also observed a fevered rhesus macaque placed in a cage near the East African Virus Research Institute in Entebbe. The monkey that kept for yellow fever study purpose developed a fever, and researchers isolated from its serum a transmissible agent that was first described as Zika virus in 1952 [3]. Following the virus isolation, the first Zika virus case reported in human being in Uganda and in Tanzania in 1954 [9].
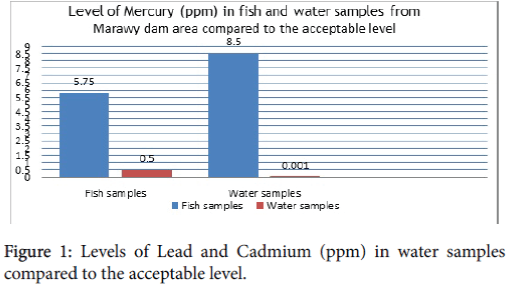
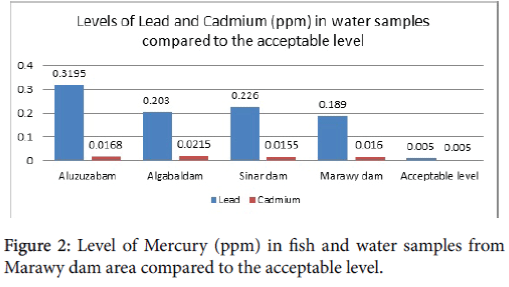
Before 2007, there were rare reports of confirmed cases of Zika virus infection from the Africa and Southeast Asian continent. Later on in 2007, major epidemic occurred in Yap Island (Micronesia) which involved about 5000 persons [10,11] and Gabon [12]. The outbreak on the island of Yap in the Federated States of Micronesia in April 2007 was the first to occur outside of Africa and Asia (Figure 1). The first outbreak of the disease outside of Africa and Asia was in April 2007, on the island of Yap in the Federated States of Micronesia (see figure 1).
The virus has spread to the South and Central America and the Caribbean since April 2015. Starting from the early 2016, a widespread outbreak of Zika virus is actively flourishing in the Americas. Since the early of April 2015, the virus started in Brazil and then continued to other areas of the South America, Central America, Mexico and the Caribbean [14]. From January 2016, the CDC gives frequent alert for travellers, pregnant women and who have the intension to be pregnant. WHO alerted the virus could likely to spread further throughout most of America at the end of 2016 [14].
Impact of Zika Virus
The illness after Zika virus is not a life threating, it is serious mainly because of its link to the birth defect microcephaly where babies to be borne with abnormally small heads and adults with neurological signs [15]. Even though the virus is not life threating as such, WHO declared the Zika virus an international public health emergency. According to the WHO notification, the virus is spreading alarmingly since April 2015 onwards. About 4 million people in Americas will be infected at the end of 2016 and Brazil 4000 cases of infants with severe birth defects are expected.
Driving factors and the disease current epidemiology
Climatic condition and weather
Directly or indirectly, the weather conditions are important in infectious diseases occurrences and incidences. For Zika virus occurrences, scientist suggest various driving factors for example rising temperature (abnormal warming) which leads to increased incidence of mosquito-borne infections. For instance, El Niño is one of the factors that bring heavy rain resulting creating good opportunity for mosquito reproduction and multiplication site. Many scientists related the global warming to coincide with the current Brazil Zika infection outbreak in early 2016 with El Niño, phenomena that happened in the Pacific Ocean, especially along the coast of South and Central America. However, the relationship of mosquito number with increased temperature is biological, means it might favor mosquito reproduction and/or increase their contact with humans (to look for blood meal in case of female Aedes aegypti ), which might favor Zika transmission [16-18]. Some scientists to global warming are attributing the rapid spread of the virus, will help virus to reproduce faster, emerge earlier in the season, survive longer and even spread to cooler areas of the world [16,19,20]. Presence of high rainfall is a positive indicator of Zika virus infection from a study done by Alto and Juliano [21]. Therefore, scientists explained and warned that increased temperature could have a significant public health risk with the potential for the increased transmission of mosquito-borne diseases like Zika virus.
Changes in climatic conditions, creates suitable conditions by lengthen its biting season that result a pandemic potential condition for further devastations and disease carrying mosquitoes will thrive as the climate warms [18,22,23].
The other perspective is; during warm condition, working hours will be changed and people will be forced to go early in the morning and stay until evening at night. In addition, the type of clothing will also be changed helping mosquitoes to bite human. When the disease complex dynamicity seen from the Environmental Health Perspective point of view; climate may influence disease ecology at many levels, which cannot be easily modeled or understood. Besides, human factors such as behavior, immunity and socioeconomic influences also adds for the complex relation of the disease-human and environment [19,24].
The vectors
Regarding the vector distribution, there might be a slight increase in the range of the mosquito vector, Aedes aegypti , and also Aedes albopictus , moving northward in the Northern Hemisphere and southward in the Southern Hemisphere comparing to the previous vector presence history. The movement of mosquito is related directly with Zika virus infection provided that an infected case present [25]. Studies for instance by Brazilian scientists showed that the Aedes aegypti mosquito has spread to 80 percent of the country, an area of 6.9 million sq km (2.6 million square miles) four times larger than a decade ago (Figure 2). Besides, a study report from Senegal showed there is an association between the viral isolation and mosquitos’ abundance [26].
The ecosystem and other factors
The virus is explosive and unprecedented pace in the pandemic reemergence nature [27]. Therefore, knowing the associated driving factors is unquestionable. There is an association between deforestation, mosquito vector factors and the susceptibility of migrants compared with indigenous people in affected areas of the world. Swampy and watery areas facilitate the vector to reproduce in the area; hence, it directly relates and facilitates the Zika virus spread in that particular area [16,28]. For instance, flooding resulted after drought leads to collecting of pools of water, consequently mosquitoes will have good breeding ground accompanied by the warmer temperature [29,30]. Besides warming temperatures, vector presence and abundance, considering environmental factor the socioeconomic factors such as population growth, poverty and the related environmental consequences issues should be considered. For example, the abandoned of DDT for insect control helped the reemergence of many of these annoying tropical diseases [29,30]. When the population grows, people starts to invade new areas, the rural areas became changed to urban which is a major driver of the Zika virus epidemics, and consequently more cases of microcephaly in infants will be seen [30,31].
Travelling effect
Another recent second larger outbreak of Zika virus outside Africa and Asia was confirmed in April 2015, in Brazil that is suspected linked to 2014 FIFA World Cup and coupled with the large population of insect vectors such as Aedes aegypt (main vector) and Aedes albopictus (Asian tiger) mosquitoes that inhabit the region. Currently, it is common to see an increased global travelling phenomena hence, it easy for an infection occurred in one geographical location shortly in another continent [18,22,29,32]. Due to globalization effect, travelling to infected areas due to various activities contribute for the acquiring of the infection easily [17]. There is high frequency of international travel probably help for rapid spread of the infection globally. Due to various factors such as war, poverty, and investment activities, the global people movement increased, as the same time infectious agents will easily travel across the globe [32,33].
Urbanization
Recent experience from Brazil showed urbanization contributes for the large outbreak of Zika virus. Urban areas where dense population living in close proximity and a lot of mosquito present, the efficiency of Zika Virus to pass from infected to healthy person in the availability of infected individual is high. Due to the population growth of the world increases alarmingly, now days it is too common to see a rapid urbanization. Community based rapid urbanization will result in unplanned urbanization consequently people will be found in remote, vector infested areas [34]. This rapid urbanization will force people to invade new areas that have not been visited for dwelling before. Rapid urbanization will easily predispose people for easy infection [33]. Hence, increasing urbanization and poverty creates a fertile environment for the infection [35], which results in urban epidemics [36].
Current geographical distribution of Zika virus
Since the 1947 where first Zika was known, case of Zika fever was seen on rhesus monkey in the Zika Forest in Uganda. Then, the virus spread gradually and continuously covers wide ranges of area. A population surveys done in Uganda at that time resulted 6.1% prevalence [13]. In recent time, the virological studies, seroprevalence surveys, diagnosis of sporadic cases, and epidemics have allowed identifying the virus epidemic cases seen different parts of the world extending from Africa, to America and Asia (See Table 1).
| Geographical location of Zika Virus | Countries reported | Reported by |
|---|---|---|
| Arica | Senegal, Uganda, Nigeria, Ivory Coast, Gabon, Tanzania, Egypt, Central African Republic, Sierra Leone, etc | Grard et al. [12]; Hayes [37]; Robin and Mouchet [38]; Jan et al. [39]; Saluzzo et al. [40]; Saluzzo et al. [41]; Diallo et al. [42] |
| Asia | Cambodia, India, Indonesia, Malaysia, Pakistan, Philippines, Singapore, Thailand, and Vietnam, Japan | Robin and Mouchet [38]; Olson et al. [43]; Tappe et al. [44] ; Kutsuna et al. [45] |
| Oceania | Ledermann et al. [46] | |
| Paciï¬c | Micronesia/Yap, FP, New Caledonia/south pacific, and Cook islands, French Polynesia | Hayes [37]; Musso et al. [47,48] |
| Europe | Germany | Tappe et al. [44] |
| America | Brazil, Barbados, Colombia, Ecuador, El Salvador, French Guiana, Guatemala, Guyana, Haiti, Honduras, Martinique, Mexico, Panama, Paraguay, Puerto Rico, Saint Martin, Suriname, and Venezuela |
Marcondes and Ximenes [49]; PAHO/WHO [50] |
Table 1: Geographical location of the Zika Virus distributions.
Major outbreaks of Zika Virus
In history, first major outbreak was reported in 2007 in the Yap Islands of the Federated States of Micronesia with 185 confirmed cases. In this outbreak, 108 cases were confirmed by PCR or serology and 72 additional cases were suspected. In the confirmed cases, symptoms such as rash, fever; arthralgia and conjunctivitis were seen with no deaths at all. The main vector suspected for the transmission of the virus in the Yap state during the outbreak was probably be the Aedes hensilli mosquito. In regarding how the virus is introduced in the Yap Island still remain uncertain in which it may be through the infected mosquitoes or a viraemic human with a strain related to Southeast Asia. The Yap Island case was also the first time Zika fever had been reported outside Africa and Asia [10,13,51].
In 2013, another large outbreak was reported in French Polynesia that was thought to be from an independent introduction of the virus from Asia than the Yap Island outbreak [52]. Mosquito-borne virus diseases in the Pacific Region have a distinct epidemiology due to small populations scattered over thousands of tropical and sub-tropical islands on both sides of the equator in relative geographic isolation, together with (nowadays) significant people’s mobility and thereby exposure to circulating arboviruses through the airline networks of the Asia-Pacific Region [24].
In the American continent, the first case of indigenous transmission reported in Chile (Easter Island) since February to June 2014. Twentyfour countries in South and Central America have reported cases of microcephaly [53]. For Brazilian, May 2015 was a historic month, because of; the Pan American Health Organization (PAHO) issued an alert regarding the first confirmed autochthonous Zika virus transmission. Unknowingly the virus infected people before the government notifies any confirmed cases, yet Zika like symptoms were reported in 14 states of Brazil (Alagoas, Bahia, Ceará, Maranhão, Mato Grosso, Pará, Paraíba, Paraná, Pernambuco, Piauí, Rio de Janeiro, Rio Grande do Norte, Roraima, and São Paulo). Later on, mosquito-borne Zika virus is suspected to be the cause of 2,400 cases of microcephaly and 29 infant deaths in Brazil in 2015. Scientists suggested that this virus probably might be introduced through the increased foreign visitors to Brazil prompted by the 2014 FIFA World Cup together with the large population of the vectors [13].
In recent times, another Latin America country; Colombia reported the detection of the first autochthonous case again reported in the state of Bolívar [13,54]. Since the above reports in South America, the emergence of the Zika led to a rapid spread throughout South and Central America, it then reach to Mexico in November 2015.
Researchers found a growing evidence of link between Zika infection and microcephaly that pushes CDC to alarm for travellers on January 15, 2016. CDC particularly advising pregnant women to consider in postponing their travel to countries and territories: Brazil, Colombia, El Salvador, French Guiana, Guatemala, Haiti, Honduras, Martinique, Mexico, Panama, Paraguay, Suriname, Venezuela, and the Commonwealth of Puerto Rico. CDC also notify women must consult their physicians before travelling in case if they think to become to be pregnant [54]. Currently Brazil is the most affected country, with preliminary estimates of 440,000 to 1.3 million cases of autochthonous ZIKV infection reported through December 2015 [8]. In the mid of January 2016, there were 363 babies in Brazil born with Zikaa-linked microcephaly, and after a week at January 23, 287 new cases besides the 363 observed according to the Brazilian health officials announcement that raised the case of Zika-linked microcephaly to 4,180 since October 2015 [55].
In North America, the Zika virus detected serologically for the first time in Colorado State. The isolation was made from a traveler returned from West Africa (Southeastern Senegal) after he has seen symptoms of prostatitis and hematospermia in 2008. The person’s wife caught by the Zika infection after she had sexual intercourse with her husband. She has never been gone outside from USA indicating sexual route was one means of Zika virus infection transmission. There is also another suspected case reported from Dallas Health County which still under investigation indicate the potential sexual transmission of Zika virus infection from men to women though no proof or investigation has done about the transmission from women to men person [56]. Although there appeared to see a sporadically increases of infection in travellers originated from infected regions who destined to the United States and Europe yet has not established person to person spread in those areas.
Cases in north America are closely related to travel-related incidents [19]. Similarly, the Public Health Agency of Canada has recently confirmed travel-related cases of Zika virus from Central and South America, and from the Caribbean, the mosquitoes known to transmit the virus to humans are not present in Canada. Latest updates regarding the Zika virus affected countries obtained in the World Health Organization’s Website [57].
Transmission
The most common rout of Zika transmission is through vectorial by mosquitoes of the Culicidae family and of the Aedes genus (sylvatic and urban transmission). The species of genus Aedes include Aedes aegypti (urban transmission). Other species have been reported such as Aedes polynesiensis and Aedes albopictus . Another Aedes hensilli was identified during the Zika epidemic on the island of Yap in 2007, in Micronesia. The virus is mainly transmitted through the bite of Aedes mosquito (hematophagous arthropods during their blood meal) which is fast and easily disseminates. There are other routs of transmission as sexual intercourse [37,44,48,58], blood transfusion [47]. Other routs include the organ transplantation, mother-to-fetusv during the period of the whole pregnancy [14,29]. The vector will acquire the virus during blood sucking period directly and from mother to child through vertical transmission.
Reservoir hosts
Despite the fact, the virus reservoir is not completely identified and isolated; studies suggest at present the reservoir host of Zika virus as primates. On the other hand authors findings indicate the presence of anti-Zika antibodies in various animals including big mammals such as Orang-outang, Zebras, elephants, etc., and rodents in Pakistan [59,60]. These show that, many of the emerging and re-emerging infectious diseases are reserved in the wild and domestic animals [61].
Symptoms
Fortunately, from the total infected individuals only 20 % will develop illness. It is often to see the most common symptoms of Zika such as fever, rash skin, and pain of joint, red eyes, muscle pain, and headache presenting what known as “dengue-like” syndrome when the case developed [5,51,52]. Although the incubation period is not known, it most likely ranges from few days to a week. Developed cases show mild symptoms that last from days to week. People infected with Zika do not get enough sick to go to hospitals, and they are rarely die. Nearly, 60%-80% of infections do not produce any symptoms or signs [62,63].
Diagnosis
The diagnosis of Zika virus needs a close communication between the health care service seeker and the healthcare service provider. The service seeker needs to see the healthcare provider when symptoms of Zika virus seen with the history of visiting areas where Zika is endemic. Any travel information should be informed to the healthcare provider the time and place. Healthcare provider may order specific serological tests for Zika virus immunoglobulins (IgG and IgM) in order to confirm and should be repeated after 2-3 weeks later. The blood test is also similar for Dengu and Chikungunya [64]. It is also possible to diagnosis the Zika virus infection during the first week after onset of symptoms, Zika virus disease can often be diagnosed by performing reverse transcriptase-polymerase chain reaction (RT-PCR) on serum. Virus-specific IgM and neutralizing antibodies typically develop toward the end of the first week of illness; cross-reaction with related flaviviruses (e.g., dengue and yellow fever viruses) is common and may be difficult to discern. Plaque-reduction neutralization testing can be performed to measure virus-specific neutralizing antibodies and discriminate between cross-reacting antibodies in primary flavivirus infections [65].
Controlling strategies
In general, Zika virus is not contagious from person to person; mainly for transmission, the virus requires a mosquito vector to pass the virus to humans. In theoretical view, blood donation and organ transplantation may allow rare person-to-person transmission. Other possible ways may be mother to fetus and under certain conditions, by sexual contact [62].
Self-caring in Zika virus infection
Zika virus has no vaccination currently. If one is infected with the virus, the person may treat the symptoms rather than the disease through drinking enough fluid, by having ample rest, taking those drugs that relief fever and pain, restricting non-steriodial antiinflammatory drugs and consultation of health care professionals in taking other drugs for other sickness [66,67].
Prevention of Zika virus infection
As a prevention strategy, a Zika virus infected person will have a paramount importance in preventing mosquito bite for the first week of the illness, as the virus is available in the blood sometimes even longer period in some people. The blood form of the virus can be easily pass from the infected person to a mosquito that potential spread the virus to other people [66,67]. Strategies for the prevention and control of ZIKV disease should include the use of insect repellent and mosquito vector eradication [68]. Know the following facts will help someone from being infected by the virus and further contribute of viral infection in the area. The virus has no vaccine exists to prevent, hence, the virus has can be prevented from protecting/avoiding mosquito bites (mostly active during day time), avoiding travelling to infested areas, and sexual transmission prevention through using condoms or not having sex are established facts of prevention and controls [67].
Precautions steps pregnant women: A pregnant woman suspected with Zika infection and or a recent travelling history to an infected area should to counsel a public healthcare provider such as doctors or midwife. After testing, if the pregnant women found infected with Zika, a serial ultrasound examination to monitor the fetal growth and anatomy and referral to a maternal-fetal medicine or infectious disease specialist [66].
Concluding remark
Zika is among the present emerging viral diseases of family called flaviviridae and genus flavivirus, that recently took attentions of many nations all over the world due to its current outbreaks and the link to the birth defect “microcephaly” where babies to be borne with small heads and adults with neurological signs. The impact of illness after Zika virus is not a life threating. The Zika infection show often the common symptoms of fever, rash skin, and pain of joint, red eyes, muscle pain, and headache presenting what known as “dengue-like” syndrome. The viruses mainly transmitted from one person to another through the mosquitoes of the genus Aedes that can potentially spread in countries where the vector is present mainly transmit this virus. Concerning the virus reservoir, primates are suggested by different authors, while still ambiguity is present, as it is not clearly identified. Researchers suggest the driving factors for Zika infection includes climatic and weather changes, the presence of vectors, the environmental ecosystems/habitats, travelling history, urbanizations, and others are among the suggested factors. With the recent available diagnostic methods of virological studies and seroprevalence surveys, the virus currently identified in wide geographical locations extending from Africa, to America to Asia, causing sporadic epidemics. The Zika virus diagnosis now is done through serological tests for Zika virus immunoglobulins (IgG and IgM), and should be repeated after 2-3 weeks later in order to confirm. RT-PCR can also help for the first week of infection. Characteristically, the Zika virus is not contagious from person to person. For the virus to transmit, it requires a mosquito vector to pass the virus to humans. In theoretical view, blood donation and organ transplantation may allow rare person-to-person transmission. Other possible ways may be mother to fetus and under certain conditions, by sexual contact. In the prevention of the infection, there is no vaccine yet produced. If one is infected with the virus, the person may treat the symptoms rather than the disease through supporting methods such as drinking enough fluid, having ample rest, taking those drugs that relief fever and pain, restricting from non-steriodial anti-inflammatory drugs and consultation of health care professionals in taking other drugs for other sickness. Special attention should be taken in case of pregnant women and though who have plan to be pregnant. The current review showed that the virus epidemiological distribution is increasing globally with many driving factors. Hence, the following recommendations are forwarded;
1. Regular viral surveillance need to be conducted whenever there is suspecting of viral exposure and presence of vectors and reservoir hosts.
2. Careful and close attention should be taken when there is sign of driving factors occur.
3. All viral transmission routs should be considered closely whenever there prevention and control of the virus dealt.
4. Whenever signs and symptoms of Zika virus observed , immediate contact with health care provider is essential.
5. Regular control of Zika virus vector such as Aedes mosquitoes is essential in order to reduce the population and restrict the reproductive sites.
References
- Biological Sciences Curriculum Study (2012) Emerging and Re-emerging Infectious Diseases. Mark Dabling Boulevard Colorado Springs, CO 80918.
- Becker J, Barry M (2009) Emerging and Reemerging Viral Infectious Diseases. Prepared as part of an education project of the Global Health Education Consortium and collaborating partners. Yale University School of Medicine.
- ATCC Product Sheet Zika virus (ATCC® VR84TM) (2016) Original Source: Blood from experimental forest sentinel rhesus monkey, Uganda, 1947.
- DICK GW (1952) Zika virus. II. Pathogenicity and physical properties. Trans R Soc Trop Med Hyg 46: 521-534.
- Hendrickson WA, Ward KB (1975) Atomic models for the polypeptide backbones of myohemerythrin and hemerythrin. BiochemBiophys Res Commun 66: 1349-1356.
- Pan American Health Organization - World Health Organization - Regional Office for the Americas. Epidemiological Update: Zika virus infection.
- WHO WPR, World Health Organization. Regional Office for the Western Pacific Region. Pacific syndromic surveillance report.
- Rapid risk assessment: Zika virus epidemic in the Americas: potential association with microcephaly and Guillain-Barré syndrome. Stockholm: European Centre for Disease Prevention and Control.
- Dick Gw, Kitchen Sf, HaddowAj(1952) Zika virus. I. Isolations and serological specificity. Trans R Soc Trop Med Hyg 46: 509-520.
- Duffy MR, Chen TH, Hancock WT, Powers AM, Kool JL, et al. (2009) Zika virus outbreak on Yap Island, Federated States of Micronesia. N Engl J Med 360: 2536-2543.
- Lanciotti RS, Kosoy OL, Laven JJ, Velez JO, Lambert AJ, et al. (2008) Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg Infect Dis 14: 1232-1239.
- Grard G, Caron M, Mombo IM, Nkoghe D, Mboui Ondo S, et al. (2014) Zika virus in Gabon (Central Africa)--2007: a new threat from Aedesalbopictus? PLoSNegl Trop Dis 8: e2681.
- http://www.zikavirusnet.com/history-of-zika.html
- https://en.wikipedia.org/wiki/Zika_virus
- Macdonald EM, Koval JJ, Natale R, Regnault T, Campbell MK (2014) Population-based placental weight ratio distributions. Int J Pediatr: 1-7.
- http://ecowatch.com/2016/02/05/climate-change-zika-virus
- http://www.nbcnews.com/storyline/zika-virus-outbreak/could-spread-zika-virus-be-linked-climate-change-n499156
- http://takepart.com./article/2016/01/25/zika
- https://www.washingtonpost.com/news/energy-environment/wp/2016/01/21/how-climate-change-could-help-the-spread-of-zika-virus-and-other-infectious-diseases/
- http://www.washingtonpost.com/sf/national/2015/11/27/disease/
- Alto BW, Juliano SA (2001) Precipitation and temperature effects on populations of Aedesalbopictus (Diptera: Culicidae): implications for range expansion. J Med Entomol 38: 646-656.
- http://takepart.com./article/2015/12/14/warming-planet-will-help-yellow-fever-mosquitoes-thrive
- www.truthdig.com/.../warming_linked_to _spread_of_zika_virus_20160
- http://www.ehp.niehs.nih.gov/1306556/#tabl
- Roth A, Mercier A, Lepers C, Hoy D, Duituturaga S, et al. (2014) Concurrent outbreaks of dengue, chikungunya and Zika virus infections – an unprecedented epidemic wave of mosquito-borne viruses in the Pacific 2012–2014. Euro Surveill 19: 20929.
- http://time.com/4177122/mosquitoes-diseases-zika-virus/
- Althouse BM, Hanley KA, Diallo M, Sall AA, Ba Y, et al. (2015) Impact of Climate and Mosquito Vector Abundance on Sylvatic Arbovirus Circulation Dynamics in Senegal. Am J Trop Med Hyg 92: 88-97.
- Thornton JA, Harrison MJ (1975) Letter: Duration of action of AH8165. Br J Anaesth 47: 1033.
- http://takepart.com./article/2016/01/28/zika/disease
- Mier PD, van den Hurk JJ (1975) Lysosomal hydrolases of the epidermis. I. Glycosidases. Br J Dermatol 93: 1-10.
- www.citylab.com/politics/2016 /02/zika-virus-urbanization.../462366/
- www.theguardian.com/world/2016/feb/11/
- www.cfr.org/public-health-threats-and-pandemics/zika-virus/p37527
- www.who.int/emergencies/zika-virus/articles/mosquito-control/en/
- http://theconversation.com/explainer-where-did-zika-virus-come-from-and-wh
- www.who.int/features/qa/zika/en
- Hayes EB (2009) Zika Virus Outside Africa. Emerging Infectious Diseases 15: 9.
- Robin Y, Mouchet J (1975) Serological and entomological study on yellow fever in Sierra Leone. Bull SocPatholExotFiliales 68: 249-258.
- Jan C, Languillat G, Renaudet J, Robin Y (1978) A serological survey of arboviruses in Gabon. Bull SocPatholExotFiliales 71: 140-146.
- Saluzzo JF, Gonzalez JP, Hervé JP, Georges AJ (1981) Serological survey for the prevalence of certain arboviruses in the human population of the south-east area of Central African Republic (author's transl). Bull SocPatholExotFiliales 74: 490-499.
- Saluzzo JF, Ivanoff B, Languillat G, Georges AJ (1982) Serological survey for arbovirus antibodies in the human and simian populations of the South-East of Gabon (author's transl). Bull SocPatholExotFiliales 75: 262-266.
- Diallo D, Sall AA, Diagne CT, Faye O, Faye O, et al. (2014) Zika virus emergence in mosquitoes in southeastern Senegal, 2011. PLoS One 9: e109442.
- Olson JG, Ksiazek TG, Suhandiman, Triwibowo (1981) Zika virus, a cause of fever in Central Java, Indonesia. Trans R Soc Trop Med Hyg 75: 389-393.
- Tappe D, Rissland J, Gabriel M, Emmerich P, Gunther S, et al. (2014) First case of laboratory-confirmed Zika virus infection imported into Europe, November 2013. Euro Surveill 19.
- Kutsuna S, Kato Y, Takasaki T, Moi M, Kotaki A, et al. (2014) Two cases of Zika fever imported from French Polynesia to Japan, December 2013 to January 2014 [corrected]. Euro Surveill 19.
- Ledermann JP, Guillaumot L, Yug L, Saweyog SC, Tided M, et al. (2014) Aedeshensilli as a potential vector of Chikungunya and Zika viruses. PLoSNegl Trop Dis 8: e3188.
- Musso D, Nhan T, Robin E, Roche C, Bierlaire D, et al. (2014) Potential for Zika virus transmission through blood transfusion demonstrated during an outbreak in French Polynesia, November 2013 to February 2014.Euro Surveill 19.
- Musso D, Roche C, Robin E, Nhan T, Teissier A, et al. (2015) Potential sexual transmission of Zika virus. Emerg Infect Dis 21: 359-361.
- Marcondes CB, Ximenes MF (2015) Zika virus in Brazil and the danger of infestation by Aedes (Stegomyia) mosquitoes. Rev Soc Bras Med Trop 49: 1.
- Pan American Health Organization/World Health Organization (2016) Epidemiological Update: Neurological syndrome, congenital anomalies and Zika virus infection.
- Grard G, Caron M, Mombo IM, Nkoghe D, Mboui Ondo S, et al. (2014) Zika virus in Gabon (Central Africa)-2007: a new threat from Aedesalbopictus? PLoSNegl Trop Dis 8: e2681.
- Direction de la santé Pf (2014) Note d’information à destination des professionnels de santé sur le virus Zika et surl’épidémieencoursenpolynésiefranc¸aise.
- www.aljazeera.com/news/2016/01/zika-virus-cases-spread-latin-america-caribbean
- https://www.minsalud.gov.co/Paginas/Confirmados-primeros-casos-de-virus-del-zika-en-Colombia.aspx
- http://wwww.morningstar.com/news/dow-jones/tdjndn_201601279958/)more-microcephaly-cases-in-brazil.html
- Oster AM, Brooks JT, Stryker JE, Kachur RE, Mead P (2016) Interim Guidelines for Prevention of Sexual Transmission of Zika Virus United States, 2016. Morbidity and Mortality Weekly Report 65: 120-121.
- http://www.phac-aspc.gc.ca/phn-asp/2016/zika-eng.php
- ProMED-mail (2013) ZIKA VIRUS - CANADA ex THAILAND. International Society for Infectious Diseases.
- Darwish MA, Hoogstraal H, Roberts TJ, Ahmed IP, Omar F (1983) A sero-epidemiological survey for certain arboviruses (Togaviridae) in Pakistan. Trans R Soc Trop Med Hyg 77: 442-445.
- Fagbami AH (1979) Zika virus infections in Nigeria: virological and seroepidemiological investigations in Oyo State. J Hyg (Lond) 83: 213-219.
- Wolf ND, Dunavan CP, Diamond J (2007) Origins of Major Human Infectious Diseases. 447: 279-283.
- www.medicinent.com/zika_virus/page3.html
- Cullen KA, Arguin PM (2014)Centers for Disease Control and Prevention (CDC) Malaria surveillance--United States, 2012. MMWR SurveillSumm 63: 1-22.
- CDC (2016) Centers for Disease Control and Prevention National Center for Emerging and Zoonotic Infectious Diseases (NCEZID) Division of Vector-Borne Diseases (DVBD).
- CDC (2016) Diagnostic Testing. Center for Disease Control and Prevention.
- CDC (2016) Center for Disease Control and Prevention.
- CDC (2016) Zika and Pregnancy. Center for Disease Control and Prevention.
- Ioos S, Mallet HP, LeparcGoffart I, Gauthier V, Cardoso T, et al. (2014) Current Zika virus epidemiology and recent epidemics. Infections par le virus Zika et épidémiesrécentes. Médecine et maladies infectieuses 44:302-307.
Relevant Topics
- Advanced Therapies
- Chicken Pox
- Ciprofloxacin
- Colon Infection
- Conjunctivitis
- Herpes Virus
- HIV and AIDS Research
- Human Papilloma Virus
- Infection
- Infection in Blood
- Infections Prevention
- Infectious Diseases in Children
- Influenza
- Liver Diseases
- Respiratory Tract Infections
- T Cell Lymphomatic Virus
- Treatment for Infectious Diseases
- Viral Encephalitis
- Yeast Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 20205
- [From(publication date):
April-2016 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 19173
- PDF downloads : 1032