Epidemiological Aspects and Evolution of Nosocomial Infection in the Neonatology Unit of Angondje Teaching Hospital
Received: 05-Apr-2018 / Accepted Date: 17-Apr-2019 / Published Date: 24-Apr-2019 DOI: 10.4172/2572-4983.1000182
Abstract
Introduction: Hospital-acquired infections in neonatology are a major security problem. We aimed to analyze the evolution of nosocomial infections and their epidemiological aspects in neonatal medicine unit of Angondje Teaching Hospital.
Patients and methods: Retrospective and descriptive study, we included newborns hospitalized for more than 48 h from December 2012 to December 2016.
Results: We admitted 727 newborns in hospital during the study period, 521 have been included, and 134 developed a nosocomial infection, a prevalence of 25.7% of cases. In the end, 103 newborns have constituted our study population. The average age was 33.6 weeks, the sex ratio 1.96. The preterm rate was 79.6 percent. The average weight was 2088.4 g. The reason for hospitalization was prematurity in 46.3%, followed by neonatal infection in 21.1%. Tachycardia associated with hypotonia and apnea, was the main sign of discovery in respectively 56.3% and 39.8%. The average delay between appearance of the signs and hospitalization was 07 days. The average of C-reactive protein was 86.64 mg/dl. Thrombocytopenia was most observed disorder on cell blood count. Escherichia coli was the significant bacteria found the blood culture, urines analysis and culture, lumbar puncture, and umbilical venous catheter culture. Imipenem was the most used antibiotics in the management of nosocomial infection in 44.7% of cases. The mortality rate was 23.3%.
Conclusion: The high rate of nosocomial infection and neonatal mortality urge the implementation of effective methods against this scourge in our neonatology unit.
Keywords: Nosocomial infection; Neonatal; Epidemiology; Antimicrobial resistance; CHUA; Gabon
Introduction
Nosocomial infections (NIs) are a scourge that affect hundreds of millions of people worldwide despite the lower incidence of these infections in developed countries (5 to 10%) [1]. In developing countries, there is little scientific data on this pathology, resulting in a largely underestimated incidence [2]. According to the WHO, the risk of contacting a nosocomial infection is 2 to 20 times higher in these countries than in developed countries with a percentage of affected patients sometimes greater than 25% [1]. In Africa in 2011, the hospitalwide prevalence of these infections ranged from 2.5% to 14.8%, and is highest in services such as the surgical ward with an incidence of 5.7% to 45.8% [3].
In any case, NFIs remain a real public health problem on a global scale, partly because of the mortality, the physical and mental consequences of patients and their families, on the other hand because of the socio-economic cost they generate [4,5]. For WHO, this is a problem still unknown that no health care facility or country can claim to have solved [1].
In neonatal medicine, neonatal nosocomial infections (NNI) are a major safety problem. They are responsible for very high mortality and morbidity, especially in developing countries [6]. The immaturity of the immune system and mucocutaneous barrier, the high rate of digestive translocation, and the invasive procedures necessary for the management (central catheters, intubation probes, vesicals etc.) are the main factors that make the newborn vulnerable in a hospital setting. Similarly, the absence of endogenous flora and the establishment of mucocutaneous flora from the germs of the maternal genital tract, the service environment and those worn by caregivers also constitute a handicap [6]. Epidemiological data on NINTs are not numerous in Africa in general, in Gabon in particular. In any case, they remain underestimated largely because of the difficulties of diagnosis [6].
The purpose of our study was to make an epidemiological analysis of nosocomial infections in the neonatal medicine unit of CHUA, with the secondary objective of identifying the risk factors related to these infections and to evaluate their impact on mortality in our unit.
Patients and Methods
This is a retrospective and descriptive study based on the file carried out in the neonatology unit of CHUA, a level III institution, with a capacity of 9 places.
The study population consisted in newborns admitted in hospital between December 2012 and December 2016. We included in this study all patients admitted to hospital for at least 48 hours with a complete medical record and presenting with a clinical infectious syndrome. secondarily acquired biological, absent at the time of admission or occurring secondarily after an initial infection treated. They must have benefited from an infectious assessment including at least a blood count (NFS), a C Reactive Protein (CRP) and a bacteriological research.
Data collection
Information collected from patient records was collected on a standardized data collection form. The main data evaluated were:
• Anamnestic and anthropometric data,
• Clinical signs at admission and at the time of suspicion of INN,
• The biological assessment carried out at the time of the suspicion of INN,
• The duration of the umbilical vein catheter.
• ATB treatment at admission and at the time of suspicion of INN,
• The evolution.
Data analysis
The data were analyzed with the Microsoft ACCESS software. Tables were made on the Microsoft Word software.
Results
During the study period, 727 newborns were admitted to hospital. Among them, 206 had less than 48 hours in hospital, 521 were included and 134 of them developed a nosocomial infection, a prevalence of 25.7%. The study population consisted of 103 newborns due to the exclusion of 31 (23.1%) unexploitable records.
General characteristics of the sample
• The study population consisted of 68 (66%) boys and 35 (34%) girls, a sex ratio of 1.96.
• The average age was 33.6 SA with extremes ranging from 26 SA+4 days to 42 SA+3 days. The rate of premature newborns (less than 37 weeks) was 79.6% (n=82). Of these, 54.9% (n=45) had less than 33 weeks.
• The average weight was 2088.4 g with extremes ranging from 800 to 6690 g. Newborns with less than 2500 g accounted for 73.7% (n=76), of which 44.7% (n=34) had less than 1500 g.
• The time between birth and hospitalization was less than 24 hours in 72.8% of newborns (n=75). More than half (70.6%, n=53) came from our maternity ward.
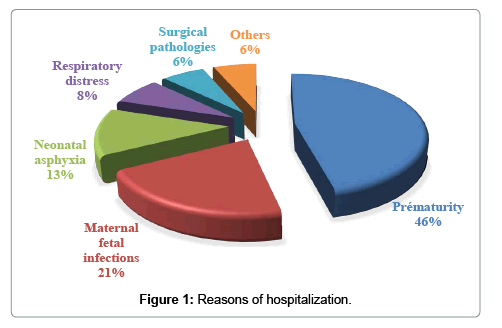
• The reason for hospitalization was mainly prematurity in 46.3%, followed by neonatal infection in 21.1% and neonatal asphyxia in 12.6% (Figure 1).
• The umbilical vein catheter was placed in 80.6% (n=83) of neonates, with an average duration of 6 days and extremes ranging from 3 to 12 days. Of these, 38.5% (n=32) had an umbilical vein catheter lifetime greater than 5 days.
Nosocomial infection
Signs of discovery: The temperature was normal in 62.2% of cases. Tachycardia was the most observed sign of discovery. It was associated with hypotonia and apnea in 56.3% and 39.8% respectively (Table 1).
| Signs | n | (%) | |
|---|---|---|---|
| Hemodynamic | Tachycardia | 29 | #### |
| Bradycardia | 10 | -9.70% | |
| Heart failure | 2 | -1.90% | |
| Respiratory | Apnea | 20 | #### |
| desaturation | 11 | #### | |
| Neurologic | Hypotonia | 10 | -9.70% |
| Convulsions | 4 | -3.90% | |
| Metabolic | Hypothermia | 20 | #### |
| Hyperthermia | 16 | #### | |
| Icterus | 5 | -4.80% | |
| Signs associations | Tachycardia+Hypotonia | 58 | #### |
| Tachycardia+apnea | 41 | #### | |
| Bradycardia+apnées+desaturation | 38 | #### | |
| Hypotonie+desaturation | 29 | #### | |
| Hypothermie+apnea+desaturation | 26 | #### | |
| Bradycardia+apnea+hypothermia | 22 | #### | |
| Icterus+tachycardia | 19 | #### | |
| Apnea+desaturation | 16 | #### | |
| Tachycardia+hypotonia | 11 | #### | |
| Abdominal distension+↑ résidus gastriques | 6 | -5.80% | |
| Convulsions+hyperthermia | 5 | -4.80% | |
| Tachycardia+hypotonia+abdominal distension | 4 | -3.90% | |
| Apnea+Bradycardia+liquid stools | 3 | -3% | |
Table 1: Signs of discovery.
The time of appearance of the signs: The average time to onset of nosocomial infection versus hospitalization was 07 days with extremes of 4 days to 19 days.
Biology report
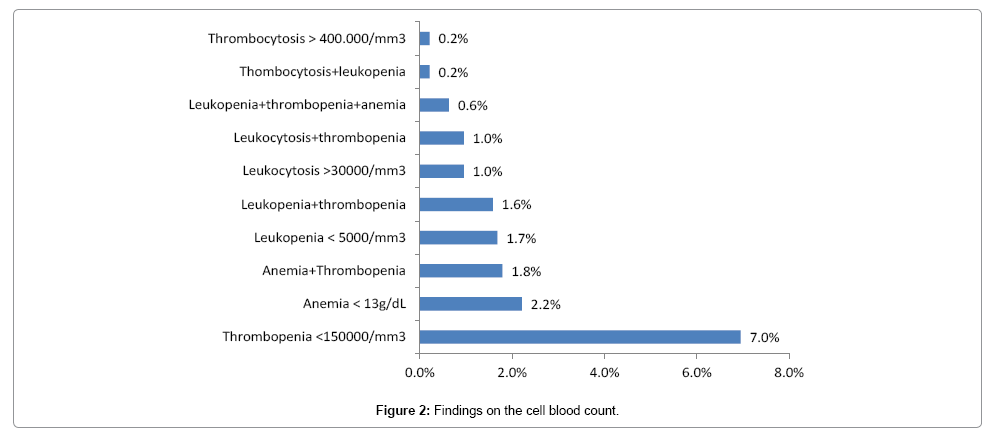
1. The Cell Blood Count (CBC): Thrombocytopenia was the most recovered parameter in the NFS with a rate of 69.5% (Figure 2).
2. The CRP: CRP was positive in all patients, with an average of 86.64 mg/dL and extremes ranging from 24 to 471.25 mg/L. Of these, 27.2% (n=28) had a CRP greater than or equal to 90 mg/dl.
Bacteriology
Blood culture: The blood culture was performed in 68.9% (n=71), it was positive in 60.5% (n=43) of newborns. Escherichia coli (E. coli) was the most recovered organism with 24% of cases, including 3 broadspectrum beta-lactamase E. coli (BSBL). In the Staphylococcus aureus group, 2 were resistant to methicillin (MRSA) (Table 2).
| Bacteria(s) | n | (%) |
|---|---|---|
| E. coli (+3 E. coli BLPE) | 9 | (24) |
| Klebsiella oxytoca | 7 | (18.7) |
| Klebsiella pneumoniae | 5 | (12) |
| Staphylococcus epidermidis | 5 | (12) |
| Enterobacter cloacae | 5 | (9.3) |
| Staphylococcus aureus (+2 MRSA) | 4 | (8) |
| Candida albicans | 2 | (4) |
| Pseudomonas aeruginosa | 2 | (6.7) |
| Staphylococcus epidermidis + Candida albicans | 2 | (2.7) |
| Serratia marcescens | 1 | (1.3) |
| Total | 43 | (100) |
Table 2: Principal bacteria(s) found on blood culture.
Lumbar puncture: PL was performed in 19 (18.5%) neonates. In 31.6% (n=6), cerebrospinal fluid (CSF) culture was positive. The germs observed were E. coli (3) including 1 BSBL, MRSA (1), Klebsiella oxytoca (1) and Enterobacter cloacae (1). Among these 6 positive CSFs, the identified germ was identical to that found in 2 hatchlings in blood cultures (E. coli ESBL).
Cytobacteriological examination of urine (CBEU): CBEU was performed in 11 (10.7%) neonates. In 36.4% (n=4), the culture was positive. The germs observed were E. coli (2) including 1 BSBL, Enterobacter cloacae (1) and Serratia marcescens (1). Among these 4 positive CBEU, the identified germ was identical to that found in 3 newborns, including 2 in the blood culture (E. coli BSBL) and 1 in the culture of CSF (Enterobacter cloacae). Serratia marcescens was the same found in blood culture.
Culture of umbilical vein catheter (UVC): The culture of UVC was carried out in 63 (61.2%) neonates, of whom 12 (19%) were positive, of which 5 had a duration greater than 5 days. The germs found were E. coli (3) including 1 ESBL, Staphylococcus aureus (3) including 1 MRSA, Enterobacter cloacae (2), Klebsiella oxytoca (1), C. albicans (2) and C. albicans associated with Klebsiella oxytoca (1). Of these, blood culture, lumbar puncture and ECBU were positive in 2 to E. coli ESBL and 1 in Enterobacter cloacae.
Treatment and Evolution in Hospital
At admission, 93.2% (n=96) of patients received a triple probiotic antibiotic therapy containing Cefotaxime, amoxicillin (or ampicillin) and gentamicin. This antibiotic was stopped after 72 hours in 62.5% (n=60) of cases.
The different antibiotics used at the time of suspicion of NI
At the time of suspicion of nosocomial infection: Imipenem was used in 44.7% (n=46) of cases at the dose of 100 mg/kg/day in 4 doses, Meropenem in 13.6% (n=14) of cases at the dose of 60 mg/kg/day in 3 doses. Vancomycin in combination with gentamycin in 20.4% (n=21) of cases, Imipenem in combination with vancomycin in 16.5% (n=17) of cases, Imipenem in combination with Gentamycin in 21.3% (n=22) of cases, Meropenem in combination with vancomycin in 8.7% (n=9).
After the antibiogram: 3rd generation cephalosporin (3GC), amoxicillin (or ampicillin) were ineffective on all the organisms observed, gentamycin was ineffective in 11.8% of cases. The sensitive molecules present on our territory were Amikacin, Imipenem, Meropenem, Ofloxacin, Ciprofloxacin.
Germs resistant to all second-line antibiotics available on the territory with the exception of quinolones were observed in 15 newborns. Thus, ofloxacin was used in 8.7% (n=9) of cases at a dose of 20 mg/kg/day in 2 doses and ciprofloxacin in 5.8% (n=6) of cases at dose. 20 mg/kg/day in 2 doses. Fluconazole (Triflucan®) in slow IV was used in 7.8% (n=8) of cases at 6 mg/kg once daily.
Evolution in hospital
The mean hospital stay was 20.3 days with extremes ranging from 10 to 45 days. The mortality rate was 23.3% (n=24) and the survival rate was 76.7% (n=79). The characteristics of dead infants are summarized in Table 3.
| Parameters | n and (%) | ||
|---|---|---|---|
| Sex | Boys | 15 (62.5%) | |
| Girls | 9 (37.5%) | ||
| Mean gestationnal age | 30 weeks (extremes 24-39 weeks) | ||
| Mean weight | 1670g (extremes 800-3520 g) | ||
| Most frequent cause of hospitalization | Prématurity 18 (75%) | ||
| Mean CRP | 43.4 mg/l (extremes 36-324 mg) | ||
| Localisation | Septicemia | 18 (75%) | |
| Septicémia+Meningeal | 4 (16.7%) | ||
| Urinary | 2 (8.3%) | ||
| Duration of UVC > 5 jours | 8 (33.3%) | ||
| Responsible germs | Klebsiella oxytoca | 5 (20.8%) | |
| E. Coli | 4 (16.7%) 2 *BLPE | ||
| Pseudomonas aeruginosa | 2 (8.3%) | ||
| C. albicans | 2 (8.3%) | ||
| Serratia marcescens | 1 (4.2%) | ||
| Staphylococcus aureus | 1 (4.2%) *MRSA | ||
| Not found | 9 (37.5%) | ||
Table 3: Characteristics of dead newborns.
Discussion
Our objective was to determine the epidemiological factors of nosocomial infection within the neonatology unit of CHUA. The exclusion of nearly 23.1% of the eligible cases due to incomplete information, was the main limitation of this study. It can be explained by the retrospective design of the study which does not provide information all the inclusion criteria. But this fact does not affect the substantive of the results obtained.
Prevalence
Nosocomial infection (NID) is defined as an infection acquired in a health care facility that was neither incubated nor present at the time of admission. The delay between admission and the start of infection should be 48-72 hours for bacterial infections and depending on the incubation period it may be longer in viral infections [7]. A diagnostic problem arises in neonatal medicine generally. Indeed, it is difficult to differentiate between an early-occurring NIN and a late-onset maternal-fetal infection [6,8]. This difficulty creates a significant bias on the epidemiological data of this condition in the neonatal period and thus makes them unreliable. This may have prompted some authors to arbitrarily define as NUI, “all infections acquired during labor and during hospitalization, unless transplacental passage can be proved, or implicitly attributed to this type of transfer, in this case toxoplasmosis or congenital cytomegalovirus infection” [9]. It has already been shown that early neonatal infections with Streptococcus and Escherichia coli, recognized as maternal-fetal infection, can be true nosocomial infections after horizontal transmission. Thus, the moment of acquisition of INN is difficult to identify, it can be intrapartum, per-partum or immediate postpartum [8,10] and is therefore not an absolute criterion in its definition. The fact that about 3% of neonates in the maternity hospital present a nosocomial infection is a good illustration of this difficulty [7,9,11].
Other parameters still related to the diagnostic problem also make NIE data unreliable, such as the differences observed according to the type of country, the type of establishment or even between series of the same country [4]. These discrepancies justify the fact that the rate of NINT varies according to continents, countries, care units and their recruitment, prescribing habits, use of invasive procedures and the characteristics of newborns. born [7].
In our department, the prevalence of this pathology is very high, i.e. 25.7%. This figure is in line with the rates observed in developing countries where the incidence in neonatology units is around 34-52% or even 73% [11,12]. At the University Hospital of Yopougon Abidjan, the prevalence of germs usually implicated in nosocomial infections was 33% [13]. In France, as in most developed countries, it varies between 7 and 24.5% depending on the type of service [7,14]. In the Maghreb countries, the hospital incidence of NINTs is closer to those observed in France. It was 7.5% at CHU Ibn Rochd in Casablanca in 2013 [15], 13% in Marrakech in 2014 and 3.48% in western Algeria in 2015 [5].
This very high incidence of NNIs in neonatal units is a real security problem despite the progress made in terms of surveillance and prophylactic measures even in developed countries. According to Stoll, these measures taken to reduce the rate of nosocomial infections in general have no impact on perinatal nosocomial infections because of the difficulties of authentication of the INN [10].
The high rate of NNI in developing countries can find a explanation in the usual insufficiency of diagnostic supports, qualified personnel and poor working conditions (materials, medicines), in a context or the proportion of premature newborns is highest and health systems do not pay sufficient attention to this segment of the population [14]. In the neonatal medicine unit of our hospital, non-compliance with hygiene regulations is observed during the performance of medical procedures. There is sometimes a lack of running water for hand washing, in a context of overcrowding with too many newborns and insufficient medical and para-medical staff, the majority of whom are not qualified (1 nurse for 5 to 8 newborns). It is coupled to this, an insufficient use of the hydroalcoholic solution which is distributed almost sporadically in the best case. Despite the multiplicity of staff training in hospital hygiene, these shortcomings do not prevent the appearance of NNI. Another factor is the financial difficulties of the structure that hinder the implementation of quality hospital hygiene by limiting the means of control and surveillance of nosocomial infections.
Diagnosis of NNIs
In neonates, there is no specific sign of neonatal infection. But most often, the nosocomial infection is suspected in front of a alteration of a previously stable clinical condition, especially in the circulatory and respiratory areas. Abdominal meteorism, increase of gastric residues, an increase of glycaemia can also be prodromal.
In biological parameters, leukopenia less than 5000/mm3 or hyperleukocytosis greater than 25000/mm3, thrombocytopenia at 100000/mm3 and elevation of inflammation proteins (PCT or CRP) were suggestive of NNI [16]. These fact corroborate with the findings in our study. Hemodynamic and respiratory signs were the most observed clinical signs, as well as thrombocytopenia. A positive blood culture associated with clinical and biological changes constitute the elements of the diagnosis of certainty [6]. It is well established that the rate of documentation of bacteraemia in neonatalogy is low, most often of the order of 45% in the developed countries [17]. One of the reasons is the insufficient blood volume to inject in the blood culture flasks (1 ml) [6]. As a result, even though some authors require bacteriological documentation of infections, most surveillance networks adopt definitions that are simply based on clinical and biological criteria [5].
In developing countries in general, Gabon in particular, it is rather the insufficient and often defective technical platform that makes it difficult to isolate the germs. In our study, the search for germs is quite insufficient, because the blood culture was carried out in only 68.9%, the CBEU in 10.7% and the culture of UVO in 61.2%. This low rate of identification of germs is justified by the frequent lack of materials in the laboratory (blood culture flasks, culture media, etc.). Most often, this search for germs is largely after the administration of antibiotic because the rapid evolution of sepsis requires a rapid start and without delay of antibiotic therapy. We can therefore find here the justification for the high number of negative results in our study.
The infection site was in the majority of cases blood (septicemia) and accounts for 45 to 55% of severe NNI, followed by pulmonary involvement which usually complicates an invasive ventilation [7,8]. In our study, sepsis was observed in 60.5% of cases. It was also predominantly observed in 31.4% of cases at Ibn Rochd UHC in Casablanca [15], 89% in Marrakech and in 76% of cases in Tlemcen, Algeria [5,16].
In developing countries, the most observed group of organisms is the group of Gram-negative bacilli (BGN) [6]. In our study it is also this group that is the most observed, dominated by E. coli, some of which were producers of broad-spectrum beta-lactamases in the blood, cerebrospinal fluid, urine or umbilical vein catheter. This observation is also made at Yopougon University Hospital in Abidjan, Casablanca, Marrakech [16]. In Madagascar, it is rather the Grampositive Cocci, followed by BGN, the great majority (95%) of which are ESBL-producing [11,13,15,16]. In developed countries, it is the Gram-positive Cocci that are in the lead and dominated by coagulasenegative staphylococcus, more than 80% of which are resistant to methicillin, followed by gram-negative bacilli [6,8,18]. The lack of hygiene observed during and after childbirth in developing countries favors the colonization of newborns by BGNs and is at the origin of this microbiological difference [6]. In addition, authors described that GNB in NNIs generally occur in individuals already colonized by their own germs [19]. Although staphylococci and gram-negative bacilli are the most frequently encountered germs, yeast pressure is clearly increasing, with C. albicans accounting for nearly 9% to 12.8% of neonatal septicemia of nosocomial origin. and affects nearly 80% of newborns under 1000 g [6-8]. In the United States, 50% of neonates hospitalized in neonatal resuscitation are colonized with C. albicans at the end of the first week of hospitalization, with a direct relationship between the extent of colonization and the risk of invasive infection. incidence reaches 20% in less than 1000 g [20]. In our study this germ is present in about 7% of cases. This rate is very probably biased, because the limits of our laboratories do not allow the detection of this microbe and increase the false negative rate of the microbial cultures.
Risk factors
The literature states that the risk factors for the occurrence NNI are prematurity, low birth weight, the presence of an invasive device (central catheters, bladder catheter, intubation probe, etc.) and the duration of hospitalization [5,14,15]. Artificial feeding, parenteral, hospital environment, drugs such as antibiotics or corticosteroids are also cited [8]. These different factors justify the high prevalence of NNI in our study because the rate of premature newborns was 79.6% with an average age of 33.6 weeks, of which 54.9% were less than 33, almost all received broad-spectrum antibiotic therapy at admission [21]. The umbilical venous catheter was placed in 80.6% with a mean duration of stay of 6 days, and in nearly 40% of cases a duration greater than 5 days. However, it is known that the infection rate of the catheter is proportional to its duration [6,22,23].
Evolution of newborns with nosocomial infection
In developed countries, the overall mortality rate linked to INN varies from 2 to 16%. In France, it is around 10% and varies according to the germ. It is 10 to 19% for Gram-positive cocci, 28% for mushrooms and 40% for BGNs [6,7,24]. In general, the mortality rate for NINTs is higher in developing countries. Mortality in our study was very high at 23.3% and was most common in preterm infants, low birth weight, umbilical catheter carrier, BGN and C. albicans sepsis. Our hospital mortality rate is similar to that of Ibn Rochd Hospital in Casablanca, which was 28.5% [15]. In Marrakech, it is higher at 52.7% [16].
NNIs increase the risk of neurological sequelae in terms of neurodevelopmental impairments in neonates in general and preterm infants in particular [6,24]. Unfortunately, given the retrospective nature of our study, we have not been able to assess the long-term future of our patients.
Conclusion
NNIs are a serious health issue in Africa in general and in CHUA in particular because of its very high prevalence and mortality rate. Paradoxically, it is a problem still “unknown” in most of our regions. The risk factors for the occurrence of these infections are identified and the establishment of preventive methods in our structure is one of the most effective ways to fight against this scourge. Thus, the respect of hospital hygiene rules, a good use of antibiotics, the establishment of an epidemiological surveillance of nosocomial infections, are the essential points to significantly reduce the incidence of nosocomial infections.
References
- Fortes Deguenonvo L, Traore K, Dia Babiane NM, Cissoko Y (2005) Resultats d’une enquête d’incidence des cas d’infections nosocomiales a bacteries multi resistants dans un centre hospitalier a Dakar (Senegal). Revue Malienne d’Infectiologie et de Microbiologie 5: 8-25.
- Bagheri Nejad S, Allegranzi B, Syed BS, Ellis B, Pittet D (2011) Health care-related infections in Africa: a systematic study. Bull World Health Organ 89: 757-765.
- Fki H, Yaich S, Jdidi J, Karray A, Kassis M (2008) Epidemiology of nosocomial infections in Sfax university hospitals: Results of the first National Survey of Prevalence of Nosocomial Infection. Rev Tun Infectiol 2: 22-31.
- Chabni N, Regagba D, Meguenni K, Ghomari SM, Smahi MC (2015) Risk factors for nosocomial infection at the multipurpose neonatology service of the mother-child specialized hospital in Tlemcen, western Algeria, "case-control study". Journal de pediatrie et de puericulture 28: 71-79.
- Doit C, Biran V, Aujard Y (2015) infection nosocomiale en neonatologie. in: infections neonatales. Paris: Elsevier Masson 91-106.
- Lachassinne E, Letamendia-Richard E, Gaudelus J (2004) Epidemiologie des infections nosocomiales en neonatalogie. Arch Pediatr 11: 229-233.
- Dachy A, Battisti O (2014) How I explore nosocomial infections in neonatology Rev Med Liege 69: 454-459.
- Baltimore RS (1998) Neonatal nosocomial infections. Semin Perinatol 22: 25-32.
- Stoll BJ, Hansen NI, Higgins RD (2005) Very low birth weight preterm infants with early onset neonatal sepsis: the predominance of gram-negative infections continues in the National Institute of Child Health and Human Development Neonatal Research Network . Dis J Pediatr Infect 24:635-639.
- Andrianarivelo AM, Rafaravavy NE, Rafalimanana C, Andriantahiana TN, Robinson AL (2010) Bacteriological profile of neonatal infections in the Neonatal Resuscitation Unit of Befelatanana Maternity.Revue d’Anesthesie-Reanimation et de Medecine d’Urgence 2: 1-4.
- Zaidi AKM (2005) Hospital acquired neonatal infections in developing countries. Lancet 365:1175-1188.
- Lasme-Guillao E, Amon-Tanoh-Dick F, GBonon V, Adja Akaffou E, Kabas R, et al. (2011) Infections with Klebsiella pneumonia and Enterobacter cloacae in neonatology in Abidjan. Journal de Pediatrie et de Puericulture 24: 118-124.
- Aujard Y, Bottineau MC (2015) Epidemiologie mondiale des infections neonatales. Dans: infections neonatales. Paris: Elsevier Masson 11-18.
- Chemsi M, Chahid I, Lehlimi M, Aalloula O, Zerouali K (2013) Incidence of nosocomial bacterial infections. Abderrahim Harouchi Children's Hospital, Ibn Rochd UHC, Casablanca, Morocco. Journal de Pediatrie et de Puericulture 26: 11-18.
- Maoulainine FMR, Elidrissi NS, Chkil G, Abba F, Soraa N, et al. (2014) Epidemiology of nosocomial bacterial infection in a Moroccan neonatal resuscitation service. Archi Pediatr 21: 938-943.
- Geffers C, Baerwolff S, Schwab F, Gastmeier P (2008) Incidence of healthcare-associated infections in high-risk neonates: results from the German surveillance system for very-low-birth weight infants. J Hosp Infect 68: 214-221.
- Campeotto F, Garnier F, Kalach N, Soulaines P, Dupont C, et al. (2004) Nosocomial acquisition of multi-resistant bacteria in a neonatal department: prospective study and analysis of risk factors.Arch Pediatr 11: 1314-1318.
- Guediche MN (1990) Bacterial colonization of the newborn and infection Medecine du Maghreb 22: 25-27.
- Brissaud O, Tandonnet O, Guichoux J (2011) Invasive candidiasis in neonatal resuscitation.Arch Pediatr 18: 22-32.
- Cottineau MC (2015) Infection neonatales dans les pays en voie de developpement. Dans: infections neonatales. Paris: Elsevier Masson 204-223.
- Oulmaati A, Hmami F, Bouharrou A (2013) The contribution of quinolones in neonatology (about 21 cases). Journal de Pediatrie et de Puericulture 26: 193-197.
- Nejjari N, Benomar S, Lahbabi MS (2000) Nosocomial infections in neonatal and pediatric resuscitation. Interest of ciprofloxacin. Arch Pediatr 7:1268-1273.
- Ericson JE, Benjamin DK (2004) Fluconazole prophylaxis for prevention of invasive candidiasis in infants. Curr Opin Pediatr 26: 151-156.
Citation: Kuissi KE, Minto’o RS, Mimbila M, Medza ER, Koumba MR, et al. (2019) Epidemiological Aspects and Evolution of Nosocomial Infection in the Neonatology Unit of Angondje Teaching Hospital. Neonat Pediatr Med 5: 182. DOI: 10.4172/2572-4983.1000182
Copyright: © 2019 Kuissi KE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5288
- [From(publication date): 0-2018 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 4480
- PDF downloads: 808