Epidemic Poisoning with Snakes in Eastern Sri Lanka; Epidemiological and Clinical Features in Batticaloa District
Received: 09-Jan-2015 / Accepted Date: 18-Feb-2015 / Published Date: 22-Feb-2015 DOI: 10.4172/2161-1165.1000183
Abstract
Keywords: Snake bite; Batticaloa; Epidermiology
162927Introduction
Snake bite is an important cause of mortality and morbidity in certain parts of Sri Lanka. Snakebite is an important health problem in Sri Lanka, particularly in rural and farming areas. In 1999, there were 32,303 cases of snakebite with a case fatality rate of 0.6% [1]. In the country, approximately 95% of the mortality is attributable to bites by the cobra (Naja naja), Russell’s viper (Daboia russelii), common krait (Bungarus caeruleus), and Sri Lankan krait [2]. The principal effects of envenomation with snake toxins are related to neurotoxicity, nephrotoxocity, myotoxicity, cardiotoxicity, coagulopathy, vascular endothelial damage and local reactions.
An accurate measure of the global burden of snakebite envenoming remains elusive despite several attempts to estimate it and, apart from a few countries, reliable figures on incidence, morbidity, and mortality are scarce. South Asia is by far the most affected region. India has the highest number of deaths due to snake bites in the world with 35,000-50,000 people dying per year according to World Health Organization (WHO) direst estimates [3]. In Sri Lanka, around 33,000 envenomed snake bite victims are reported annually from government hospitals [3].
Snake bite is an important occupational injury affecting farmers, plantation workers, herders, and fishermen [4,5]. Open-style habitation and the practice of sleeping on the floor also expose people to bites from nocturnal snakes. Bites are more frequent in young men, and generally occur on lower limbs [6]. The incidence of snake bites is higher during the rainy season and during periods of intense agricultural activity [3]. Snake bite incidence and mortality also increase sharply during extreme weather events such as floods [6].
The aim of this study was to evaluate the epidemiological features, clinical manifestations, biochemical findings and outcome of management using currently available treatment, in the Batticaloa district in Eastern Sri Lanka.
Materials and Methods
Study Population
104 patients [Mean age: 30-32(±0.43) yrs.], (Male: Female=81:23) with snake bites admitted to a Poisoning Unit, Tertiary Care Hospital in Eastern Sri Lanka with one year period were included using predesigned questionnaires, retrospectively.
Electrocardiographic Monitoring
12-lead standard electrocardiography (INNOMED Medical ECG machine) and 2-lead ECG monitoring were taken during the standard work up of each patient in this unit.
Blood Samples
Five millilitres (5 ml) venous blood was collected from each patient. Serum was separated by centrifuging in a laboratory centrifuge at for three (3) minutes after blood clotting and retraction at room temperature. Serum potassium (K+) and Sodium (Na+) were analysed at the Department of Chemical Laboratory. Renal function including blood urea nitrogen [BUN], creatinine and liver function indices including SGOT, SGPT, PT and serum protein were analysed in the clinical laboratory of Batticaloa Teaching Hospital using standard automated techniques.
Ethical clearance
Ethical clearance was obtained from Ethical Review Committee, Faculty of Health Care Sciences, Eastern University of Sri Lanka.
Statistical Analysis
Differences between the two groups [patients with significant systemic envenomation vs patients without systemic envenomation were analysed with pair-wise comparisons. Baseline results are presented as counts and percentages and as mean ± SD for continuous variables. A P value < 0.05 was considered significant.
Results
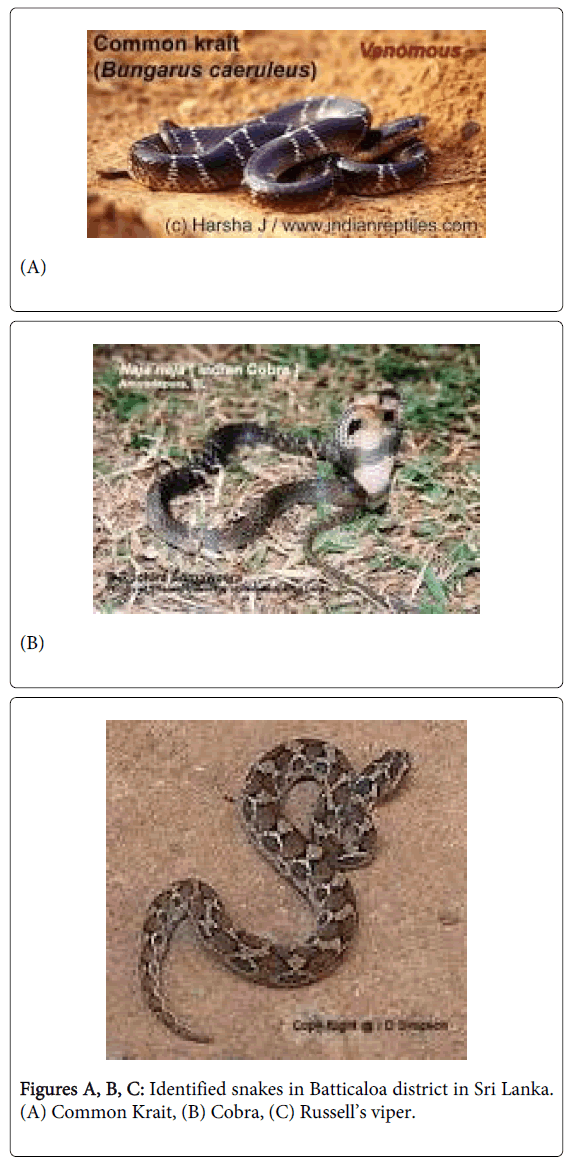
Common krait (42, 40.1%), Cobra (18, 17.3%) and Russell’s viper (25, 24%) and Saw scald viper (5, 4.8%) were identified snakes (Figure 1). 19 cases were unidentified. Krait bites were observed anywhere from head to toes of victims sleeping on the floor (30, 71.5%) mainly at night related to rainy seasons; high incidence (68.5%) reported in November and December. Cobra bites were below elbow and knee of victims (12, 77.8%) near water reservoirs and inside dwellings. Russell’s viper bites occurred below elbow and knee of victims (20, 80%) working in paddy fields (19, 76%). Fingers, hand, ankle and foot were main sites of Saw scald viper bite.
Neurotoxicity (ptosis, external opthalmoplegia, respiratory paralysis, limb paralysis) was the cardinal feature of krait bite (35, 83.3%) (Table 1). Local effects and coagulopathy were not observed. Local swelling/tissue necrosis (12, 66.7%) and neurotoxicity (ptosis, external opthalmoplegia, respiratory paralysis, limb paralysis) (15, 83.3%) were main clinical manifestation of cobra bite (Table 1). Localized swelling (12, 48%), neurotoxicity (ptosis, external opthalmoplegia, respiratory paralysis, limb paralysis) (18, 72%) and coagulopathy (spontaneous bleeding such as haematuria, GIT bleeding, mucosal bleeding, prolonged clotting time, in coagulate blood) (22, 88%) were main clinical features of Russell’s viper (Table 1).
| Types of Snakes | Clinical Manifestations | Number of Cases | |
|---|---|---|---|
| Krait | Local effects | Localised swelling/necrosis | Nil |
| Neurological effects | Ptosis | 35 | |
| External opthalmoplegia | 24 | ||
| Respiratory paralysis | 18 | ||
| Coagulopathy | Mucosal bleeding | Nil | |
| Disseminated Intravascular Coagulation | Nil | ||
| Russell’s viper | Local effects | Localized swelling | 12 |
| Localized necrosis | 2 | ||
| Neurological effects | Ptosis | 18 | |
| External pthalmoplegia | 12 | ||
| Respiratory paralysis | 6 | ||
| Coagulopathy | Mucosal bleeding | 25 | |
| Disseminated Intravascular Coagulation | 8 | ||
| Cobra | Local effects | Localized swelling | 12 |
| Localized necrosis | 2 | ||
| Neurological effects | Ptosis | 15 | |
| External pthalmoplegia | 7 | ||
| Respiratory paralysis | 3 | ||
| Coagulopathy | Mucosal bledding | Nil | |
| Disseminated Intravascular Coagulation | Nil |
Table 1: Clinical manifestations of identified snakes in Batticaloa District.
All patients with systemic envenomation were managed with Anti Snake Venom (ASV) available in Sri Lanka which is a polyvalent equine serum manufactured by Indian companies. 10-20 vials of ASV were sufficient to manage the Krait and cobra bites. In viper bites, ASV was repeated in 6 hours in dose of 10 vials if coagulopathy persisted; the end point of ASV therapy was reversal of coagulopathy as determined by serial performance of the 20 WBCT.
Acute respiratory failure (18, 51%) was the main hazard in krait bite. Sever localized necrosis (2, 11.1%) and respiratory failure (3, 16.6%) were lethal complications in cobra bites. Acute renal failure (15, 60%) and Disseminated Intravascular Coagulation (8, 33.6%) were main complications in viper bites. Blood and other investigations were shown in Table 2.
| Biochemical markers | Parameters | Values/Findings | Number of Cases |
|---|---|---|---|
| Renal markers | Serum Electrolytes (K+) | 5.5-6.9 mEq/dL | 10 |
| >7 mEq/dL | 5 | ||
| Blood Urea | 30-70 mg/dL | 5 | |
| 70-100 mg/dL | 5 | ||
| >100 mg/dL | 12 | ||
| Serum creatinine | 1.5 -2.5 mg/dL | 2 | |
| 2.6-4.0 mg/dL | 5 | ||
| >4 mg/dL | 12 | ||
| Liver markers | SGPT/SGOT | <100 IU/L | 12 |
| >100 IU/L | 14 | ||
| PT/INR | 1.5- 2.5 | 5 | |
| >2.0 | 8 | ||
| Others | UFR | Haematuria | 28 |
| Proteinuria | 4 | ||
| ECG | Ischaemic changes | 5 | |
| Echocardiography | Myocarditis | 7 | |
| Impaired LV function | 5 |
Table 2: Biochemical and other findings of snake bite victims in Batticaloa District.
Acute respiratory failure needed ventilator care in intensive care units. Acute renal failure was managed with dialysis. DIC was managed with blood products. Local effects were managed with oral /intravenous cloxacillin.
Mortality rate was 3.8%. Severe systemic envenomation was significantly associated with mortality and morbidity of victims (P<0.05).
Discussion
Common krait (42, 40.1%), Cobra (18, 17.3%) and Russell’s viper (25, 24%) and Saw scald viper (5, 4.8%) were identified snakes in Batticaloa district of Eastern part of Sri Lanka. In other parts of Sri Lanka, these are identified snakes [2]. In Sri Lanka, around 33,000 envenomed snake bite victims are reported annually from government hospitals [3]. In Eastern Province of Sri Lanka, 104 envenomed snake bite victims are reported annually from Batticaloa district.
Snake bite is an important occupational injury affecting farmers, plantation workers, herders, and fishermen. Open-style habitation and the practice of sleeping on the floor also expose people to bites from nocturnal snakes. The incidence of snake bites is higher during the rainy season and during periods of intense agricultural activity [4]. Krait bites were observed among victims sleeping on the floor (30, 71.5%) mainly at night related to rainy seasons; high incidence (68.5%) reported in November and December.
In Sri Lanka, occupation has a direct relationship to snakebite [5]. The occupation of 45% of the population is agriculture, animal husbandry, forestry, fishing and hunting. In Sri Lanka, 85% of the circumstances in which snakebite took place were while they engaged directly or indirectly in agricultural activities or related pursuits such as weeding, preparation of fields, harvesting, guarding fields etc. [5]. Cobra bites were occurred near water reservoirs and inside dwellings. Russell’s viper bite occurs while working in paddy fields (19, 76%).
Bites are more frequent in young men, and generally occur on lower limbs [6]. Krait bites were observed anywhere from head to toes of victims. Cobra bites were below elbow and knee of victims (12, 77.8%). Russell’s viper bites occurred below elbow and knee of victims (20, 80%). Fingers, hand, ankle and foot were main sites of Saw scald viper bite. Young adults aged 20-40 years were the victims of snake bites in Batticaloa district (57, 54.5%).
A widespread belief is that snake bites inevitably result in envenoming. However, bites by nonvenomous snakes are common and bites by venomous species are not always accompanied by the injection of venom (dry bites). A large survey conducted in ten hospitals of southern Nepal revealed that envenoming occurred in only 10% of the victims [7].
When envenoming does occur, it can be rapidly life-threatening. Snake venom is a complex mixture of toxins and enzymes, each of which may be responsible for one or more distinct toxic actions. The principal effects of envenomation with snake toxins are related to neurotoxicity, nephrotoxocity, myotoxicity, cardiotoxicity, coagulopathy, vascular endothelial damage and local reactions. Muscle weakness following snake bite has been reported by several authors [8]. Clinical and electrophysiological studies have demonstrated defective neuromuscular transmission as a causative mechanism [9].
In bites by South Asian viperid snakes, envenoming results in local pain and tissue damage, characterised by swelling, blistering, bleeding, and necrosis at the bite site, sometimes extending to the whole limb [10]. Viperid venoms can also induce coagulopathy and platelet dysfunction, leading to spontaneous systemic haemorrhages and persistent bleeding from fang marks, wounds, or gums. Viperid venoms can also induce coagulopathy and platelet dysfunction, leading to spontaneous systemic haemorrhages and persistent bleeding from fang marks, wounds, or gums. Intracranial bleeding, including anterior pituitary haemorrhage, and multi-organ failure are common causes of death [11]. A prospective study conducted in Anuradhapura District, Sri Lanka, showed that 92% of patients with Russell's viper envenoming presented with local swelling and 77% had haemostatic disturbances [12]. Localized swelling (12, 48%), neurotoxicity (18, 72%) and coagulopathy (22, 88%) were main clinical features of Russell’s viper in our study.
Bites by kraits or sea snakes do not usually cause signs of local envenoming and can be virtually painless. Cobra venom contains mainly postsynaptic neurotoxins, which bind and block acetylcholine receptors of the neuromuscular junction, while krait venom in addition contains presynaptic toxins that damage nerve endings [13]. Extraocular muscles are particularly sensitive to neuromuscular blockade, leading to a drop of upper eyelids (bilateral ptosis), a frequently observed early sign of paralysis [13]. In our study, Neurotoxicity (35, 83.3%) was the cardinal feature of krait bite. Local effects and coagulopathy were not observed. Local swelling/tissue necrosis (12, 66.7%) and neurotoxicity (15, 83.3%) were main clinical manifestation of cobra bite.
Patients are often unable to protrude their tongue beyond the incisors and may present with difficulty speaking or swallowing. Limb weakness, loss of deep tendon reflexes, and fixed dilated pupils may follow. Once paralysis reaches the diaphragm and the intercostal muscles, victims usually die of respiratory failure if they are not adequately ventilated. Hospital-based studies in Sri Lanka showed that 48%-64% of B. caeruleus victims developed respiratory paralysis and required mechanical ventilation [13]. Acute respiratory failure (18, 51%) was the main hazard in krait bite in our study. Sever localized necrosis (2, 11.1%) and respiratory failure (3, 16.6%) were lethal complications in cobra bites.
Immunotherapy is the only specific treatment for snake bite envenoming. The success of anti-venom therapy depends on the ability of immunoglobulins to bind, extract, and eliminate toxins present in the body. While their efficacy in restoring haemostasis and cardiovascular functions is well established, the ability of anti-venoms to prevent tissue damage and to reverse neurotoxicity is more controversial [14]. In our study, All patients with systemic envenomation were managed with Anti Snake Venom (ASV) available in Sri Lanka which is a polyvalent equine serum manufactured by Indian companies (Haffkine Laboratories, Mumbai; Serum Institute of India, Pune; Vins Bio products Limited, Mumbai and Bharat Serum and Vaccine Limited Ambernath, India) using the venoms of Indian species of cobra, Russell’s viper, common krait and saw-scaled viper. There is no anti-venom production in Sri Lanka for local use despite snake bite being a major health problem. 10-20 vials of ASV were sufficient to manage the Krait and cobra bites. In viper bites, ASV was repeated in 6 hours in dose of 10 vials if coagulopathy persisted; the end point of ASV therapy was reversal of coagulopathy as determined by serial performance of the 20 WBCT.
The management of envenomed snake bites is not limited to the administration of anti-venoms. In the case of neurotoxic envenoming, artificial ventilation and careful airway management are crucial to avoid asphyxiation in patients with respiratory paralysis. Cases of complete recovery from severe neuromuscular paralysis without anti-venom have been reported after prolonged artificial ventilation [15]. Anticholinesterase drugs such as edrophonium can partly overcome blockade by postsynaptic neurotoxins and have shown good efficacy in cobra bite envenoming [16]. Bacterial infections can develop at the bite site, especially if the wound has been incised or tampered with non-sterile instruments, and may require antibiotic treatment.
Acute respiratory failure needed ventilator care in intensive care units. Acute renal failure was managed with dialysis. DIC was managed with blood products. Local effects were managed with oral /intravenous antibiotics.
In 1999, there were 32,303 cases of snakebite with a case fatality rate of 0.6% [1]. India has the highest number of deaths due to snake bites in the world with 35,000-50,000 people dying per year according to World Health Organization (WHO) direst estimates [17]. Mortality rate was 3.8% in our study. This is relatively higher compared to in India either due to delayed admission or severe envenomation.
Conclusions
Common krait, Cobra and Russell’s viper were identified snake bites in Batticaloa district. Neurotoxicity, Localized swelling and Neurotoxicity and Coagulopathy and Neurotoxicity were main clinical manifestation of krait, cobra and Russell’s viper bites respectively.
Acknowledgements
We thank the staffs of Department of Emergency, Cardiology and Poisoning Units, Teaching Hospital, Batticaloa for the help during the course of these studies.
References
- Department of health services of Sri Lanka. Mortality and morbidity tables. Annual Health Bulletin 1999; 98.
- De Silva A, Ranasinghe L. (1983) Epidemiology of snake bite in Sri Lanka: a review. Ceylon Med J ;28:144-54.
- Kasturiratne A, Wickremasinghe AR, de Silva N, Gunawardena NK, Pathmeswaran A, et al. (2008) The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deaths. PLoS Med 5: e218.
- Ariaratnam CA, Sheriff MH, Theakston RD, Warrell DA (2008) Distinctive epidemiologic and clinical features of common krait (Bungaruscaeruleus) bites in Sri Lanka. Am J Trop Med Hyg 79: 458-462.
- De Silva, Anslem(1980) Snake bite and antivenom treatment in Sri Lanka. Proc. of International seminar on epidemiology and Medical treatment of snake bites. Japan: 134-137.
- De Silva A, Ranasinghe L (1983) Epidemiology of snake bite in Sri Lanka: a review. Ceylon Med J28:144-154.
- Sharma SK, Khanal B, Pokhrel P, Khan A, Koirala S (2003) Snakebite-reappraisal of the situation in eastern Nepal. Toxicon 41: 285-289.
- Warrell DA, Looareesuwan S, White NJ, Theakston RD, Warrell MJ, et al. (1983) Severe neurotoxic envenoming by the Malayan krait Bangaruscandidus (Linnaeus): response to antivenom and anticholinesterase. Br Med J 286:678-680.
- Watt G, Theakston RDG, Hayes CG, Yambao ML, Sangalang R, Ranoa CP, et al. (1986) Positive response to edrophonium in patients with neurotoxic envenoming by cobras (Najanajaphilippinensis). A placebo-controlled study. N Engl J Med315:1444-1448.
- Warrell DA (1995) Clinical toxicology of Snake bites in Asia. In: White MA (ed.) Handbook of clinical toxicology of animal venoms and poisons. CRC Press. pp. 493-588.
- Sharma SK, Chappuis F, Jha N, Bovier PA, Loutan L, et al. (2004) Impact of snake bites and determinants of fatal outcomes in southeastern Nepal. Am J Trop Med Hyg 71: 234-238.
- Kularatne SA (2003) Epidemiology and clinical picture of the Russell's viper (Daboiarusseliirusselii) bite in Anuradhapura, Sri Lanka: a prospective study of 336 patients. Southeast Asian J Trop Med Public Health 34: 855-862.
- Ariaratnam CA, Sheriff MH, Theakston RD, Warrell DA (2008) Distinctive epidemiologic and clinical features of common krait (Bungaruscaeruleus) bites in Sri Lanka. Am J Trop Med Hyg 79: 458-462.
- Kularatne SA (2002) Common krait (Bungaruscaeruleus) bite in Anuradhapura, Sri Lanka: a prospective clinical study, 1996-98. Postgrad Med J 78: 276-280.
- Pochanugool C, Limthongkul S, Sitprija V, Benyajati C (1994) Management of cobra bite by artificial respiration and supportive therapy. J Med Assoc Thai 77: 161-164.
- Urrie B, Fitzmaurice M, Oakley J (1988) Resolution of neurotoxicity with anticholinesterase therapy in death-adder envenomation. Med J Aust 148: 522-525.
- Warrell DA (1999) WHO Guidelines for the clinical management of snake bites in the South East Asia Region. SE Asian J Trop Med Pub Health 30: 1-83.
Citation: Pirasath S*, Gnanathasan A, Thadchanamoorthy S (2015) Epidemic Poisoning with Snakes in Eastern Sri Lanka; Epidemiological and Clinical Features in Batticaloa District. Epidemiology(sunnyvale) 5:183. DOI: 10.4172/2161-1165.1000183
Copyright: © 2015 Pirasath S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 15836
- [From(publication date): 3-2015 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 11268
- PDF downloads: 4568