Eosinophilic Esophagitis: Our Experience with the Emerging Disease at a Single Center in Northern Israel
Received: 07-Jun-2024 / Manuscript No. JGDS-24-138497 / Editor assigned: 10-Jun-2024 / PreQC No. JGDS-24-138497 (PQ) / Reviewed: 24-Jun-2024 / QC No. JGDS-24-138497 / Revised: 01-Jul-2024 / Manuscript No. JGDS-24-138497 (R) / Published Date: 10-Jul-2024
Abstract
Purpose: Data on Eosinophilic esophagitis (EoE) in Israel is sparse. We appraised the clinical, endoscopic, and histological characteristics of 50 Israeli adults with EoE.
Methods: We reviewed the medical records of 50 adult patients with a diagnosis of EoE who were referred to our center at Bnai Zion Medical Center, Haifa, Israel from 2020 until 2024.
Results: 50 patients with EoE were included; the mean age at diagnosis was 34 years ± 9.5 years. The sex ratio of males to females was approximately 2:1 with 34 males (68%) and 16 females (32%). 22 of the 50 patients had a history of allergic diseases. Symptoms at diagnosis were as follows: Dysphagia was the primary presenting symptom observed (n=25, 50%), followed by food impaction (n=17, 34%) and GERD-like symptoms (n=14, 28%). Less frequent symptoms included vomiting, nausea, and chest pain. The most common endoscopic findings were normal mucosa (n=21, 42%) followed by trachealization (n=17, 34%), esophagitis (n=7, 14%), and exudates (n=5, 10%). 66% of the subjects were initially treated with proton-pump inhibitors (PPIs). 9 patients (18%) were asymptomatic without any treatment. The remaining 8 patients (16%) were given topical steroids. Clinical and histological resolution was detected in 50% of the patients who underwent a second EGD after 6 weeks-8 weeks of PPI.
Conclusion: Our current study describes the clinical features of adult patients with EoE in north Israel. This is the first demographic study in Israel that defines the clinical, endoscopic, and histological manifestations of EoE in the adult population.
Keywords
Eosinophilic esophagitis; Esophagus; Proton pump inhibitors
Introduction
Eosinophilic Esophagitis (EoE) is a chronic inflammatory disease of the esophagus which is characterized by esophageal dysfunction symptoms and eosinophilic infiltration of the esophageal mucosa with more than 15 eosinophils per high power field (HPF) [1]. The incidence and prevalence of EoE have constantly increased over time. In the past two decades and, mainly in western countries [2], EoE has become a more frequently diagnosed disease pertaining to esophageal symptoms. The pattern of the onset of the disease consists of two stages, with a first occurrence in childhood, and a second peak in the 3rd and 4th decade of life at an average age of 38 years [1,3]. Nowadays, it is considered the second most common cause of chronic esophagitis and dysphagia (after GERD, which is the leading cause) [4].
The exact pathogenesis of the disease has yet to be fully understood. However, a study has shown that it consists of an interaction between genetic and environmental factors [5].
Presently, there are no studies that have assessed the clinical characteristics of EoE in Israel. We would like to share our data of 50 cases of adult subjects diagnosed with EoE in the last 5 years (February 2019 to February 2024) at Bnai Zion Medical Center in Haifa, in the North Israel.
Materials and Methods
Study design and subjects
We performed a retrospective study of patients evaluated from 2019 to 2024 by the esophageal gastrointestinal disease clinic at the Gastroenterology Department at Bnai Zion Medical Center in Haifa, Israel. Data were extrapolated from medical records of adult subjects with the diagnosis of EoE. The diagnosis of EoE was based on the histopathology finding of more than 15 eosinophils per high power field (HPF) taken from esophageal biopsies. A total of 50 patients over 18 years of age were identified. For each subject, a personal history of atopic background, symptomatic manifestations, endoscopic and histological findings were obtained.
Statistical analysis
After collecting medical records, the data from clinical, endoscopic and initial treatment protocols were analyzed for each patient to evaluate the characteristics of the disease. Data were stored in Microsoft Office Excel 2013 (Microsoft, Redmond, WA, USA), and the variables were calculated using the SPSS program, version 23 (IBM Co., Armonk, NY, USA).
Results
Clinical characteristics
Fifty patients with EoE were included in the study. The mean age at diagnosis was 34 ± 9.5 years. The sex ratio of males to females was approximately 2:1, with 34 males (68%) and 16 females (32%).
22 (44%) patients with EoE had a history of allergic diseases, including allergic rhinitis in 22% (n=11), atopic dermatitis in 6% (n=3), food allergy in 12% (n=6), and asthma in 12% (n=6). 3 patients (6%) had two atopic diseases, and one patient had three atopic diseases, namely allergic rhinitis, asthma, and a food allergy.
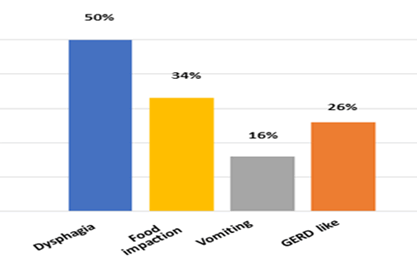
Symptoms at diagnosis were as follows: Dysphagia was the prominent presenting symptom (n=25, 50%), followed by food impaction (n=17, 34%) and GERD-like symptoms (n=14, 28%). Less frequent symptoms included vomiting, nausea, and chest pain (Figure 1).
Endoscopic findings
The main endoscopic findings were normal mucosa (n=21, 42%) followed by trachealization (n=17, 34%), esophagitis (n=7, 14%), and white exudates (n=5, 10%). Furrows, crepe paper esophagus, and edema were found in one case each (Figure 2). Biopsies were taken from the upper and lower esophagus.
Initial treatment
33 patients (66%) were treated with proton-pump inhibitors (PPIs) from the time of diagnosis. About 50% of them had a clinical and histologic remission (Figure 3). Since the 6-food elimination diet was not efficacious enough in the adult population, it was not chosen as a first-line treatment option. Initially, 9 patients (18%) had very mild disease with minimal symptoms and were asymptomatic without any treatment. The other 8 subjects (16%) were given topical steroids in the form of Budesonide oral gel (Budesonide 1 mg to be swallowed once a day, avoid food or drink for at least an hour after taking the medication), which has been replaced by Budesonide orodispersible tablets (Jorveza) since 2021. None of the patients had treatment-related adverse events at the time of follow-up. None of the patients had been previously treated with a biologic drug or any other clinical-trial drug for EoE or any other atopic disease.
Figure 3: Microscopic slides of esophageal biopsies with H and E stain of patient treated with Esomeprazol; slide before treatment with PPI showing infiltration of numerous eosinophils throughout the mucosa (red arrows) at magnification level of X40, another slide after treatment of PPI for 12 weeks showing no eosinophils throughout the mucosa at magnification level of X40
Discussion
Eosinophilic esophagitis is an emerging disease affecting both the pediatric and adult population. Israeli data on EoE is scarce. However, emerging reports on EoE from Israel have demonstrated that it is not uncommon and is probably underdiagnosed due to the medical system’s lack of awareness. Over the last decade, patients presenting with esophageal symptoms have increasingly been diagnosed with the disease all over the world. There are various hypotheses that have attempted to explain the increase in incidence. One of these hypotheses is the increase in awareness of the disease, in addition to the increasing number of the volume of the Esophagogastroduodenoscopy (EGD) examinations that have been added in the last two decades [6-8]. Nevertheless, two studies have shown that both the prevalence and the cumulative incidence of EoE have increased more than the rate of annual endoscopies during the observation [9,10].
In our demographic study, there was a significant sex difference, with a male-to-female ratio of 2:1, demonstrating that males were more affected. Males are known to have a higher prevalence than females among both children and adults. In previous studies, the ratio between men and women ranged from 2.5:1 to 3:1 [11], comparable with our ratio. This gender risk is attributed to the hereditary differences between the sexes in the cytokin receptor-like factor 2 gene, which encodes for the Thymic Stromal Lymphopoietin receptor [12].
Clinical presentation relies on the patient’s self-reported symptoms associated with esophageal dysfunction, and it can take a long time to reach a diagnosis of EoE. The most prominent presenting symptom was dysphagia, followed by food impaction, GERD-like symptoms, and vomiting. This wide range may be explained by symptoms presenting as an acute onset, such as in the case of food bolus impaction; at other times, the presentation might be more subtle and chronic.
Despite the fact that there is no pathognomonic endoscopic finding consistent with EoE, EGD is usually the first-step procedure in the management of a patient with dysphagia for solids [13]. There are endoscopic findings that are characterized with EoE, the most common of which are longitudinal furrows, white exudates, narrowings, strictures, trachealization, edema, and crepe paper mucosa [14]. These findings can usually be present in random combination in any given patient. White exudates, edema, and longitudinal furrows reflect acute inflammation, while rings, trachealization, and stenosis are the result of fibrosis due to chronic inflammatory disease. To objectively describe the endoscopic findings and give a score accordingly, endoscopists use the so-called EREFS score, which includes the five endoscopic patterns mentioned above [15]. In our study, the most common endoscopic features were normal mucosa (42%), trachealization (34%), esophagitis (14%), and white exudates (10%). The normal mucosa appearance in most of the cases observed in our study accentuates the concern of regularly performing esophageal biopsies when performing EGD. Since esophagitis comprises 14% of the endoscopic features in our study, we suggest modifying the EREFS score and to include esophagitis in its scoring system.
Since EoE is a chronic and progressive disease, life-long treatment is needed to prevent the complications of the disease. The main therapeutic goal of the treatment is to control the symptoms and reduce the inflammatory process of the esophagus [16]. Nowadays, there are several different treatment options available for EoE: Dietary treatment, pharmacological treatment, and finally, endoscopic dilatation. It should be noted that either dietary or pharmacological treatment may serve as a primary treatment option as published in the therapeutic algorithm in the guidelines of the European Society of Gastroenterology UEG [17]. However, the choice should consider the phenotype of the disease (inflammatory or fibrostenotic/obstructive), the patient's clinical background, preferences, side effects, and the physician's experience. Current pharmacologic treatment options for EoE include PPIs, swallowed steroids, and the very new biologic drug Dupilumab, a monoclonal antibody against IL4 and IL13, which has newly been approved as a second-line treatment option in persistent patients [18]. However, so far, our clinic has not had any practical experience in prescribing this drug.
Nowadays, PPIs are the first-line treatment option usually offered to patients with EoE. In our study, most of the patients received PPI as the initial treatment. The efficacy of PPIs in inducing remission appears to be related to two mechanisms, namely, by reducing acid reflux into the esophagus, leading to healing the mucosal barrier, which in turn prevents exposure to environmental allergens [19]. Additionally, they decrease the levels of eotaxin-3, a pro-inflammatory cytokine produced by Th2 cells involved in recruiting eosinophils to the esophageal mucosa [20].
PPIs are considered effective and safe. Various studies have shown clinical and histological remission in up to 50% of patients with EoE [21]. In everyday practice, they are one of the most common first-line treatment options available, especially for the adult population.
Corticosteroids are known for their anti-inflammatory effect, the reduction of esophageal constriction, and improving the integrity of the esophageal barrier with the outer lumen.
Topical viscous formulations and dispersible tablet formulations are considered optimal delivery methods. In recent years, budesonide gel injections have been replaced by Orodispersible tablets of budesonide (Jorveza), which currently represent a convenient and available option for local steroid treatment.
Jorveza has been evaluated in multiple placebo-controlled trials and found to be effective in inducing clinical and histological responses when administered at an induction dose of 1 mg twice daily for 12 weeks [22]. Followed by an extension trial of 204 patients with EoE, a maintenance dose of 1 mg per day was administered and also proved its effectiveness for 48 weeks in 75% of the subjects [23]. Despite these impressive results, in our study, PPIs were the most frequently prescribed first-line treatment, probably due to our lack of experience at the time with the newly introduced Jorveza during the period of the study.
Conclusion
Our study describes the demographic characteristics of the adult population with EoE in northern Israel. To the best of our knowledge, it is the first study conducted in Israel that describes the clinical, endoscopic, and histological manifestations of EoE. Our population findings were comparable to those of other studies, except for the endoscopic findings. We suggest adding esophagitis to the current endoscopic scoring system as mentioned above. Most patients in this study demonstrated a good clinical response to PPI treatment. A population-based, multi-center study with long-term follow-up is warranted to estimate the prevalence and incidence of EoE in Israel.
Acknowledgement
None.
Conflict of Interest
The author’s declared that they have no conflict of interest.
References
- Liacouras CA, Furuta GT, Hirano I, Atkins D, Attwood SE, et al. (2011) Eosinophilic esophagitis: Updated consensus recommendations for children and adults. J Allergy Clin Immunol 128: 3-20.
- Dellon ES, Hirano I (2018) Epidemiology and natural history of eosinophilic esophagitis. Gastroenterology 154: 319-332.
- Weiss AH, Iorio N, Schey R (2015) Esophageal motility in eosinophilic esophagitis. Rev Gastroenterol Mex 80: 205-13.
- Arias A, Perez-Martinez I, Tenias JM, Lucendo AJ (2016) Systematic review with meta-analysis: The incidence and prevalence of eosinophilic oesophagitis in children and adults in population based studies. Aliment Pharmacol Ther 43: 3-15.
- Alexander ES, Martin LJ, Collins MH, Kottyan LC, Sucharew H, et al. (2014) Twin and family studies reveal strong environmental and weaker genetic cues explaining heritability of eosinophilic esophagitis. J Allergy Clin Immunol 134: 1084-1092.
- Mahesh VN, Holloway RH, Nguyen NQ (2013) Changing epidemiology of food bolus impaction: Is eosinophilic esophagitis to blame? J Gastroenterol Hepatol 28: 963-68.
- Dellon ES (2014) Epidemiology of eosinophilic esophagitis. Gastroenterol Clin North Am 43: 201-18.
- Ali MA, Lam-Himlin D, Voltaggio L (2012) Eosinophilic esophagitis: Aclinical, endoscopic, and histopathologic review. Gastrointest Endosc 76: 1224-1237.
- Straumann A, Spichtin HP, Grize L, Bucher KA, Beglinger C, et al. (2003) Natural history of primary eosinophilic esophagitis: A follow-up of 30 adult patients for up to 11.5 years. Gastroenterology 125:1660-1669.
- Giriens B, Yan P, Safroneeva E, Zwahlen M, Reinhard A, et al. (2015) Escalating incidence of eosinophilic esophagitis in Canton of Vaud, Switzerland, 1993-2013: A population-based study. Allerg 70(12):1633-1639.
- Lucendo AJ, Molina-Infante J, Arias A, Arnim UV, Bredenoord AJ, et al. (2017) Guidelines on eosinophilic esophagitis: Evidence-based statements and recommendations for diagnosis and management in children and adults. United European Gastroenterol J 5: 335-358.
- Davis BP (2018) Pathophysiology of eosinophilic esophagitis. Clin Rev Allergy Immunol 55: 19-42.
- Varadarajulu S, Eloubeidi MA, Patel RS, Mulcahy HE, Barkun A, et al. (2005) The yield and the predictors of esophageal pathology when upper endoscopy is used for the initial evaluation of dysphagia. Gastrointest Endosc 61(7): 804-808.
- Remedios M, Campbell C, Jones DM, Kerlin P (2006) Eosinophilic esophagitis in adults: Clinical, endoscopic, histologic findings, and response to treatment with fluticasone propionate. Gastrointest Endosc 63: 3-12.
- Hirano I, Moy N, Heckman MG, Thomas CS, Gonsalves N, et al. (2013) Endoscopic assessment of the oesophageal features of eosinophilic oesophagitis: Validation of a novel classification and grading system. Gut 62: 489-495.
- Dellon ES, Liacouras CA, Molina-Infante J, Furuta GT, Spergel JM, et al. (2018) Updated international consensus diagnostic criteria for eosinophilic esophagitis: Proceedings of the AGREE Conference. Gastroenterology. 155(4): 1022-1033.
- Lucendo AJ, Molina-Infante J, Árias A, Arnim UV, Bredenoord AJ, et al. (2017) Guidelines on eosinophilic esophagitis: Evidence-based statements and recommendations for diagnosis and management in children and adults. United European Gastroenterol J 5: 335-358.
- Dellon ES, Rothenberg ME, Collins MH, Hirano I, Chehade M, et al. (2022) Dupilumab in adults and adolescents with eosinophilic esophagitis. N Engl J Med 387(25): 2317-2330.
- Van Rhijn BD, Weijenborg PW, Verheij J, Van Den Bergh Weerman MA, Verseijden C, et al. (2014) Proton pump inhibitors partially restore mucosal integrity in patients with proton pump inhibitor-responsive esophageal eosinophilia but not eosinophilic esophagitis. Clin Gastroenterol Hepatol 12: 1815-1823.
- Cheng, E, Zhang, X, Huo, X, Yu C, Zhang Q, et al. (2013) Omeprazole blocks eotaxin-3 expression by oesophageal squamous cells from patients with eosinophilic oesophagitis and GORD. Gut 62(6): 824-832.
- Laserna-Mendieta EJ, Casabona S, Savarino E, Perelló A, Martínez IP, et al. (2020) Efficacy of therapy for eosinophilic esophagitis in real-world practice. Clin Gastroenterol Hepatol 18: 2903-2911.
- Lucendo AJ, Miehlke S, Schlag C, Vieth M, Biedermann L, et al. (2019) Efficacy of budesonide orodispersible tablets as induction therapy for eosinophilic esophagitis in a randomized placebo-controlled trial. Gastroenterology 157(1): 74-86.
- Straumann A, Lucendo AJ, Miehlke S, Vieth M, Schla C, et al. (2020) Budesonide orodispersible tablets maintain remission in a randomized, placebo-controlled trial of patients with eosinophilic esophagitis. Gastroenterology 159(5): 1672-1685.
Citation: Hindy J, Rainis T (2024) Eosinophilic Esophagitis: Our Experience with the Emerging Disease at a Single Center in Northern Israel. J Gastrointest Dig Syst. 14:804.
Copyright: © 2024 Hindy J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 692
- [From(publication date): 0-2024 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 506
- PDF downloads: 186