Case Report Open Access
Endoscopic Multiple Gastric Polypectomy in Two Phage of the Same Patient - A Case Report and Discussion
Abu Taiub Mohammed Mohiuddin Chowdhury* and Zhuo Yue
Department of Digestive Disease, 1st Affiliated Hospital of Jiamusi University, Jiamusi, Heilongion, China
- Corresponding Author:
- Abu Taiub Mohammed Mohiuddin Chowdhury
Department of Digestive Disease -II
First Affiliated Hospital of Jiamusi University, Jiamusi, China
Tel: 008618745463632
E-mail: dr_mohiuddinchy@yahoo.com
Received Date: June 07, 2014; Accepted Date: July 29, 2014; Published Date: August 04, 2014
Citation: Mohiuddin Chowdhury ATM, Yue Z (2014) Endoscopic Multiple Gastric Polypectomy in Two Phage of the Same Patient - A Case Report and Discussion. J Gastroint Dig Syst 4:202. doi:10.4172/2161-069X.1000202
Copyright: © 2014 Mohiuddin Chowdhury ATM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
A POLYP is defined as a proliferative or neoplastic lesion of gastrointestinal mucosal layer. It is a "polypoid lesion" which appeared at endoscopy, protruding into the lumen of digestive tract as discrete projection above the adjacent mucosal surface. In most cases, polyps are incidental findings during routine endoscopy, also they are typically found incidentally when upper gastrointestinal endoscopy is performed for an unrelated indication. These lesions have previously been accepted as completely benign but Gastric adenomas have a higher incidence of malignant transformation than adenomatous polyps in colon. Though polypectomy has various immediate and delayed complications, Specially in case of multiple polypectomy. Multiple polypectomy has been advised and applied in several phages for the achievement of complete removal of polypoid lesions in same patient. In the aim to reduce the frequency of this invasive procedure and to achieve a probable safe limit in a single phase we performed an evaluatory multiple endoscopic gastric polypectomy under extensive precaution and close supervision in two phages of a same patient. To avoid possible hazards and to minimize the complication as possible we choose a non-diabetic, non-hypertensive patient with no established cardiovascular disorder. In first phage a number of thirty two and in second phage twenty nine gastric polyps had been success fully removed by electro coagulation without any immediate or delayed complications.
Keywords
Polyp; Gastric polypectomy; Multiple gastric polyp; Endoscopic polypectomy; Polypectomy and complication
Introduction
Multiple gastric polypectomy has been advised and performed in several settings in a same patient to remove possible complications and the threat of malignant transformation of polyps. In the aim to reduce the number of frequency of endoscopic invasion and to achieve a probable safe limit of the number of gastric polypectomy we performed an evaluatory multiple endoscopic gastric polypectomy under extensive precaution and close supervision in two phages of a same patient. To avoid possible hazards and to minimize the complication as possible we choose a non diabetic, non hypertensive patient with no established cardiovascular disorder.
Case Report
We report a 66 years old female patient presented to the outpatient department of Gastroenterology complaining upper abdominal pain for a period three months with loss of appetite and occasional nausea. On examination the patient was generally healthy, her upper abdomen was moderately tender and no significant major systemic disease was found. She was non diabetic and not hypertensive. With history of occasional PPI intake. The patient denied weight loss, history of altered bowl habit or use of NSAID.
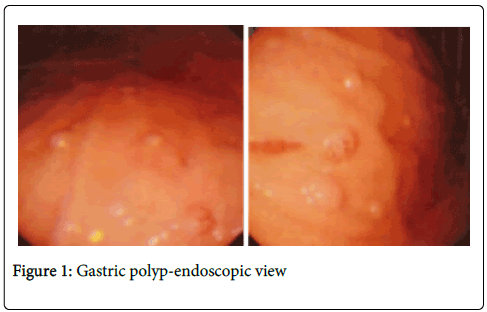
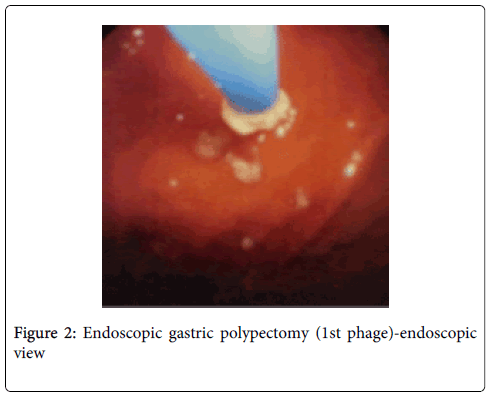
Her clinical examination and routine blood tests were normal. But upper GI endoscopy reveals feature of gastritis with multiple gastric polyps about sixty in number of <0.6 cm (Figure 1). While a colonoscopy revel no abnormality. In the first attempt with proper preparation 32 polyps were endoscopically removed (Figure 2) successfully by electro coagulation. During polypectomy procedure no immediate hemorrhage is seen.
After the polypectomy the patient was kept under close observation with routine post procedural treatment for three days. No post polypectomy complication or hemorrhage is noted. Her stool color was normal. The patient was discharged with medication and advised for the second phage of polypectomy after seven days if no complication arises.
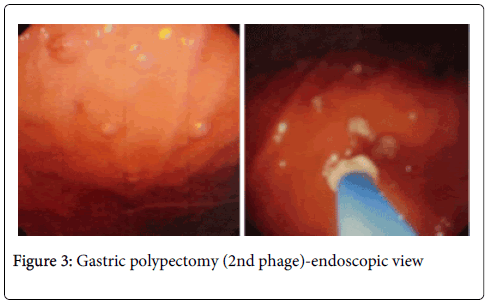
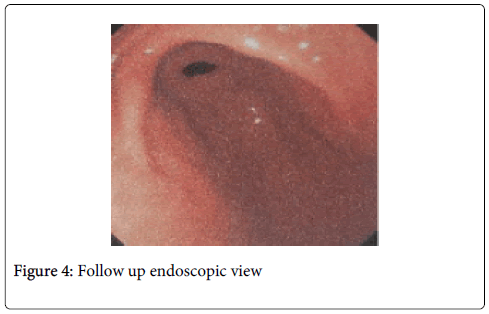
In the second attempt twenty nine gastric polyps (Figure 3) were endoscopically removed without any complication. Previous polypectomy sites show excellent recovery (Figure 4) with no sign of ulceration or any other lesion. The patient was kept under close observation for three days with post polypectomy treatment and no complications were observed.
Her 15th and 30th day follow up shows no detectable complication with significant improvement of the previous complains. Evidence of upper GI hemorrhage or change of stool color was denied. Physical examination reveals no sign of anemia, soft non tender abdomen with normal bowel sound.
Conclusion
Though in our patient no complication was seen during the polypectomy procedure and no evidence of immediate or delayed post polypectomy complication was noted, but further extensive study is required to achieve a safe limit margin of multiple polypectomy in a single setting.
Discussion
A POLYP is defined as a proliferative or neoplastic lesion of gastrointestinal mucosal layer [1]. It is a “polypoid lesion” which appeared at endoscopy, protruding into the lumen of digestive tract as discrete projection above the adjacent mucosal surface. Usually they are found in 2-3% of all gastroscopic examinations [2]. In most cases, polyps are incidental findings during routine endoscopy, also they are typically found incidentally when upper gastrointestinal endoscopy is performed for an unrelated indication [3,4]. The most common types of benign epithelial gastric polyps (BEGP) are fundic gland polyps, hyperplastic polyps and adenomas. If there are multiple gastric polyps present, these are usually of the same histological type [5]. Polyps were classified macroscopically according to Yamada’s classification [6]. Yamada type I polyps are elevated, with an indistinct border. Type II polyps are elevated with a distinct border at the base but no notch. Type III polyps are elevated, but no peduncle. Type IV polyps are pedunculated and elevated.
Gastric polyps rarely produce symptoms like haemorrhage and delayed gastric emptying [3,7]. But the surrounding mucosa often shows features of atrophic gastritis with patchy intestinal metaplasia. Associated presentation with other conditions, such as chronic atrophic gastritis and pernicious anemia and upper gastrointestinal bleeding (typically occult) or obstruction is also noted [8]. Polyp formation is strongly associated with chronic gastritis; Helicobacter-associated gastritis, pernicious anemia, reactive or chemical gastritis, when adjacent to ulcer erosions and around gastroenterostomy stomas [8,9]. These lesions have previously been accepted as completely benign. However, some current studies showed that they might include adenomatous changes or dysplastic areas [9-12]. Gastric adenomas have a higher incidence of malignant transformation than adenomatous polyps in colon [13]. Hyperplastic polyps account for approximately 75% of gastric polyps [14] and are believed to develop as a consequence of mucosal response to tissue injury and inflammation. Which were previously considered completely benign but recent evidence shows small but well-defined malignant potential [15,16]. The reported frequencies of dysplastic foci within hyperplastic polyps showed a wide range (4-22 %) [17,18]. Hizawa [19] and Zea-Iriarte [20] found the incidence of malignancy in hyperplastic polyps was 2 % and 1.8 %, respectively. Though there is an increased risk of adenocarcinoma elsewhere in the stomach because of association of chronic gastritis, particularly autoimmune gastritis and H.pylori gastritis [20,21]. A positive association between FGPs and acid suppression was first reported in 1992 [22]. This is possibly because of this that PPIs elevate serum gastrin, which is a growth factor for oxyntic mucosa and a downstream target of Wnt signaling [23,24]. Beside that however the second step in FGP formation is considered as the formation of Fundic gland cyst secondary to dilated glands, as the fundic gland cysts enlarge subsequently they develop into FGPs [25]. Some studies do indicate association between use of proton pump inhibitors and fundic gland polyps (FGPs) and a 4-fold increase in the risk of developing FGPs with long-term PPI use [26,27]. In a study FGPs were present in 23% of patients on PPIs compared with 12% of patients not taking a PPI [27]. The incidence of gastric cancer is increased in patients with FGPs (Fundic Gland Polyps) and FAP (Familial Adenomatous Polyposis) [28]. The pathogenesis and cancer risk of FGPs are not well understood. FGPs in FAP arise from mutational inactivation of the adenomatous polyposis coli gene, whereas sporadic FGPs are usually caused by activating mutations of the b-catenin gene [29]. A study reported a significantly lower rate of FGP dysplasia in FAP patients taking acid suppressive medications (histamine antagonist or PPI) versus patients not using these medications [30].
Complete removal of gastric polyp is recommended by experienced endoscopist of all epithelial gastric polyps larger than 5 mm after thorough individualized risk-benefit analysis [31,32]. Though there is an existing debate between taking biopsy before performing Polypectomy. However, forceps biopsies carried the risk of missing the neoplastic foci within polyp, since only a small portion of the lesion was sampled in this technique [33]. Seifert and Elster [34] showed a remarkable discrepancy of 70 % of cases between histopathologic results of biopsy materials and polypectomy specimens compared in same lesions. With this observation, the authors recommended to remove all gastric polyps larger than 5 mm in diameter [33,35].
Repeat gastroscopy should be performed at 1 year following complete polypectomy for high risk polyps [36]. Bleeding is the primary complication of polypectomy [37] and it has been reported to be as high as 3% to 6.1% [36-43]. Gastric perforation during endoscopic polypectomy is also having been reported [44]. Endoscopic post polypectomy hemorrhage can be immediate or be delayed from hours to up to 29 days [40-42]. Polyps up to 1 cm in diameter have been safely removed in patients on warfarin therapy. In a report of 225 polypectomy in 123 anticoagulated patients, three patients bled (one requiring treatment) [45]. Risk of significant bleeding is greatest with sessile polyps larger than 2 cm in diameter, followed by those with a thick stalk; significant bleeding is unlikely to occur if a small polyp is removed with a snare without cautery [46]. The reported incidence of perforation during polypectomy of “normal-sized” polyps ranges from 0.3%-0.5% [47]. Though the complications of polypectomy widely vary as presented in literature, polyp size has been the most important identified risk factor for both hemorrhage and perforation. Age = 65 years, Hypertension, cardiovascular or chronic renal disease, use of anticoagulants, poor bowel preparation, cutting mode of electrosurgical current, and inadvertent cutting of a polyp before current application are also identified risk factors. A total of 6617 cases of colorectal polypectomy was performed in 3138 consecutive patients in Japan shows that Hypertension is a significant risk factor for delayed colorectal postpolypectomy hemorrhage. The interval between polypectomy and hemorrhage can be as long as 14 days in the presence of hypertension [48]. Though Hemorrhage was the most frequent complication even if it remains questionable whether the bleeding should be considered a complication when it occurs during the procedure and is effectively and immediately controlled by Endoscopic means [49].
References
- Crawford JM. The gastrointestinal tract. In: Cotran RS, Kumar V, Robbins SL, eds. Pathologic Basis of Disease. 6th ed. Philadelphia: W. B. Saunders Company 1999: 775-843.
- Dent TL, Kukora JS, Buinewicz BR (1989) Endoscopic screening and surveillance for gastrointestinal malignancy. SurgClin North Am 69: 1205-1225.
- Oberhuber G, Stolte M (2000) Gastric polyps: an update of their pathology and biological significance. Virchows Arch 437: 581-590.
- Hattori T (1985) Morphological range of hyperplastic polyps and carcinomas arising in hyperplastic polyps of the stomach. J ClinPathol 38: 622-630.
- Deppisch LM, Rona VT (1989) Gastric epithelial polyps. A 10-year study. J ClinGastroenterol 11: 110-115.
- Yamada T, Ichikawa H (1974) X-ray diagnosis of elevated lesions of the stomach. Radiology 110: 79-83.
- Gencosmanoglu R, Sen-Oran E, Kurtkaya-Yapicier O, Avsar E, Sav A, et al. (2003) Gastric polypoid lesions: analysis of 150 endoscopic polypectomy specimens from 91 patients. World J Gastroenterol 9: 2236-2239.
- Abraham SC, Singh VK, Yardley JH, Wu TT (2001) Hyperplastic polyps of the stomach: associations with histologic patterns of gastritis and gastric atrophy. Am J SurgPathol 25: 500-507.
- Ohkusa T, Miwa H, Jojo M, Kumagai J, Tanizawa T et al. (2003) Endoscopic, histological and serologic findings of gastric hyperplastic polyps after eradication of Helicobacter pylori: comparison between responder and non-responder cases. Digestion 68: 57-62.
- Dean PG, Davis PM, Nascimento AG, Farley DR (1998) Hyperplastic gastric polyp causing progressive gastric outlet obstruction. Mayo ClinProc 73: 964-967.
- Debongnie JC (1999) Gastric polyps. ActaGastroenterolBelg 62: 187-189.
- Declich P, Ambrosiani L, Grassini R, Tavani E, Bellone S, et al. (2000) Fundic gland polyps: a still elusive entity on the eve of the year 2000. Pol J Pathol 51: 3-8.
- Ljubicic N, Kujundzic M, Roic G, Banic M, Cupic H, et al. (2002) Benign epithelial gastric polyps--frequency, location, and age and sex distribution. CollAntropol 26: 55-60.
- Turner JR, Odze RD (2004) Polyps of the stomach. In: Odze RD, Goldblum JR, Crawford JM, editors.Surgical pathology of the GI tract, Liver, Biliary tract and Pancreas. 1st edition. Philadelphia: Saunders: 267-294.
- Orlowska J, Jarosz D, Pachlewski J, Butruk E (1995) Malignant transformation of benign epithelial gastric polyps. Am J Gastroenterol 90: 2152-2159.
- Sebastian MW (1997) Benign tumors of stomach. In: Sabiston DC, editor.The biological basis of modern surgical practice. Philadelphia: W.B. Saunders 868-875.
- DaiboM, Itabashi M, Hirota T (1990) Malignant trasformation of gastric hyperplastic polyps. Am J Gastroenterol 85: 327-328.
- Davaris P, Petraki K, Archimandritis A, Haritopoulos N, Papacharalampous N (1986) Mucosal hyperplastic polyps of the stomach. Do they have any potential to malignancy? Pathol Res Pract 181: 385-389.
- Hizawa K, Fuchigami T, Iida M, Aoyagi K, Iwashita A, et al. (1995) Possible neoplastic transformation within gastric hyperplastic polyp. Application of endoscopic polypectomy. SurgEndosc 9: 714-718.
- Zea-Iriarte WL, Sekine I, Itsuno M, Makiyama K, Naito S, et al. (1996) Carcinoma in gastric hyperplastic polyps. A phenotypic study. Dig Dis Sci 41: 377-386.
- Tomasulo J (1971) Gastric polyps. Histologic types and their relationship to gastric carcinoma. Cancer 27: 1346-1355.
- Graham JR (1992) Gastric polyposis: onset during long-term therapy with omeprazole. Med J Aust 157: 287-288.
- Koh TJ, Bulitta CJ, Fleming JV, Dockray GJ, Varro A, et al. (2000) Gastrin is a target of the beta-catenin/TCF-4 growth-signaling pathway in a model of intestinal polyposis. J Clin Invest 106: 533-539.
- Koh TJ, Chen D (2000) Gastrin as a growth factor in the gastrointestinal tract. RegulPept 93: 37-44.
- Cats A, Schenk BE, Bloemena E, Roosedaal R, Lindeman J, et al. (2000) Parietal cell protrusions and fundic gland cysts during omeprazole maintenance treatment. Hum Pathol 31: 684-690.
- Stolte M, Sticht T, Eidt S, Ebert D, Finkenzeller G (1994) Frequency, location, and age and sex distribution of various types of gastric polyp. Endoscopy 26: 659-665.
- Jalving M, Koornstra JJ, Wesseling J, Boezen HM, DE Jong S, et al. (2006) Increased risk of fundic gland polyps during long-term proton pump inhibitor therapy. Aliment PharmacolTher 24: 1341-1348.
- Zwick A, Munir M, Ryan CK, Gian J, Burt RW, et al. (1997) Gastric adenocarcinoma and dysplasia in fundic gland polyps of a patient with attenuated adenomatous polyposis coli. Gastroenterology 113: 659-663.
- Abraham SC, Nobukawa B, Giardiello FM, Hamilton SR, Wu TT (2001) Sporadic fundic gland polyps: common gastric polyps arising through activating mutations in the beta-catenin gene. Am J Pathol 158: 1005-1010.
- Bianchi LK, Burke CA, Bennett AE, Lopez R, Hasson H, et al. (2008) Fundic gland polyp dysplasia is common in familial adenomatous polyposis. ClinGastroenterolHepatol 6: 180-185.
- Yoon WJ, Lee DH, Jung YJ, Jeong JB, Kim JW, et al. (2006) Histologic characteristics of gastric polyps in Korea: emphasis on discrepancy between endoscopic forceps biopsy and endoscopic mucosal resection specimen. World J Gastroenterol 12: 4029-4032.
- Molaei M, Mashayekhi R, Zojaji H, Haghazali M, Reza Zali M (2008) Gastroenterology and Hepatology From Bed to Bench. Gastric polypoid lesions: analysis of histopathologic features of 107 endoscopic polypectomy specimens 1: 127-132.
- Muehldorfer SM, Stolte M, Martus P, Hahn EG, Ell C; Multicenter Study Group "Gastric Polyps" (2002) Diagnostic accuracy of forceps biopsy versus polypectomy for gastric polyps: a prospective multicentre study. Gut 50: 465-470.
- Seifert E, Elster K (1975) Gastric polypectomy. Am J Gastroenterol 63: 451-456.
- Ginsberg GG, Al-Kawas FH, Fleischer DE, Reilly HF, Benjamin SB (1996) Gastric polyps: relationship of size and histology to cancer risk. Am J Gastroenterol 91: 714-717.
- The management of gastric polyps (2010). Andrew F Goddard, RawyaBadreldin, D Mark Pritchard, et al. Gut 59: 1270.
- Freeman HJ (2005) Endoscopic excision of a prolapsing malignant polyp which caused intermittent gastric outlet obstruction. World J Gastroenterol 11: 5245-5247.
- Waye JD, Lewis BS, Yessayan S (1992) Colonoscopy: a prospective report of complications. J ClinGastroenterol 15: 347-351.
- Gibbs DH, Opelka FG, Beck DE, Hicks TC, Timmcke AE, et al. (1996) Postpolypectomy colonic hemorrhage. Dis Colon Rectum 39: 806-810.
- Waye JD, Kahn O, Auerbach ME (1996) Complications of colonoscopy and flexible sigmoidoscopy. GastrointestEndoscClin N Am 6: 343-377.
- Rosen L, Bub DS, Reed JF 3rd, Nastasee SA (1993) Hemorrhage following colonoscopicpolypectomy. Dis Colon Rectum 36: 1126-1131.
- Sorbi D, Norton I, Conio M, Balm R, Zinsmeister A, et al. (2000) Postpolypectomy lower GI bleeding: descriptive analysis. GastrointestEndosc 51: 690-696.
- Levin TR, Zhao W, Conell C, Seeff LC, Manninen DL, et al. (2006) Complications of colonoscopy in an integrated health care delivery system. Ann Intern Med 145: 880-886.
- Katsinelos P, Beltsis A, Paroutoglou G, Galanis I, Tsolkas P, et al. (2004)Endoclipping for gastric perforation after endoscopic polypectomy: an alternative treatment to avoid surgery. SurgLaparoscEndoscPercutan Tech 14: 279-281.
- Friedland S, Sedehi D, Soetikno R (2009) Colonoscopicpolypectomy in anticoagulated patients. World J Gastroenterol 15: 1973-1976.
- Bleeding after colonic polypectomy. R Saltzman, MD, FACP, FACG, FASGE, AGAF
- Waye JD (1993) Management of complications of colonoscopicpolypectomy. Gastroenterologist 1: 158-164.
- Watabe H, Yamaji Y, Okamoto M, Kondo S, Ohta M, et al. (2006) Risk assessment for delayed hemorrhagic complication of colonic polypectomy: polyp-related factors and patient-related factors,Gastrointestinal Endoscopy 64: 73-78.
- Consolo P, Luigiano C, Strangio G, Scaffidi MG, Giacobbe G, et al. (2008) Polypectomy: Ten year experience at a single center. World J Gastroenterol 14: 2364-2369.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15605
- [From(publication date):
August-2014 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 11024
- PDF downloads : 4581