Case Report Open Access
Endoscopic Curative Treatment of a Submucosal Invasive Rectal Adenocarcinoma
Carlos Eduardo Oliveira dos Santos1*, Daniele Malaman1, César Vivian Lopes2 and Júlio Carlos Pereira-Lima21Department of Gastroenterology and Endoscopy, Santa Casa de Caridade Hospital, Bagé, RS, Brazil
2Department of Gastroenterology and Endoscopy, Santa Casa Hospital, Porto Alegre, RS, Brazil
- *Corresponding Author:
- Carlos Eduardo Oliveira dos Santos
Rua Gomes Carneiro, 1343, CEP 96400-130, Bagé-RS, Brazil
Tel: +55-53-3241-6955
E-mail: clinica@endosantos.com.br
Received date: May 23, 2014; Accepted date: June 18, 2014; Published date: June 24, 2014
Citation: Oliveira dos Santos CE, Malaman D, Lopes CV, Pereira-Lima JC (2014) Endoscopic Curative Treatment of a Submucosal Invasive Rectal Adenocarcinoma. J Gastroint Dig Syst 4:193. doi:10.4172/2161-069X.1000193
Copyright: © 2014 Oliveira dos Santos CE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
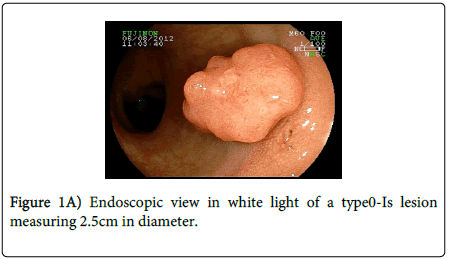
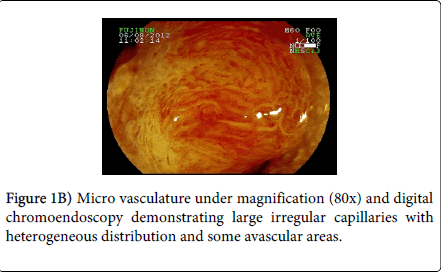
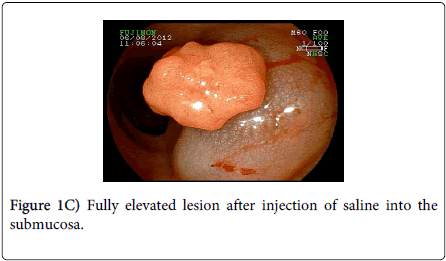
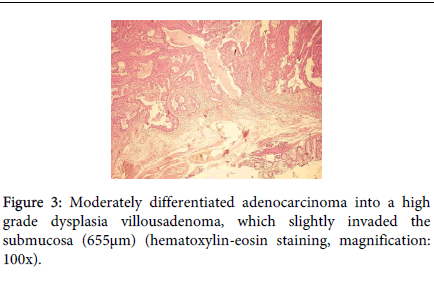
We report a case of a 45-year-old man with the diagnosis of rectal adenocarcinoma, in which a proctocolectomy was proposed and the patient refrained from surgery. A new colonoscopy was performed, which revealed a 2.5 cm diameter sessile lesion with irregular microvascular mesh work, thick capillaries with heterogeneous distribution and avascular areas, suggesting carcinoma with massive invasion of the sub-mucosa (a C3 lesion in the Hiroshima classification). However, we tried endoscopic resection and the lesion has completely elevated after Sub-mucosal hipertonic saline injection. Then the lesion was removed “en block” with a polypectomy snare. Histopathological study evidenced a moderately differentiated adenocarcinoma in a villous adenoma with high grade dysplasia with sub-mucosal invasion of 655 μm; there was no angiolymphatic invasion and the lateral and lower margins were lesion-free.
Abstract
We report a case of a 45-year-old man with the diagnosis of rectal adenocarcinoma, in which a proctocolectomy was proposed and the patient refrained from surgery. A new colonoscopy was performed, which revealed a 2.5 cm diameter sessile lesion with irregular microvascular mesh work, thick capillaries with heterogeneous distribution and avascular areas, suggesting carcinoma with massive invasion of the sub-mucosa (a C3 lesion in the Hiroshima classification). However, we tried endoscopic resection and the lesion has completely elevated after Sub-mucosal hipertonic saline injection. Then the lesion was removed “en block” with a polypectomy snare. Histopathological study evidenced a moderately differentiated adenocarcinoma in a villous adenoma with high grade dysplasia with sub-mucosal invasion of 655 µm; there was no angiolymphatic invasion and the lateral and lower margins were lesion-free.
Keywords
Colonoscopy; Colorectal neoplasm; Endoscopic diagnosis; Endoscopic mucosal resection
Introduction
Lymph node metastases are found in up to 15% of colorectal cancers that invade the submucosa. Lymphovascular invasion, cellular differentiation and depth of invasion are predictive of lymph node metastases [1,2].
Chromoendoscopy is an important tool for the differential diagnosis of neoplastic and non-neoplastic lesions and could also be employed in predicting submucosal invasion by early colorectal cancer [3]. We report, herein, a case of a sessile polyp which presented vascular characteristics of deep sub mucosal invasion on magnifying chromoendoscopy. Nevertheless, the lesion was successfully treated by endoscopic mucosal resection (EMR).
Case Report
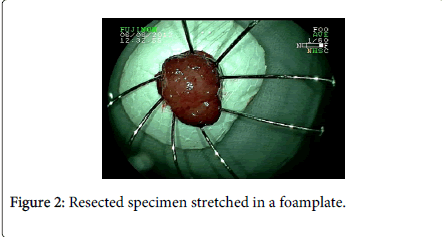
A 45 year-old man with lower abdominal discomfort underwent a colonoscopy at another hospital, which revealed a rectal adenocarcinoma at biopsy. Surgical consultation recommended surgical resection with rectal amputation, which was refused by the patient. A family doctor referred the patient to our unit and a new colonoscopy was performed (Fujinon 590ZW5 high-resolution magnifying video colonoscope -Fujifilm Corp., Saitama, Japan), which revealed a sessile polypoid lesion with a diameter of 2.5 cm, with a small fibrin-covered ulcer (Figure 1A). The lesion surface showed an irregular microvasculature, thick capillaries with a heterogeneous distribution, including avascular areas (Figure 1B). This pattern is highly suggestive of deep invasion of the submucosa (Sm–m) as seen by digital chromoendoscopy with magnification as seen by digital chromoendoscopy with magnification. Thus, surgical treatment should be indicated. However, we tried an EMR, and the lesion was completely elevated after submucosal saline injection (Figure 1C), being grasped with a polypectomy snare and resected “ en bloc ” (Figure 2). At histopathology, the specimen demonstrated to be a moderately differentiated adenocarcinoma in a villous adenoma with high grade dysplasia, with a 655 µm submucosal invasion, no angiolymphatic invasion and the resected margins were lesion-free (Figure 3). Eighteen months after endoscopic mucosal resectionand follow-upevery 6 months (Figure 4), no recurrence was observed.
Discussion
Lymph node metastases – the limiting factor for endoscopic cancer resection – are associated with the depth of submucosal invasion. So, a predictive analysis of depth of invasion by endoscopy or endoscopic ultrasound is of paramount importance to determine the therapeutic strategy for early colorectal cancers. In the Hiroshima Classification of vascular pattern in colorectal lesions, Sm-m invasion occurs only in the C type, which is subdivided in C1 (irregular vessels with a homogeneous distribution), C2 (irregular capillaries with heterogeneous distribution), and C3 (irregular capillaries, thick heterogeneous vessels with avascular areas) as in our case [4].
Kanao et al. [4] demonstrated 11%, 54% and 100% of Sm-m invasion with types C1, C2 and C3, respectively. Oka et al. [5] found similar figures of 3%, 57%, and 93%, respectively. Sensitivity, specificity and accuracy of this classification are between 64% – 100%, 89% – 100%, and 88% – 98% in different studies [6-9].
According to the guidelines of the Japanese Colorectal Cancer Society [10], EMR is considered curative when the resection is complete, the carcinoma is well or moderately differentiated, there is no angiolymphatic invasion and the depth of invasion is less than 1000 µm. According to other groups, these criteria could be even expanded to 1300 or 1500 µm [2,11]. Nakadoi et al. [12] found lymph node metastases in 8.22% of 499 colorectal lesions with submucosal invasion. All metastatic lesions were undifferentiated, had vascular invasion or had a depth of invasion greater than 1800 µm. Other treatment options are endoscopic submucosal dissection (ESD) and transanal endoscopic microsurgery (TEM). In Brazil, few endoscopy units perform ESD as well as TEM. We have a long experience with EMR, which has been a very safe and effective procedure in our endoscopic unit, and carries significant less morbidity than surgical treatment. In a previous study by our group, complete resection with EMR was achieved in 155 of 172 (90%) cases with few complications and recurrences [13].
This way, for all the reasons listed above, in the presence of colorectal lesions without clear conditions for endoscopic resection, or when the patient refuses, or is frail to undergo surgery, or the surgical procedure is too mutilant, as in this case, it is important to highlight the value of clinical judgment for the best therapeutic decision-making. The lifting or not of the lesion after submucosal saline injection should be attempted, since magnifying chromoendoscopy, either virtual or by means of dyes, does not present an accuracy of 100% for the prediction of deep submucosal invasion, as we have demonstrated in this case report.
In summary, this case presented with typical chromoendoscopic characteristics of a Sm-m submucosal cancer. However, EMR showed to be curative. Thus, in expert hands, EMR could be attempted to accurately stage and even cure early colorectal cancers when they elevate after submucosal saline injection.
References
- Choi PW, Yu CS, Jang SJ, Jung SH, Kim HC, et al. (2008) Risk factors for lymph node metastasis in submucosal invasive colorectal cancer. World J Surg 32: 2089-2094.
- Tominaga K, Nakanishi Y, Nimura S, Yoshimura K, Sakai Y, et al. (2005) Predictive histopathologic factors for lymph node metastasis in patients with nonpedunculated submucosal invasive colorectal carcinoma. Dis Colon Rectum 48:92-100.
- dos Santos CE, Lima JC, Lopes CV, Malaman D, Salomão AD, et al. (2010) Computerized virtual chromoendoscopy versus indigo carmine chromoendoscopy combined with magnification for diagnosis of small colorectal lesions: a randomized and prospective study. Eur J Gastroenterol Hepatol 22: 1364-1371.
- Kanao H, Tanaka S, Oka S, Hirata M, Yoshida S, et al. (2009) Narrow-band imaging magnification predicts the histology and invasion depth of colorectal tumors. Gastrointest Endosc 69: 631-636.
- Oka S, Tanaka S, Takata S, Kanao H, Chayama K (2011) Clinical usefulness of narrow band imaging magnifying classification for colorectal tumors based on both surface pattern and microvessel features. Dig Endosc 23 Suppl 1: 101-105.
- Yoshida N, Naito Y, Kugai M, Inoue K, Uchiyama K, et al. (2011) Efficacy of magnifying endoscopy with flexible spectral imaging color enhancement in the diagnosis of colorectal tumors. J Gastroenterol 46: 65-72.
- Ikematsu H, Matsuda T, Emura F, Saito Y, Uraoka T, et al. (2010) Efficacy of capillary pattern type IIIA/IIIB by magnifying narrow band imaging for estimating depth of invasion of early colorectal neoplasms. BMC Gastroenterol 10: 33.
- Tanaka S, Sano Y (2011) Aim to unify the narrow band imaging (NBI) magnifying classification for colorectal tumors: current status in Japan from a summary of the consensus symposium in the 79th Annual Meeting of the Japan Gastroenterological Endoscopy Society. Dig Endosc 23:131-139.
- Wada Y, Kashida H, Kudo SE, Misawa M, Ikehara N, et al. (2010) Diagnostic accuracy of pit pattern and vascular pattern analyses in colorectal lesions. Dig Endosc 22: 192-199.
- Japanese Society for Cancer of the Colon and Rectum (2010) General Rules for Clinical and Pathological Studies on Cancer of the Colon, Rectum, and Anus, 7th edn, Revised Version. Tokyo: Kanahara Shuppan.
- Tanaka S, Haruma K, Oh-E H, Nagata S, Hirota Y, et al. (2000) Conditions of curability after endoscopic resection for colorectal carcinoma with submucosally massive invasion. Oncol Rep 7: 783-788.
- Nakadoi K, Tanaka S, Kanao H, Terasaki M, Takata S, et al. (2012) Management of T1 colorectal carcinoma with special reference to criteria for curative endoscopic resection. J Gastroenterol Hepatol 27: 1057-1062.
- Santos CE, Malaman D, Pereira-Lima JC (2011) Endoscopic mucosal resection in colorectal lesion: a safe and effective procedure even in lesions larger than 2 cm and in carcinomas. Arq Gastroenterol 48: 242-247.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13972
- [From(publication date):
June-2014 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 9471
- PDF downloads : 4501