Endometrial Polyp Metastases from Invasive Ductal Carcinoma: A Rare Case Report and Review of the Only 24 Cases in the Literature
Received: 02-Nov-2023 / Manuscript No. roa-23-119871 / Editor assigned: 06-Nov-2023 / PreQC No. roa-23-119871 / Reviewed: 20-Nov-2023 / QC No. roa-23-119871 / Revised: 24-Nov-2023 / Manuscript No. roa-23-119871 / Published Date: 30-Nov-2023
Abstract
Metastatic recurrence is a significant problem in patients with breast cancer, the most frequently diagnosed malignancy and the second leading cause of cancer-related death among women worldwide. Although the incidence of distant relapse has reduced and improved survival rates, 20–30% of patients with early breast cancer still die of metastatic disease. Breast cancer (BC) rarely metastasizes to the female reproductive system and when it does, ovaries are more frequently affected than other sites. BC metastasis to the endometrium is extremely rare and origin from Invasive ductal carcinoma (IDC) with endometrial polyp metastases which is even more uncommon than Invasive lobular carcinoma (ILC). We present a rare case of endometrial polyp metastases from IDC and reviewed the only 25 cases in the literature so far.
Keywords
Breast cancer (BC); Invasive ductal carcinoma (IDC); Invasive lobular carcinoma (ILC); Gallium 68 labelled fibroblast activation protein inhibitor (Ga68 FAPI PET/CT)
Introduction
Breast cancer is the most common malignancy among women globally with an estimated incidence of 2.3 million new cases, accounting for 11.7% of all cancers in 2020. Epidemiological studies predict a spike of almost 2 million cases by 2030 and over 3 million cases by 2040. In India by 2020, BC accounted for 13.5% of all cancers and 10.6% of all cancer related deaths [1,2].
Invasive ductal cancer (IDC) is the most common breast cancer (75%) followed by Invasive lobular carcinoma (ILC) (10-15%). Gynecologic organ metastases are more common with ILC than with IDC. 6% have de novo metastases, and about 30% metastasize after months to years of treatment [3].
Breast cancer metastasizes most frequently to the lung, bone, liver, and brain and very rarely to the female genital tract. Most affected are the ovaries (75.8%), followed by the vagina (13.4%), uterine corpus (4.7%), cervix (3.4%), vulva (2%), and fallopian tubes (0.7%) [4]. Uterine metastases usually occur with ovarian metastases via a lymphatic route whereas isolated uterine metastases spread hematogenously [4]. In the uterus, myometrial involvement is the most common (63.5%), followed by the myometrium and endometrium together (32.7%) and only the endometrium (3.8 %). Even more infrequent are isolated endometrial polyp metastases, formerly reported as related to the use of tamoxifen [3].
In a PUBMED search and review of literature related to endometrial metastasis from Invasive ductal carcinoma published from 1990 to 2022, there are merely 24 cases of endometrial metastases from IDC and as per this search we present the 25th case of Invasive ductal carcinoma with isolated metastases to the endometrial polyp.
Case Report
A 59-year-old, middle eastern woman with complaints of painful left breast lump, fatigue, weight loss, low back ache, and lower abdominal pain. She has been menopausal for 10 years with no history of abnormal vaginal bleeding. Family history of breast cancer was positive in her sister. The patient is BRCA 2 positive. Physical examination revealed a firm, tender, mobile mass in the left breast in the upper outer
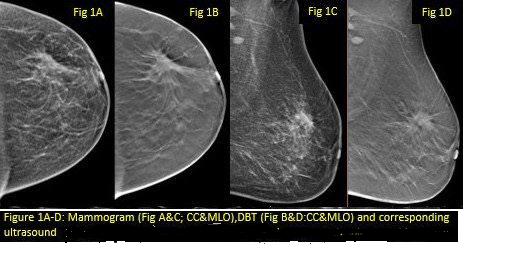
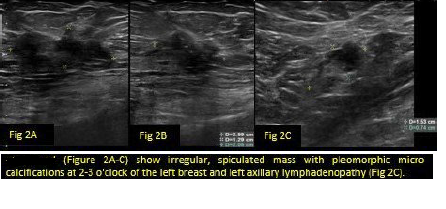
quadrant. The mammogram showed an irregular, spiculated mass with architectural distortion at the 2-3 o’clock with pleomorphic micro calcifications. No satellite nodules seen. No skin thickening/nipple retraction. The corresponding breast ultrasound revealed an irregular, hypoechoic mass measuring 2.9 x 1.3 x 2cm with increased vascularity; medial ductal extension, and mild perilesional edema; ACR BI-RADS 5: highly suggestive of malignancy. Histsopathological correlation was advised. Enlarged left level 1 axillary lymph nodes with loss of normal architecture were noted; the largest one measured 1.5 x 0.7cm suggestive of metastases (Figures 1 and 2).
Due to a strong family history and BRCA 2 positive status transvaginal ultrasound of the pelvis was performed which showed irregularly thickened, polypoidal growth arising from the endometrium measuring.
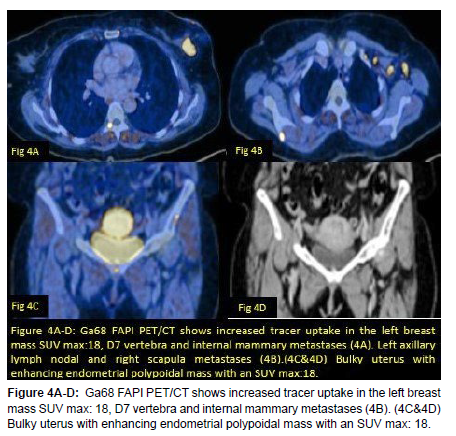
In view of BIRADS 5 on breast ultrasound and mammography and as per our institutional protocol patient was subjected to metastatic workup with Ga68 FAPI PET CT scan which showed a 2.5 x 2.2 x 2cm metabolically active irregular spiculated mass in the upper outer quadrant of left breast involving the nipple areolar complex (SUV max: 18). Metabolically active and enlarged level 1 and level 2 left axillary lymph nodes, largest one measuring 1.3 x 1.1 cm (SUV max: 33.6) and left internal mammary lymph node measuring 8 x 6mm (SUV max: 26). No evidence of contralateral breast mass. No hepatic or pulmonary metastases (Figure 3). The uterus appeared bulky, measured 8.9 x 4.9 x 5.7mm and showed metabolically active endometrial soft tissue thickening which was suspicious for malignancy, and MRI pelvis correlation was recommended for further evaluation. Also documented were metabolically active mixed lytic and sclerotic skeletal metastases involving the right scapula, cervical, thoracic and lumbar vertebrae, bilateral iliac bones and femur (SUV max: 41.5) (Figure 4).
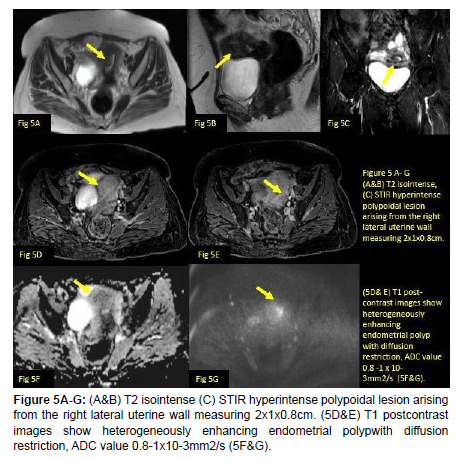
CE MRI of the pelvis (Figure 5A-G) showed a T2 isointense, STIR hyperintense and T1 post contrast enhancing endometrial polyp arising from the right lateral fundal wall with diffusion restriction and ADC values ranging between 0.8 x 10-3mm2/s to 1 x 10-3mm2/s. A core needle biopsy of breast mass revealed a mildly differentiated IDC, grade I and immunohistochemical (IHC) analysis demonstrated that the tumor was estrogen receptor (ER) positive, progesterone receptor (PR) weakly positive, and HER2 neu negative by fluorescence in situ hybridization (FISH) and Ki-67 10%. Luminal A subtype. Hysteroscopic polypectomy was performed, and a histopathological examination revealed endometrial metastases from a breast primary. On gross examination, the endometrial cavity was filled by a tan-pink polypoidal mass measuring 2x1x0.8cm. Microscopic examination demonstrated a poorly differentiated metastatic carcinoma in the endometrium consistent with breast primary. Tumor cells were positive for GATA 3 and Pan CK suggestive of mammary origin and not endometrial origin.
The patient received chemotherapy and fortunately completed the first 8 sessions with reluctance for surgical management of the breast lesion.
Discussion
The female genital organs are rare sites of metastases. Interestingly ovaries are the most common site among them (78.5%) because they are extremely vascular organs, have good lymphatic drainage, with appropriate metabolic factors, pH, and partial pressure of oxygen making it a suitable environment for the cancer cells to thrive. On the other hand, the uterus accounts for only 4.7% of the metastases likely because it contains more fibrous tissue, which is not conducive to the colonization and growth of tumor cells [5]. Endometrial metastasis accounting for a few numbers of cases so far is frequently associated with ovarian metastases and is spread via the lymphatics, whereas isolated endometrial polyp metastases are even more unusual and possibly hematogenous in route [6].
Kumar et al studied 63 cases of uterine metastases from a variety of extra-genital cancers. Breast cancer accounted for approximately 43% of these cases, followed by colon cancer (18%), stomach cancer (11%), and pancreatic cancer (11%) [7].
A study by Mazur et al analyzed 52 cases of metastases to the female genital tract. Of these, 46 cases involved metastases to the ovaries, and only two cases had isolated endometrial involvement [8].
Metastases to the endometrium from breast cancer account for 34% of cases after gastrointestinal cancer (37%) [9]. Rahmani et al in 2018 documented endometrium as a rare site for metastases from a breast primary (4%), with increasing rarity from IDC (24 cases so far). Metastatic potential is higher for invasive lobular carcinoma (ILC) (80%) than invasive ductal carcinoma (IDC). Although the lung, liver, bone, and brain are common sites of metastasis in both IDC and ILC, ILCs exhibit organotropism and cellular tropism favoring the gastrointestinal system, gynecologic organs, peritoneumretroperitoneum, adrenal glands, and bone marrow more than IDC [9].We presented a case of invasive ductal carcinoma with asymptomatic, endometrial polyp metastases which remains a rarity.
After conducting a literature search using the following terms: “breast carcinoma with endometrial metastases”, “invasive ductal carcinoma”, “endometrial polyp metastases” and “uterine metastases”. 24 cases of endometrial metastases from invasive ductal carcinoma were found between 1990 and 2022.
18/25 were ER-positive, 3/25 were ER-negative and 4/25 cases with unknown ER status. 15/25 was PR positive, 5/25 were PR negative, and 5/25 cases with unknown PR status. Only one case was HER2 neu positive, 13/25 was HER2 neu negative and in 11/25 cases the HER2 neu status was unknown.
The most common molecular subtype was ER, PR positive, HER 2neu negative (luminal subtype) accounting for 56% of cases (14/25). Only 3/25 were ER, PR, and HER2 neu negative (TNBC) in the literature so far, one case was ER, PR, and HER2 neu positive (TPBC) and one case were ER positive, PR, and HER2neu negative. The remaining 6 cases did not have adequate IHC data. Our case was ER, PR positive, and HER2 neu negative with KI 67 10% (Luminal A subtype).
Razia et al described 17 cases of breast cancer with metastases to endometrial polyps, eight of the lobular subtype, seven of the ductal subtype, one apocrine, and one mixed (lobular and ductal). Of these patients, 12 had vaginal bleeding as a symptom. Vaginal bleeding is the most common symptom reported in women with a tumor that affects the endometrium [10]. Our patient was asymptomatic.
A comprehensive review done by Ayesha et al from 1984 to 2017, reported 23 cases of endometrial metastases from breast cancer, 13 from ILC, nine from IDC, one apocrine, one Metaplastic, and one mixed.
Most recent review by Anne-Sophie et al in 2021 found 44 cases of uterine metastases from breast carcinoma between 2000 and 2018. Out of which 18 cases were of Invasive ductal carcinoma metastasizing to the endometrium.
A literature review performed by Huo et al. from 1984 to 2015 identified 13 cases of breast metastasis to the endometrium between 1984 and 2015, demonstrating that ER/PR-positive tumors, especially from lobular type (ILC), were more likely to result in endometrial metastasis in comparison to IDC [5,6]. Most of these uterine metastases were detected in known cases of breast cancer patients during their follow-up and hormone therapy period.
Aisha Akhtar et al identified 23 cases of uterine metastases, nine were ductal and 13 were lobular. The remaining three were mixed, apocrine, and metaplastic. Fifteen were ER-positive, 13 were PR positive, and eight cases were Her2-negative. Most patients with uterine metastases were positive for hormone receptors. It is unclear whether there is a relation between hormone-positive status and risk of uterine metastases.
Rahmani et al stated, there have been only 5 reported cases of endometrial metastases with IDC origin. Among them, 1 case was ER/ PR-positive, 2 cases were only ER-positive and the other 2 were ER/PRnegative. All 4 Her-2/neu receptors were negative [9].
Only 3 cases of triple-negative breast cancer metastasizing to the endometrium have been reported in the literature so far [6].
Endometrial metastases from breast cancer tend to occur synchronously with multi-organ metastases, like in our case the patient presented with lymph nodal metastases, endometrial polyp metastases, and skeletal metastases.
Our review noted that most patients were above the age of 50 years (17/25). The endometrium was the only metastatic site in 36% of cases (9/25) out of which endometrial polyp metastases were noted in only 5 cases (as seen in our case).
The peak time of recurrence in these 25 cases was between 1 and 12 years. Most patients underwent total abdominal hysterectomy with oophorectomy along with chemotherapy.
Endometrial polyp metastases have been reported primarily related to the use of tamoxifen as it is one of the most used chemotherapeutic agents in breast cancer. Along with the antiestrogenic effect, tamoxifen has a small agonist effect leading to an increased risk of endometrial hyperplasia, polyps, and malignant transformation in 2.7% of cases. Hence primary endometrial cancer is an important differential diagnosis in patients with abnormal vaginal bleeding and on tamoxifen therapy. Our patient did not have abnormal vaginal bleeding nor was she on Tamoxifen as both primary and metastatic diseases were brought to light during the same course of time.
It is vital to differentiate between endometrial metastases from breast cancer and primary endometrial carcinoma, as both are hormone receptor positive. Immunohistochemical markers such as GATA3, Pan CK, mammaglobin, and GCDFP15 for breast origin and PAX8 for endometrial origin are employed to indicate the primary origin of cancer [3]. Our patient tested positive for PanCK with diffuse and strong nuclear GATA3 immunoreactivity in the tumor, indicating metastases from a breast primary. Our review also revealed GATA3 was performed in 9 cases and was positive for all 9 cases including ours. A study with 57 cases of endometrial metastasis from breast cancer showed that the GATA3 marker had the highest expression rate (82% of cases), showing good sensitivity to identify endometrial metastasis with greater sensitivity than the mammaglobin. Also, primary endometrial cancer may be curable with surgery, whereas metastatic disease to the uterus has only systemic treatment options with an overall poor prognosis [3].
Conclusion
We report the 25th case of ductal carcinoma metastasizing to the endometrial polyp. Isolated endometrial metastases from breast cancer are extremely rare and can pose a significant diagnostic and therapeutic challenge. Metastases to the endometrium from extrauterine malignancies usually indicate disseminated disease and a poor prognosis. The accurate diagnosis of metastases is therefore essential to ensure proper management.
References
- Riggio AI, Varley KE, Welm AL (2021) The lingering mysteries of metastatic recurrence in breast cancer. Br J Cancer 124: 13-26.
- Mehrotra R, Yadav K (2022) Breast cancer in India: Present scenario and the challenges ahead. World J Clin Oncol 13: 209.
- Çift T, Aslan B, Bulut B, İlvan Ş (2016) Unusual uterine metastasis of invasive ductal carcinoma: A case report. Turk J Obstet Gynecol 13: 164.
- Kong D, Dong X, Qin P, Sun D, Zhang Z, et al. (2022) Asymptomatic uterine metastasis of breast cancer: Case report and literature review. Medicine 10: 101.
- Choi S, Joo JW, Do SI, Kim HS (2020) Endometrium-limited metastasis of extragenital malignancies: A challenge in the diagnosis of endometrial curettage specimens. Diagnostics 10: 150
- Kumar NB, Hart WR (1982) Metastases to the uterine corpus from extragenital cancers. A clinic pathologic study of 63 cases. Cancer 50: 2163-2169.
- Mazur MT, Hsueh S, Gersell DJ (1984) Metastases to the female genital tract: analysis of 325 cases. Cancer 53: 1978-1984.
- Rahmani M, Nili F, Tabibian E (2018) Endometrial metastasis from ductal breast carcinoma: a case report with literature review. Am J Case Rep 19: 494.
- Razia S, Nakayama K, Tsukao M (2017) Metastasis of breast cancer to an endometrial polyp, the cervix, and a leiomyoma: A case report and review of the literature. Oncol Lett 14: 4585-4592.
- Akhtar A, Ratra A, Puckett Y, Sheikh AB, Ronaghan CA (2017) Synchronous uterine metastases from breast cancer: case study and literature review. Cureus 13: 9.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Zohra F (2023) Endometrial Polyp Metastases from Invasive DuctalCarcinoma: A Rare Case Report and Review of the Only 24 Cases in the Literature.OMICS J Radiol 12: 509.
Copyright: © 2023 Zohra F. This is an open-access article distributed under theterms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 1595
- [From(publication date): 0-2023 - Dec 13, 2025]
- Breakdown by view type
- HTML page views: 1270
- PDF downloads: 325